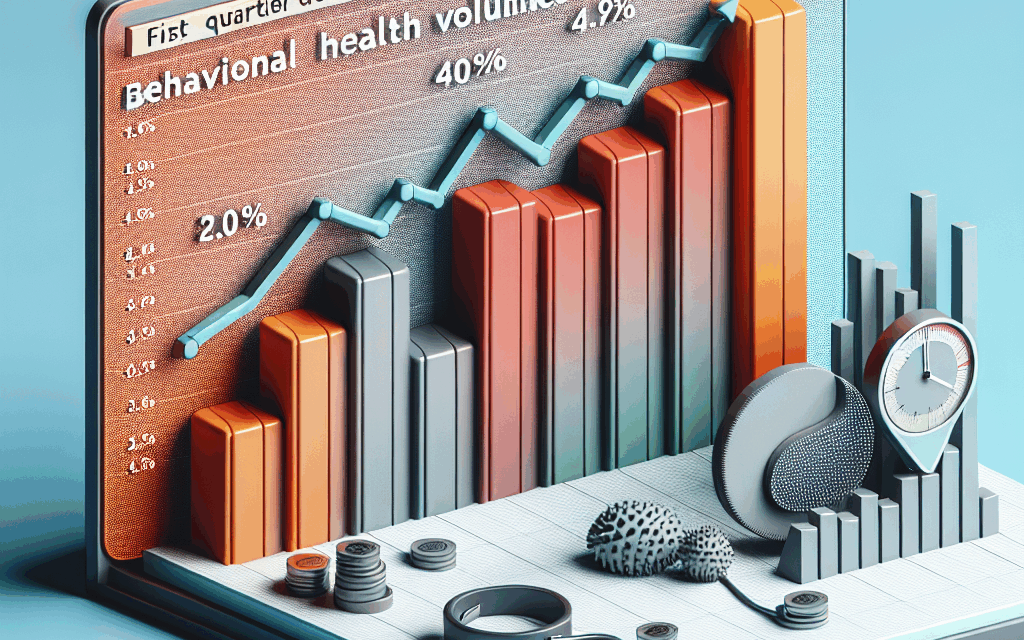
UHS Reports Decrease in Behavioral Health Volumes for Q1
Universal Health Services (UHS), one of the largest healthcare management companies in the United States, has recently reported a notable decrease in behavioral health volumes for the first quarter of the fiscal year. This decline raises important questions about the state of mental health services, the factors contributing to this trend, and its implications for patients and healthcare providers alike. In this article, we will explore the various dimensions of this issue, including the current landscape of behavioral health, the impact of the COVID-19 pandemic, the role of telehealth, and the future of mental health services.
Understanding the Current Landscape of Behavioral Health
The behavioral health sector encompasses a wide range of services aimed at treating mental health disorders and substance use issues. This includes inpatient and outpatient care, therapy, counseling, and medication management. According to the National Institute of Mental Health (NIMH), nearly one in five adults in the U.S. experiences mental illness in a given year, highlighting the critical need for accessible and effective behavioral health services.
UHS operates numerous facilities across the country, providing a variety of mental health services. However, the recent report indicating a decrease in patient volumes raises concerns about access to care and the overall health of the behavioral health system. Several factors may contribute to this decline:
- Stigma and Awareness: Despite growing awareness of mental health issues, stigma still prevents many individuals from seeking help.
- Access to Care: Geographic and financial barriers can limit access to necessary services, particularly in rural areas.
- Insurance Coverage: Variability in insurance coverage for mental health services can deter patients from pursuing treatment.
- Workforce Shortages: A shortage of qualified mental health professionals can lead to longer wait times and reduced availability of services.
- COVID-19 Impact: The pandemic has altered the landscape of healthcare, affecting how and when individuals seek treatment.
Understanding these factors is crucial for addressing the decline in behavioral health volumes and ensuring that individuals receive the care they need.
The Impact of the COVID-19 Pandemic on Behavioral Health
The COVID-19 pandemic has had a profound impact on mental health across the globe. The stressors associated with the pandemic, including isolation, economic uncertainty, and health concerns, have exacerbated existing mental health issues and created new challenges for many individuals. According to a report from the Centers for Disease Control and Prevention (CDC), the prevalence of anxiety and depression symptoms increased significantly during the pandemic.
Despite the heightened need for mental health services, UHS has reported a decrease in behavioral health volumes. This paradox can be attributed to several factors:
- Fear of Seeking Care: Many individuals may have avoided seeking treatment due to fears of contracting the virus in healthcare settings.
- Disruption of Services: The pandemic led to the temporary closure of some facilities and a reduction in available services, impacting patient volumes.
- Shift to Telehealth: While telehealth has expanded access to care for some, it may not be suitable for all patients, particularly those with severe mental health issues.
- Economic Factors: Job loss and financial instability may have made it difficult for individuals to afford care, leading to decreased volumes.
- Changes in Priorities: Some individuals may have prioritized physical health concerns over mental health during the pandemic, leading to a decline in behavioral health visits.
As the pandemic continues to evolve, understanding its impact on behavioral health is essential for developing strategies to improve access to care and support individuals in need.
The Role of Telehealth in Behavioral Health Services
Telehealth has emerged as a critical tool for delivering behavioral health services, particularly during the pandemic. The ability to connect with mental health professionals remotely has provided a lifeline for many individuals seeking support. UHS has adapted to this shift by expanding its telehealth offerings, allowing patients to access care from the comfort of their homes.
However, the transition to telehealth has not been without challenges. Some of the key considerations include:
- Access to Technology: Not all patients have access to the necessary technology or internet connectivity to participate in telehealth sessions.
- Comfort with Technology: Some individuals may feel uncomfortable using technology for healthcare, which can hinder their willingness to engage in telehealth services.
- Quality of Care: While telehealth can be effective for many patients, it may not provide the same level of care for those with severe or complex mental health issues.
- Insurance Reimbursement: Variability in insurance coverage for telehealth services can create barriers for patients seeking care.
- Regulatory Challenges: Different states have varying regulations regarding telehealth, which can complicate service delivery.
Despite these challenges, telehealth has the potential to play a significant role in the future of behavioral health services. By addressing barriers to access and ensuring that patients receive high-quality care, telehealth can help mitigate the decline in behavioral health volumes reported by UHS.
Addressing Workforce Shortages in Behavioral Health
The shortage of qualified mental health professionals is a significant challenge facing the behavioral health sector. According to the Health Resources and Services Administration (HRSA), there is a critical shortage of mental health providers in many areas, particularly in rural and underserved communities. This shortage can lead to longer wait times for patients and decreased access to care.
UHS and other healthcare organizations must prioritize workforce development to address this issue. Some strategies to consider include:
- Incentives for Providers: Offering financial incentives, loan forgiveness programs, and competitive salaries can attract more professionals to the field.
- Training and Education: Expanding training programs for mental health professionals can help increase the number of qualified providers.
- Telehealth Integration: Encouraging providers to offer telehealth services can help reach more patients and alleviate some of the burden on in-person services.
- Collaboration with Educational Institutions: Partnering with universities and colleges can create pathways for students to enter the mental health workforce.
- Support for Burnout: Providing resources and support for mental health professionals can help reduce burnout and retain staff in the field.
By addressing workforce shortages, UHS can improve access to behavioral health services and better meet the needs of patients seeking care.
The Future of Behavioral Health Services
As UHS navigates the challenges of decreased behavioral health volumes, it is essential to consider the future of mental health services. The landscape is evolving, and several trends are shaping the direction of behavioral health:
- Increased Focus on Integrated Care: Integrating mental health services with primary care can improve access and outcomes for patients.
- Emphasis on Prevention: Focusing on preventive measures and early intervention can help reduce the prevalence of mental health issues.
- Advancements in Technology: Innovations in technology, including artificial intelligence and data analytics, can enhance the delivery of mental health services.
- Policy Changes: Advocacy for policy changes that support mental health funding and access can drive improvements in the system.
- Community-Based Approaches: Engaging communities in mental health initiatives can help reduce stigma and promote awareness.
By embracing these trends and adapting to the changing landscape, UHS can position itself to better serve individuals in need of behavioral health services and address the decline in patient volumes.
Conclusion
The recent report from UHS indicating a decrease in behavioral health volumes for Q1 highlights significant challenges within the mental health sector. Understanding the current landscape, the impact of the COVID-19 pandemic, the role of telehealth, workforce shortages, and future trends is essential for addressing these challenges and improving access to care.
As we move forward, it is crucial for healthcare organizations, policymakers, and communities to work together to ensure that individuals receive the support they need. By addressing barriers to access, investing in workforce development, and embracing innovative solutions, we can create a more robust and effective behavioral health system that meets the needs of all individuals.
In summary, the decline in behavioral health volumes reported by UHS serves as a call to action for all stakeholders in the mental health field. By prioritizing access, quality of care, and workforce development, we can work towards a future where mental health services are accessible, effective, and stigma-free.