-
Table of Contents
- Precision Oncology: A New Era in Cancer Treatment
- 1. The Foundations of Precision Oncology
- 1.1 The Role of Genomics in Precision Oncology
- 1.2 The Importance of Biomarkers
- 1.3 From Traditional to Personalized Treatment Paradigms
- 2. Technological Advancements in Precision Oncology
- 2.1 Liquid Biopsies: A Non-Invasive Diagnostic Tool
- 2.2 Artificial Intelligence in Cancer Treatment
- 2.3 CRISPR Gene Editing: A New Frontier in Cancer Therapy
- 3. Clinical Applications of Precision Oncology
- 3.1 Targeted Therapies: Precision Medicine in Action
Precision Oncology: A New Era in Cancer Treatment
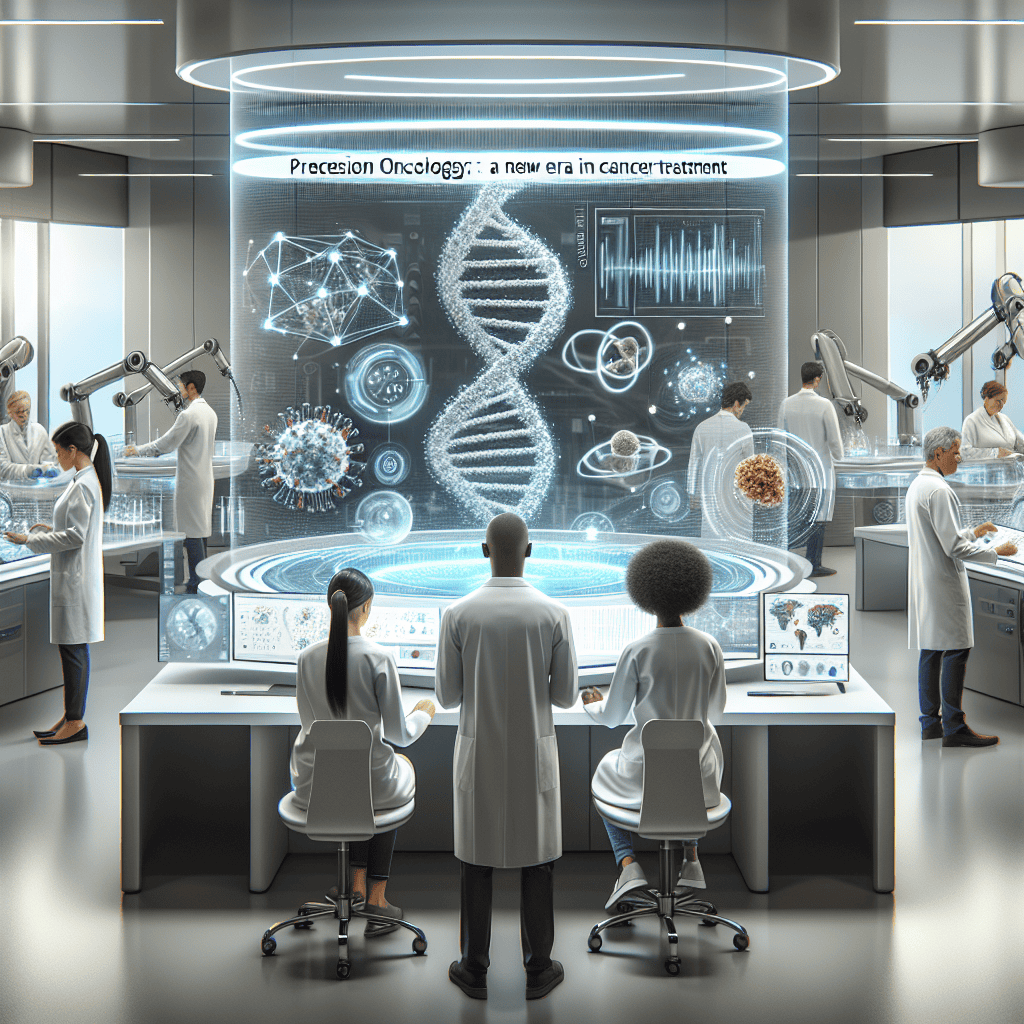
In recent years, the field of oncology has witnessed a paradigm shift with the advent of precision oncology. This innovative approach to cancer treatment tailors medical care to the individual characteristics of each patient, including their genetic makeup and the specific genetic profile of their tumor. Precision oncology promises to improve outcomes by targeting therapies more effectively and minimizing unnecessary side effects. This article delves into the intricacies of precision oncology, exploring its foundations, technological advancements, clinical applications, challenges, and future prospects.
1. The Foundations of Precision Oncology
Precision oncology is rooted in the understanding that cancer is not a single disease but a collection of related diseases, each with its own genetic and molecular characteristics. This section explores the foundational principles that underpin precision oncology, including the role of genomics, the importance of biomarkers, and the shift from traditional to personalized treatment paradigms.
1.1 The Role of Genomics in Precision Oncology
Genomics plays a pivotal role in precision oncology by providing insights into the genetic alterations that drive cancer. The Human Genome Project, completed in 2003, laid the groundwork for understanding the genetic basis of diseases, including cancer. By sequencing the DNA of cancer cells, researchers can identify mutations and alterations that contribute to tumor growth and progression.
One of the key breakthroughs in genomics is the ability to perform next-generation sequencing (NGS), which allows for the rapid and comprehensive analysis of a patient’s genome. NGS has enabled the identification of actionable mutations, which are genetic changes that can be targeted with specific therapies. For example, mutations in the EGFR gene in non-small cell lung cancer can be targeted with tyrosine kinase inhibitors, leading to improved patient outcomes.
1.2 The Importance of Biomarkers
Biomarkers are biological molecules that indicate the presence or progression of a disease. In precision oncology, biomarkers are used to identify patients who are likely to benefit from specific treatments. These biomarkers can be genetic, such as mutations in the BRCA1 and BRCA2 genes in breast cancer, or protein-based, such as the overexpression of HER2 in certain breast cancers.
The identification of biomarkers has revolutionized cancer treatment by enabling the development of targeted therapies. For instance, the discovery of the BCR-ABL fusion gene in chronic myeloid leukemia led to the development of imatinib, a targeted therapy that has significantly improved survival rates. Biomarkers also play a crucial role in monitoring treatment response and detecting resistance, allowing for timely adjustments in therapy.
1.3 From Traditional to Personalized Treatment Paradigms
Traditional cancer treatments, such as chemotherapy and radiation, often have a one-size-fits-all approach, targeting rapidly dividing cells without distinguishing between healthy and cancerous cells. This can lead to significant side effects and variable treatment responses. Precision oncology shifts the focus from treating cancer based on its location in the body to treating it based on its unique genetic and molecular characteristics.
Personalized treatment paradigms involve tailoring therapies to the individual patient, taking into account their genetic profile, lifestyle, and preferences. This approach not only improves treatment efficacy but also enhances the patient’s quality of life by reducing unnecessary side effects. Personalized treatment plans are developed through a multidisciplinary approach, involving oncologists, geneticists, pathologists, and other specialists.
2. Technological Advancements in Precision Oncology
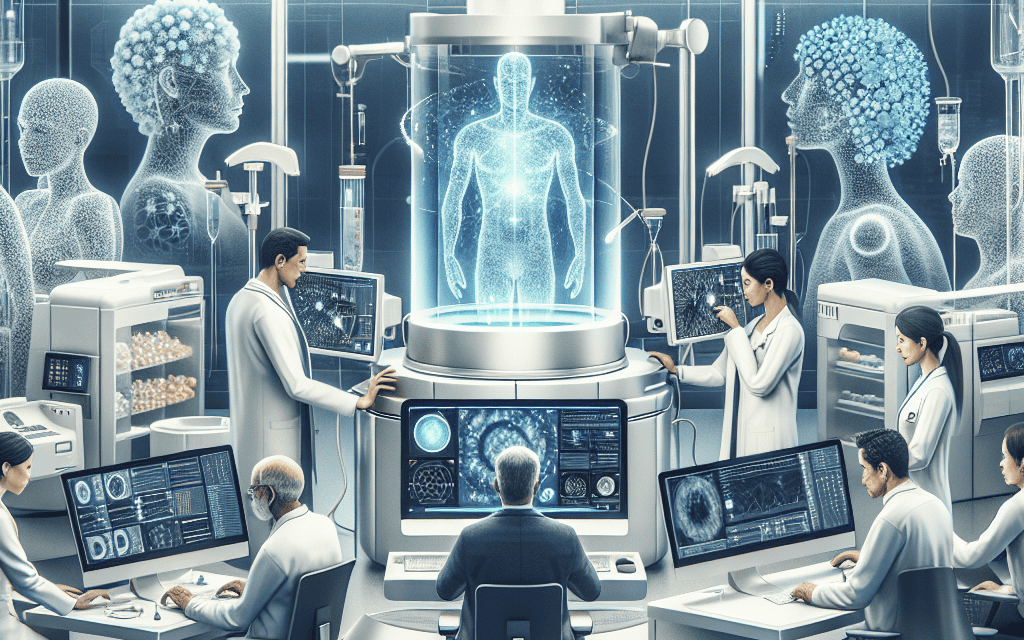
The rapid advancement of technology has been a driving force behind the evolution of precision oncology. This section examines the cutting-edge technologies that are transforming cancer diagnosis and treatment, including liquid biopsies, artificial intelligence, and CRISPR gene editing.
2.1 Liquid Biopsies: A Non-Invasive Diagnostic Tool
Liquid biopsies represent a significant advancement in cancer diagnostics, offering a non-invasive alternative to traditional tissue biopsies. By analyzing circulating tumor DNA (ctDNA) in a patient’s blood, liquid biopsies can detect genetic mutations and monitor tumor dynamics in real-time.
One of the key advantages of liquid biopsies is their ability to provide a comprehensive view of tumor heterogeneity, capturing genetic alterations from multiple tumor sites. This is particularly important in metastatic cancers, where different tumor sites may harbor distinct mutations. Liquid biopsies also enable early detection of treatment resistance, allowing for timely adjustments in therapy.
Several studies have demonstrated the clinical utility of liquid biopsies. For example, a study published in Nature Medicine showed that liquid biopsies could detect EGFR mutations in non-small cell lung cancer patients with high accuracy, guiding the selection of targeted therapies. As technology continues to advance, liquid biopsies are expected to become an integral part of precision oncology.
2.2 Artificial Intelligence in Cancer Treatment
Artificial intelligence (AI) is revolutionizing precision oncology by enhancing the analysis of complex datasets and improving decision-making processes. AI algorithms can analyze genomic data, medical images, and clinical records to identify patterns and predict treatment outcomes.
One of the key applications of AI in precision oncology is in the development of predictive models for treatment response. By analyzing large datasets, AI can identify biomarkers and genetic signatures associated with positive treatment outcomes. This information can be used to stratify patients and guide treatment selection.
AI is also being used to improve the accuracy of cancer diagnosis. For instance, deep learning algorithms have been developed to analyze pathology slides and identify cancerous cells with high precision. These algorithms can assist pathologists in making more accurate diagnoses and reduce the risk of human error.
2.3 CRISPR Gene Editing: A New Frontier in Cancer Therapy
CRISPR-Cas9 gene editing technology has opened new avenues for cancer treatment by enabling precise modifications of the genome. This technology allows researchers to target and edit specific genes involved in cancer development and progression.
One of the most promising applications of CRISPR in precision oncology is the development of gene therapies that target cancer-specific mutations. For example, researchers have used CRISPR to correct mutations in the KRAS gene, which is commonly mutated in pancreatic and colorectal cancers. By targeting these mutations, CRISPR-based therapies have the potential to halt tumor growth and improve patient outcomes.
CRISPR is also being used to enhance the efficacy of existing cancer therapies. For instance, researchers are exploring the use of CRISPR to modify immune cells, such as T cells, to enhance their ability to recognize and attack cancer cells. This approach, known as CRISPR-enhanced CAR-T cell therapy, has shown promising results in preclinical studies.
3. Clinical Applications of Precision Oncology
Precision oncology is transforming clinical practice by enabling more effective and personalized cancer treatments. This section explores the clinical applications of precision oncology, including targeted therapies, immunotherapy, and combination treatments.
3.1 Targeted Therapies: Precision Medicine in Action
Targeted therapies are a cornerstone of precision oncology, designed to specifically target the molecular alterations driving cancer growth.