Understanding Chronic Back Pain: An In-Depth Guide
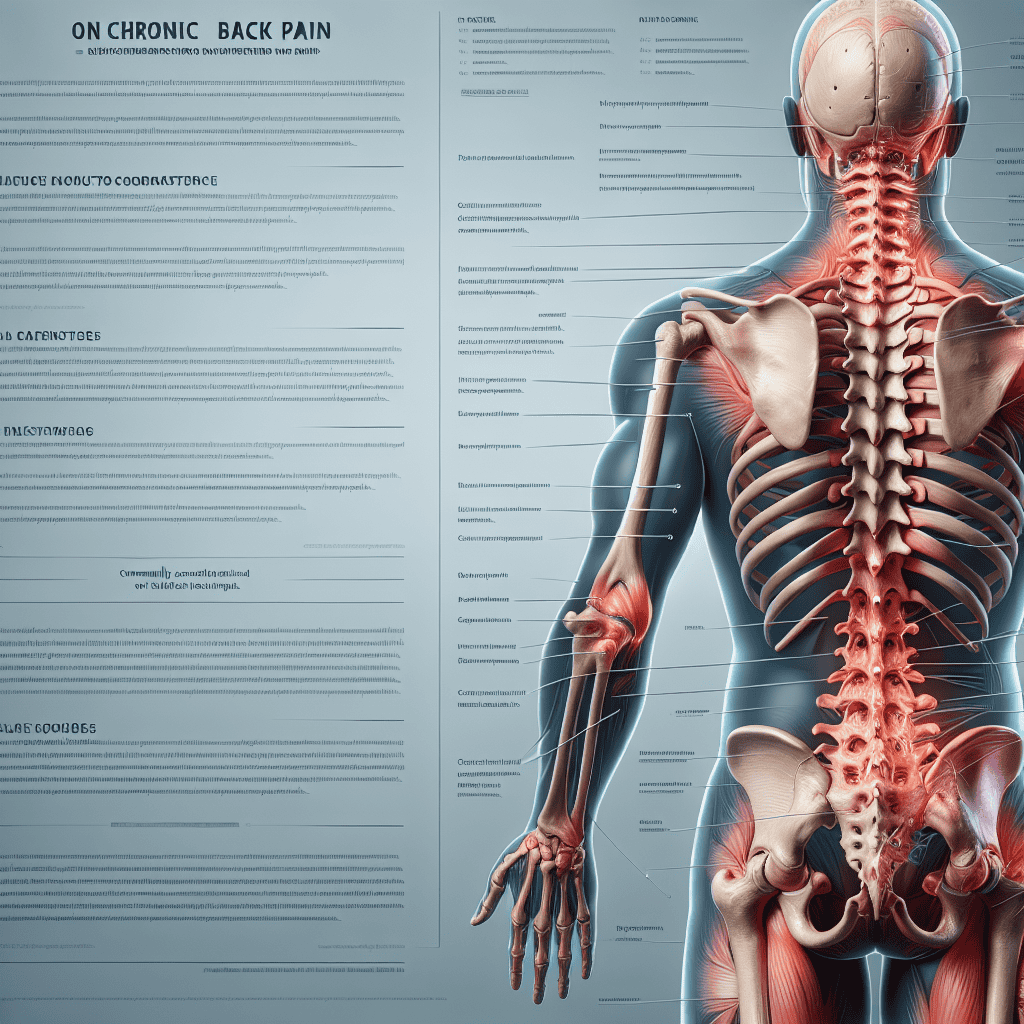
Chronic back pain is a pervasive issue affecting millions of people worldwide. It is a complex condition that can significantly impact an individual’s quality of life, leading to physical limitations, emotional distress, and financial burdens. This comprehensive guide aims to provide a detailed understanding of chronic back pain, exploring its causes, symptoms, diagnosis, treatment options, and prevention strategies. By delving into these aspects, we hope to offer valuable insights and practical advice for those affected by this debilitating condition.
1. Causes of Chronic Back Pain
Chronic back pain can arise from a multitude of factors, each contributing to the persistence and severity of the condition. Understanding these causes is crucial for effective management and treatment.
1.1 Musculoskeletal Disorders
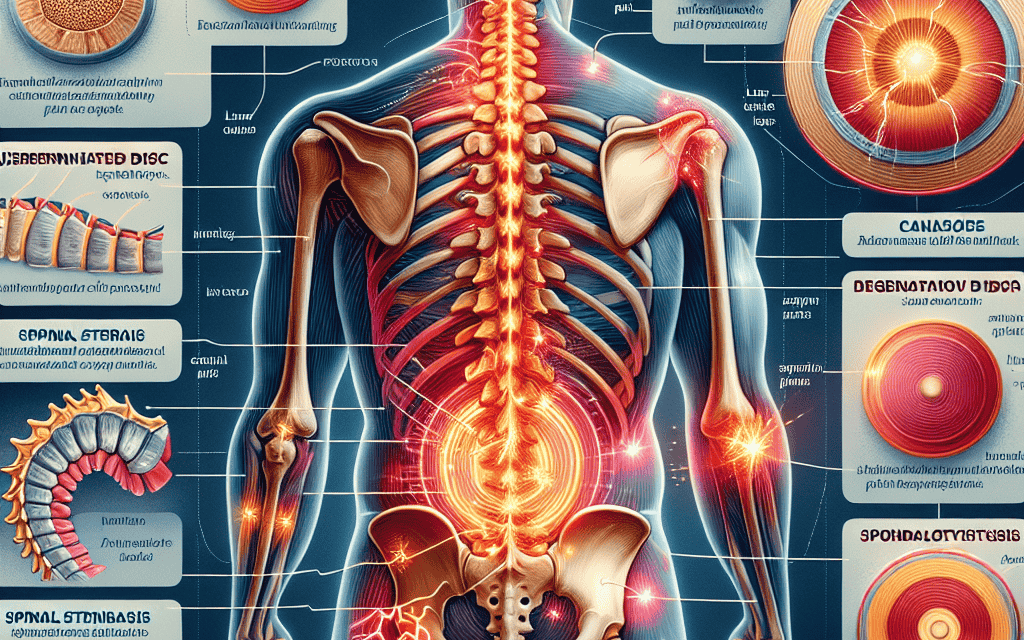
Musculoskeletal disorders are among the most common causes of chronic back pain. These include conditions such as:
- Herniated Discs: When the soft material inside a spinal disc pushes through a crack in the tougher exterior, it can irritate nearby nerves, leading to pain.
- Degenerative Disc Disease: As people age, the spinal discs can lose hydration and elasticity, resulting in pain and discomfort.
- Spinal Stenosis: This condition involves the narrowing of the spinal canal, which can put pressure on the spinal cord and nerves.
These disorders often result from wear and tear, injuries, or genetic predispositions. For instance, a study published in the journal Spine found that individuals with a family history of back problems are more likely to develop similar issues.
1.2 Lifestyle Factors
Lifestyle choices can significantly influence the development and progression of chronic back pain. Key factors include:
- Poor Posture: Sitting or standing with improper alignment can strain the back muscles and spine.
- Lack of Exercise: A sedentary lifestyle can weaken the muscles that support the spine, increasing the risk of pain.
- Obesity: Excess body weight can place additional stress on the spine, exacerbating pain.
Research indicates that individuals who engage in regular physical activity and maintain a healthy weight are less likely to experience chronic back pain. A study in the Journal of Physical Activity and Health highlighted the protective effects of exercise against back pain.
1.3 Psychological Factors
Psychological factors can also play a significant role in chronic back pain. Conditions such as depression, anxiety, and stress can exacerbate pain perception and hinder recovery. The relationship between mental health and chronic pain is well-documented, with studies showing that individuals with chronic pain are more likely to experience psychological distress.
For example, a study published in Pain found that patients with chronic back pain who also suffered from depression reported higher pain intensity and greater disability than those without depression.
1.4 Occupational Hazards
Certain occupations are associated with a higher risk of developing chronic back pain due to repetitive movements, heavy lifting, or prolonged periods of sitting or standing. Jobs in construction, nursing, and office work are particularly prone to back-related issues.
Employers and employees can mitigate these risks by implementing ergonomic solutions and promoting safe work practices. The Occupational Safety and Health Administration (OSHA) provides guidelines to help reduce workplace-related back injuries.
1.5 Medical Conditions
Several medical conditions can contribute to chronic back pain, including:
- Arthritis: Inflammatory conditions like osteoarthritis and rheumatoid arthritis can affect the spine, leading to pain and stiffness.
- Fibromyalgia: This chronic disorder is characterized by widespread musculoskeletal pain, including back pain.
- Scoliosis: An abnormal curvature of the spine that can cause discomfort and pain.
Understanding the underlying medical conditions is essential for developing an effective treatment plan. A comprehensive evaluation by a healthcare professional can help identify these contributing factors.
2. Symptoms and Diagnosis of Chronic Back Pain
Recognizing the symptoms of chronic back pain and obtaining an accurate diagnosis are critical steps in managing the condition effectively. This section explores the common symptoms and diagnostic approaches used by healthcare professionals.
2.1 Common Symptoms
Chronic back pain can manifest in various ways, with symptoms ranging from mild discomfort to severe, debilitating pain. Common symptoms include:
- Persistent Pain: Pain that lasts for more than three months and does not improve with rest or standard treatments.
- Stiffness: Reduced flexibility and difficulty moving the back.
- Muscle Spasms: Involuntary contractions of the back muscles, often causing sharp pain.
- Numbness or Tingling: Sensations that may radiate down the legs, indicating nerve involvement.
These symptoms can vary in intensity and may be influenced by factors such as activity level, posture, and stress. It is essential to monitor these symptoms and seek medical attention if they persist or worsen.
2.2 Diagnostic Approaches
Diagnosing chronic back pain involves a comprehensive evaluation by a healthcare professional. The diagnostic process typically includes:
- Medical History: A detailed review of the patient’s medical history, including previous injuries, surgeries, and family history of back problems.
- Physical Examination: An assessment of the patient’s posture, range of motion, and areas of tenderness or pain.
- Imaging Tests: X-rays, MRI, or CT scans may be used to visualize the spine and identify structural abnormalities.
- Nerve Tests: Electromyography (EMG) and nerve conduction studies can help assess nerve function and identify nerve-related issues.
These diagnostic tools enable healthcare providers to pinpoint the underlying causes of chronic back pain and develop a tailored treatment plan.
2.3 Case Studies
Case studies provide valuable insights into the diagnostic process and highlight the complexity of chronic back pain. Consider the following example:
A 45-year-old woman presented with persistent lower back pain that radiated down her left leg. Despite trying various over-the-counter pain medications and physical therapy, her symptoms persisted. An MRI revealed a herniated disc pressing on the sciatic nerve, confirming the diagnosis of sciatica. With this information, her healthcare provider recommended a combination of physical therapy, medication, and lifestyle modifications to manage her condition effectively.
This case illustrates the importance of thorough diagnostic evaluations in identifying the root cause of chronic back pain and guiding treatment decisions.
2.4 The Role of Pain Assessment Tools
Pain assessment tools are essential for evaluating the severity and impact of chronic back pain. These tools help healthcare providers understand the patient’s pain experience and monitor treatment progress. Commonly used pain assessment tools include:
- Visual Analog Scale (VAS): A simple scale that allows patients to rate their pain intensity on a continuum from “no pain” to “worst pain imaginable.”
- Numeric Rating Scale (NRS): Patients rate their pain on a scale from 0 to 10, with 0 representing no pain and 10 representing the worst possible pain.
- Oswestry Disability Index (ODI): A questionnaire that assesses the impact of back pain on daily activities and quality of life.
These tools provide valuable data for tailoring treatment plans and evaluating the effectiveness of interventions.
2.5 Challenges in Diagnosis
Diagnosing chronic back pain can be challenging due to its multifactorial nature and the overlap of symptoms with other conditions. Some common challenges include:
- Non-Specific Symptoms: Back pain symptoms can be vague and may not point to a specific underlying cause.
- Psychosocial Factors: Psychological and social factors can influence pain perception and complicate diagnosis.
- Comorbid Conditions: The presence of other medical conditions can obscure the primary cause of back pain.
Despite these challenges, a thorough and systematic approach to diagnosis can help healthcare providers identify the root causes of chronic back pain and develop effective treatment strategies.
3. Treatment Options for Chronic Back Pain
Treating chronic back pain requires a multifaceted approach that addresses the underlying causes, alleviates symptoms, and improves overall quality of life. This section explores various treatment options, ranging from conservative measures to advanced interventions.
3.1 Conservative Treatments
Conservative treatments are often the first line of defense against chronic back pain. These non-invasive approaches aim to reduce pain and improve function without the need for surgery. Common conservative treatments include:
- Physical Therapy: Tailored exercise programs designed to strengthen the back muscles, improve flexibility, and enhance posture.
- Medications: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, and prescription medications, such as muscle relaxants or antidepressants, may be used to manage pain.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area can help reduce inflammation and alleviate pain.
- Chiropractic Care: Manual manipulation of the spine by a chiropractor can help relieve pain and improve mobility.
These treatments are often used in combination to achieve optimal results. A study published in the Journal of Orthopaedic & Sports Physical Therapy found that a multimodal approach, including physical therapy and medication, was more effective than single-modality treatments in managing chronic back pain.
3.2 Advanced Interventions
For individuals who do not respond to conservative treatments, advanced interventions may be necessary. These options include:
- Epidural Steroid Injections: Corticosteroid injections into the epidural space can help reduce inflammation and relieve pain.
- Nerve Blocks: Injections of anesthetic agents near specific nerves can provide temporary pain relief.
- Radiofrequency Ablation: A procedure that uses heat to destroy nerve fibers responsible for transmitting pain signals.
These interventions are typically performed by pain management specialists and may provide significant relief for individuals with chronic back pain. A study in the journal Pain Medicine reported that radiofrequency ablation resulted in substantial pain reduction and improved function in patients with chronic back pain.
3.3 Surgical Options
Surgery is considered a last resort for chronic back pain and is typically reserved for cases where conservative and advanced treatments have failed. Common surgical procedures include:
- Discectomy: Removal of a herniated disc that is pressing on a nerve.
- Laminectomy: Removal of part of the vertebra to relieve pressure on the spinal cord or nerves.
- Spinal Fusion: Joining two or more vertebrae to stabilize the spine and reduce pain.
Surgical outcomes can vary, and it is essential for patients to discuss the potential risks and benefits with their healthcare provider. A study published in The New England Journal of Medicine found that surgical intervention for herniated discs resulted in better outcomes than non-surgical treatment in certain cases.
3.4 Complementary and Alternative Therapies
Complementary and alternative therapies can be valuable adjuncts to conventional treatments for chronic back pain. These therapies include:
- Acupuncture: Insertion of thin needles into specific points on the body to relieve pain and promote healing.
- Massage Therapy: Manipulation of soft tissues to reduce muscle tension and improve circulation.
- Yoga and Tai Chi: Mind-body practices that enhance flexibility, strength, and relaxation.
Research supports the efficacy of these therapies in managing chronic back pain. A meta-analysis published in the journal Pain found that acupuncture significantly reduced pain intensity and improved function in patients with chronic back pain.
3.5 The Role of Multidisciplinary Pain Management
Multidisciplinary pain management involves a team-based approach to treating chronic back pain, incorporating input from various healthcare professionals, including physicians, physical therapists, psychologists, and nutritionists. This approach addresses the physical, emotional, and social aspects of pain, providing comprehensive care for patients.
A study published in the journal Pain Management Nursing highlighted the benefits of multidisciplinary pain management, reporting improved pain relief, function, and quality of life for patients with chronic back pain.
4. Prevention Strategies for Chronic Back Pain
Preventing chronic back pain is a proactive approach that involves adopting healthy habits and making lifestyle changes to reduce the risk of developing or exacerbating the condition. This section explores effective prevention strategies.
4.1 Ergonomic Practices
Ergonomics plays a crucial role in preventing chronic back pain, particularly in the workplace. Key ergonomic practices include:
- Proper Desk Setup: Ensuring that the computer monitor is at eye level, the chair provides adequate lumbar support, and the keyboard and mouse are within easy reach.
- Lifting Techniques: Using proper lifting techniques, such as bending at the knees and keeping the load close to the body, can prevent back injuries.
- Frequent Breaks: Taking regular breaks to stretch and move around can reduce the strain on the back muscles.
Employers can promote ergonomic practices by providing training and resources to employees. A study published in the journal Applied Ergonomics found that ergonomic interventions significantly reduced the incidence of work-related musculoskeletal disorders, including back pain.
4.2 Exercise and Physical Activity
Regular exercise and physical activity are essential for maintaining a healthy back and preventing chronic pain. Recommended activities include:
- Strengthening Exercises: Exercises that target the core muscles, such as planks and bridges, can provide stability and support to the spine.
- Aerobic Activities: Low-impact activities like walking, swimming, and cycling can improve cardiovascular health and promote weight management.
- Flexibility Exercises: Stretching exercises, such as yoga or Pilates, can enhance flexibility and reduce muscle tension.
A study published in the journal Spine found that individuals who engaged in regular physical activity had a lower risk of developing chronic back pain compared to those with a sedentary lifestyle.
4.3 Weight Management
Maintaining a healthy weight is crucial for preventing chronic back pain, as excess body weight can place additional stress on the spine. Strategies for weight management include:
- Balanced Diet: Consuming a diet rich in fruits, vegetables, lean proteins, and whole grains can support weight management and overall health.
- Portion Control: Being mindful of portion sizes can help prevent overeating and weight gain.
- Regular Physical Activity: Incorporating regular exercise into daily routines can aid in weight management and reduce the risk of back pain.
A study published in the journal Obesity found that individuals who maintained a healthy weight had a lower risk of developing chronic back pain compared to those who were overweight or obese.
4.4 Stress Management
Stress can exacerbate chronic back pain by increasing muscle tension and altering pain perception. Effective stress management techniques include:
- Mindfulness Meditation: Practicing mindfulness meditation can help reduce stress and improve emotional well-being.
- Deep Breathing Exercises: Deep breathing exercises can promote relaxation and reduce muscle tension.
- Cognitive-Behavioral Therapy (CBT): CBT can help individuals develop coping strategies to manage stress and pain.
A study published in the journal Pain found that stress management interventions significantly reduced pain intensity and improved quality of life in patients with chronic back pain.
4.5 Education and Awareness
Education and awareness are essential components of chronic back pain prevention. By understanding the risk factors and adopting healthy habits, individuals can take proactive steps to protect their back health. Educational initiatives may include:
- Workshops and Seminars: Providing information on back health, ergonomics, and exercise can empower individuals to make informed decisions.
- Online Resources: Access to online resources, such as articles, videos, and interactive tools, can enhance awareness and knowledge.
- Community Programs: Community-based programs that promote physical activity and healthy lifestyles can support back pain prevention efforts.
A study published in the journal Health Education Research found that educational interventions significantly increased knowledge and awareness of back pain prevention strategies among participants.
5. Living with Chronic Back Pain: Coping Strategies and Support
Living with chronic back pain can be challenging, but effective coping strategies and support systems can help individuals manage their condition and improve their quality of life. This section explores practical approaches to coping with chronic back pain.
5.1 Developing a Pain Management Plan
A personalized pain management plan is essential for effectively managing chronic back pain. Key components of a pain management plan include:
- Goal Setting: Establishing realistic goals for pain reduction, function improvement, and overall well-being.
- Medication Management: Working with healthcare providers to optimize medication use and minimize side effects.
- Regular Monitoring: Tracking pain levels, triggers, and treatment effectiveness to adjust the plan as needed.
A study published in the journal Pain Management Nursing found that individualized pain management plans significantly improved pain relief and quality of life for patients with chronic back pain.
5.2 Building a Support Network
A strong support network can provide emotional and practical assistance for individuals living with chronic back pain. Strategies for building a support network include:
- Family and Friends: Engaging family and friends in the pain management process can provide encouragement and understanding.
- Support Groups: Joining support groups, either in-person or online, can connect individuals with others who share similar experiences.
- Healthcare Providers: Collaborating with healthcare providers, including doctors, physical therapists, and mental health professionals, can ensure comprehensive care.
A study published in the journal Pain found that social support significantly improved coping and reduced pain-related disability in patients with chronic back pain.
5.3 Mind-Body Techniques
Mind-body techniques can help individuals manage chronic back pain by promoting relaxation and reducing stress. Effective mind-body techniques include:
- Meditation: Practicing meditation can enhance mindfulness and reduce pain perception.
- Progressive Muscle Relaxation: Systematically tensing and relaxing muscle groups can reduce muscle tension and promote relaxation.
- Guided Imagery: Using visualization techniques to create calming mental images can reduce stress and improve well-being.
A study published in the journal Pain Management Nursing found that mind-body techniques significantly reduced pain intensity and improved quality of life for patients with chronic back pain.
5.4 Adapting Daily Activities
Adapting daily activities can help individuals manage chronic back pain and maintain independence. Strategies for adapting activities include:
- Pacing: Balancing activity and rest to prevent overexertion and minimize pain flare-ups.
- Assistive Devices: Using assistive devices, such as braces or ergonomic tools, can reduce strain on the back.
- Task Modification: Modifying tasks, such as using a stool while cooking or taking breaks during prolonged activities, can reduce pain.
A study published in the journal Pain found that activity adaptation strategies significantly improved function and reduced pain-related disability in patients with chronic back pain.
5.5 Seeking Professional Help
Seeking professional help is essential for individuals struggling to manage chronic back pain on their own. Professional support may include:
- Pain Management Specialists: Specialists can provide advanced interventions and develop comprehensive treatment plans.
- Mental Health Professionals: Therapists can help individuals cope with the emotional impact of chronic pain and develop effective coping strategies.
- Rehabilitation Programs: Comprehensive rehabilitation programs can provide multidisciplinary care and support for individuals with chronic back pain.
A study published in the journal Pain Management Nursing found that professional support significantly improved pain relief and quality of life for patients with chronic back pain.
Conclusion
Chronic back pain is a complex condition that requires a comprehensive understanding of its causes, symptoms, diagnosis, treatment options, and prevention strategies. By exploring these aspects, individuals affected by chronic back pain can gain valuable insights and practical advice for managing their condition effectively. From conservative treatments to advanced interventions, a wide range of options is available to alleviate pain and improve quality of life. Additionally, adopting healthy habits and making lifestyle changes can help