The Impact of Telemedicine on Healthcare Accessibility and Equity
Telemedicine, the use of technology to provide remote healthcare services, has been gaining popularity in recent years. With the advancement of technology and the increasing demand for accessible healthcare, telemedicine has become a viable solution for many patients. However, one of the most significant impacts of telemedicine is its potential to improve healthcare accessibility and equity.
In today’s fast-paced world, access to healthcare is a major concern for many individuals. Long wait times, limited availability of healthcare providers, and geographical barriers can make it challenging for people to receive timely and quality care. This is where telemedicine comes in. By utilizing technology, telemedicine allows patients to connect with healthcare providers remotely, eliminating the need for in-person visits. This not only saves time but also reduces the burden on the healthcare system, making it more accessible for those in need.
One of the main advantages of telemedicine is its ability to bridge the gap between rural and urban healthcare. In many rural areas, access to healthcare is limited due to a shortage of healthcare providers and facilities. This often results in patients having to travel long distances to receive care, which can be both time-consuming and expensive. With telemedicine, patients in rural areas can connect with healthcare providers in urban areas, eliminating the need for travel. This not only saves time and money but also ensures that patients in remote areas have access to the same quality of care as those in urban areas.
Moreover, telemedicine also has the potential to improve healthcare equity. In many underserved communities, access to healthcare is a major issue. This can be due to various factors such as socioeconomic status, language barriers, or lack of transportation. Telemedicine can help bridge these gaps by providing remote healthcare services that are accessible to all, regardless of their location or background. This can significantly improve the health outcomes of underserved populations and promote healthcare equity.
Another significant impact of telemedicine on healthcare accessibility is its ability to reach patients with chronic conditions. Patients with chronic illnesses often require frequent check-ups and monitoring, which can be challenging for those who live far from healthcare facilities. With telemedicine, these patients can connect with their healthcare providers remotely, allowing for more frequent and convenient check-ups. This not only improves the management of chronic conditions but also reduces the need for hospital visits, making healthcare more accessible for these patients.
Furthermore, telemedicine has the potential to improve healthcare accessibility for individuals with disabilities. For those with mobility issues, traveling to a healthcare facility can be a daunting task. Telemedicine eliminates the need for physical travel, allowing these individuals to receive care from the comfort of their homes. This not only saves time and effort but also ensures that individuals with disabilities have equal access to healthcare services.
However, despite its potential to improve healthcare accessibility and equity, telemedicine also has its limitations. One of the main concerns is the lack of access to technology for some individuals, particularly those in underserved communities. To fully realize the benefits of telemedicine, it is crucial to address this issue and ensure that everyone has access to the necessary technology.
In conclusion, telemedicine has the potential to revolutionize healthcare accessibility and equity. By utilizing technology, it can bridge the gap between rural and urban healthcare, improve healthcare equity, and reach patients with chronic conditions and disabilities. However, it is essential to address the issue of technology access to ensure that telemedicine can benefit all individuals, regardless of their location or background. With continued advancements in technology and a focus on addressing barriers, the future of telemedicine and remote patient monitoring looks promising in improving healthcare accessibility and equity.
Advancements in Remote Patient Monitoring Technology and its Potential for Chronic Disease Management
The healthcare industry has been rapidly evolving in recent years, with advancements in technology playing a major role in this transformation. One area that has seen significant growth and potential is telemedicine and remote patient monitoring. With the rise of chronic diseases and an aging population, the need for efficient and effective management of these conditions has become more pressing. This is where remote patient monitoring technology comes into play, offering a promising solution for chronic disease management.
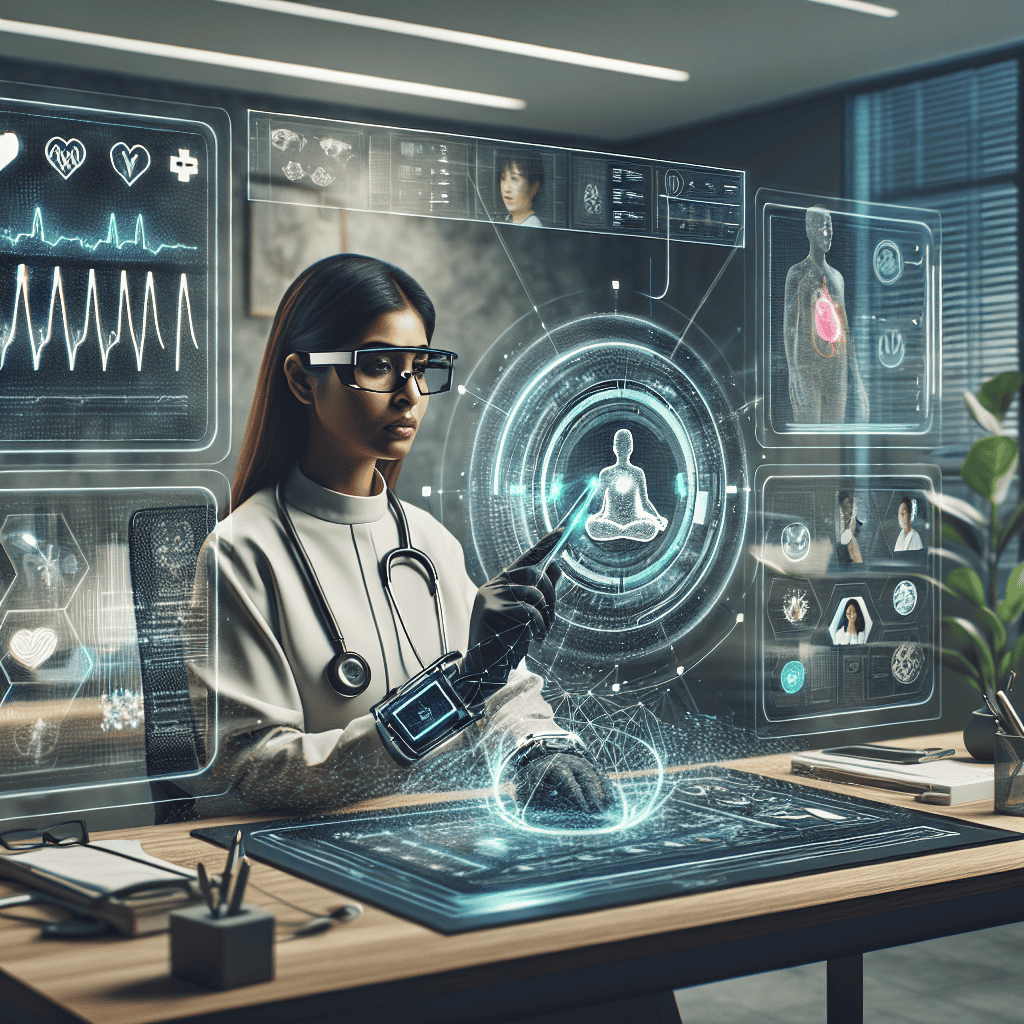
Remote patient monitoring (RPM) involves the use of technology to collect and transmit patient data from a distance. This data can include vital signs, medication adherence, and other health-related information. RPM technology has been around for some time, but recent advancements have made it more accessible and user-friendly, paving the way for its potential in chronic disease management.
One of the key advancements in RPM technology is the development of wearable devices. These devices, such as smartwatches and fitness trackers, can collect and transmit real-time data on a patient’s vital signs, activity levels, and sleep patterns. This data can then be monitored by healthcare professionals remotely, allowing for early detection of any changes or abnormalities. This is especially beneficial for patients with chronic diseases, as it allows for continuous monitoring without the need for frequent in-person visits.
Another significant advancement in RPM technology is the use of artificial intelligence (AI) and machine learning. These technologies can analyze large amounts of patient data and identify patterns and trends that may not be apparent to human healthcare providers. This can help in predicting potential health issues and providing personalized treatment plans for patients. AI and machine learning can also assist in identifying patients who may be at risk for developing chronic diseases, allowing for early intervention and prevention.
The integration of telemedicine and RPM technology has also opened up new possibilities for remote consultations and virtual care. Patients can now connect with their healthcare providers through video conferencing, allowing for remote diagnosis and treatment. This is particularly beneficial for patients with chronic diseases who may have difficulty traveling to in-person appointments. Virtual care also offers convenience and cost savings for both patients and healthcare providers.
One of the most promising aspects of RPM technology is its potential for chronic disease management. Chronic diseases, such as diabetes, heart disease, and hypertension, require continuous monitoring and management to prevent complications and improve outcomes. RPM technology allows for real-time monitoring of vital signs and other health data, providing healthcare providers with a more comprehensive view of a patient’s health. This can lead to early detection of any changes or issues, allowing for timely interventions and adjustments to treatment plans.
Moreover, RPM technology can also improve patient engagement and self-management. With the use of wearable devices and mobile apps, patients can track their own health data and receive personalized feedback and recommendations. This empowers patients to take an active role in managing their chronic conditions, leading to better outcomes and a higher quality of life.
In conclusion, advancements in remote patient monitoring technology have the potential to revolutionize chronic disease management. With the use of wearable devices, AI, and telemedicine, healthcare providers can now monitor and treat patients remotely, leading to improved outcomes and cost savings. As technology continues to advance, the future of telemedicine and remote patient monitoring looks bright, offering a promising solution for the growing burden of chronic diseases.
The Role of Telemedicine in Disaster Response and Emergency Care
Telemedicine, the use of technology to provide remote medical care, has been gaining popularity in recent years. With advancements in technology and the increasing demand for convenient and accessible healthcare, telemedicine has become a valuable tool in disaster response and emergency care.
During natural disasters, such as hurricanes, earthquakes, or wildfires, traditional healthcare facilities may become inaccessible or overwhelmed. This is where telemedicine plays a crucial role in providing medical care to those in need. With the use of telecommunication technology, healthcare providers can remotely assess and treat patients, even in the most challenging situations.
One of the main advantages of telemedicine in disaster response is its ability to bridge the gap between patients and healthcare providers. In areas where traditional healthcare facilities are damaged or destroyed, telemedicine can connect patients with medical professionals who are located in safe and functioning facilities. This not only ensures that patients receive timely and appropriate care but also relieves the burden on local healthcare systems.
Moreover, telemedicine can also be used to provide medical care to individuals who are unable to reach a healthcare facility due to road closures or other barriers. In these situations, telemedicine can be a lifesaver, as it allows patients to receive medical attention without having to physically travel to a healthcare facility.
In addition to disaster response, telemedicine also plays a crucial role in emergency care. In emergency situations, every second counts, and telemedicine can help save precious time. For instance, in cases of stroke or heart attack, where immediate medical attention is critical, telemedicine can enable healthcare providers to remotely assess the patient’s condition and provide necessary treatment recommendations. This can significantly improve the chances of survival and reduce the risk of long-term complications.
Furthermore, telemedicine can also be used to monitor patients with chronic conditions, such as diabetes or heart disease, in emergency situations. By remotely monitoring these patients, healthcare providers can detect any changes in their condition and intervene before it becomes a medical emergency. This not only improves patient outcomes but also reduces the need for emergency room visits, which can be costly and time-consuming.
Another significant advantage of telemedicine in emergency care is its ability to provide medical care in remote or underserved areas. In many rural or low-income communities, access to healthcare is limited, and emergency care may not be readily available. Telemedicine can bridge this gap by connecting patients with healthcare providers who are located in other areas. This not only improves access to emergency care but also reduces healthcare disparities.
Moreover, telemedicine can also be used to provide mental health support in emergency situations. Natural disasters and other emergencies can have a significant impact on individuals’ mental health, and telemedicine can provide access to mental health professionals for those in need. This can be especially beneficial for individuals who may not have access to mental health services in their local area.
In conclusion, telemedicine has a crucial role to play in disaster response and emergency care. Its ability to bridge the gap between patients and healthcare providers, provide timely medical care, and improve access to healthcare in remote or underserved areas makes it an invaluable tool in emergency situations. As technology continues to advance, the future of telemedicine in disaster response and emergency care looks promising, and it is likely to become an essential component of the healthcare system.