Transforming Lumbar Fusions: The Impact of Medical Technology
Lumbar fusion surgery has long been a cornerstone in the treatment of chronic back pain and spinal instability. As medical technology continues to evolve, the landscape of lumbar fusions is undergoing a significant transformation. This article explores the impact of medical technology on lumbar fusions, focusing on five key areas: advancements in surgical techniques, the role of imaging technologies, innovations in biomaterials, the integration of robotics and automation, and the future of telemedicine in post-operative care.
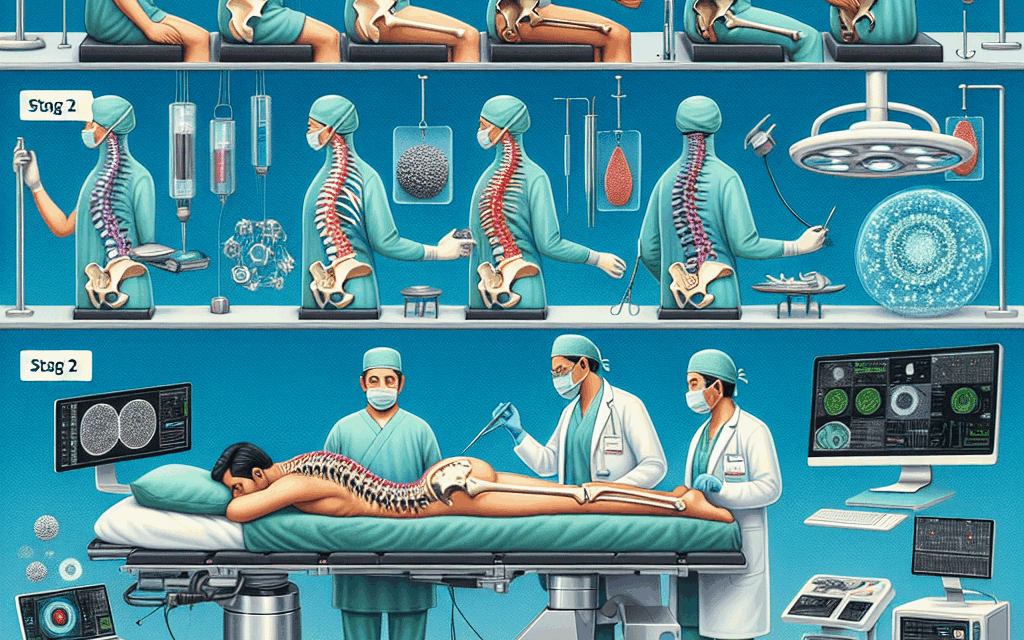
Advancements in Surgical Techniques
Over the past few decades, surgical techniques for lumbar fusion have evolved dramatically. Traditional open surgery, which involves large incisions and significant muscle disruption, has gradually been replaced by minimally invasive techniques. These advancements have led to reduced recovery times, less postoperative pain, and improved patient outcomes.
Minimally invasive lumbar fusion (MILF) techniques utilize smaller incisions and specialized instruments to access the spine. This approach minimizes soft tissue damage and allows for quicker recovery. Studies have shown that patients undergoing MILF experience less blood loss and shorter hospital stays compared to those who undergo traditional open surgery. For instance, a study published in the Journal of Spinal Disorders & Techniques found that patients who underwent MILF had a 30% reduction in hospital stay duration and a 40% decrease in postoperative pain levels.
Another significant advancement is the use of endoscopic techniques in lumbar fusion. Endoscopic spine surgery allows surgeons to visualize the surgical site through a small camera, providing enhanced precision. This technique is particularly beneficial for patients with complex anatomical variations or those who have had previous surgeries. A case study involving a 45-year-old patient with recurrent herniated discs demonstrated that endoscopic lumbar fusion resulted in a successful outcome with minimal complications, highlighting the effectiveness of this approach.
Furthermore, the development of intraoperative navigation systems has revolutionized the way surgeons perform lumbar fusions. These systems use advanced imaging technologies to provide real-time feedback during surgery, allowing for precise placement of screws and implants. A study published in the European Spine Journal reported that the use of navigation systems improved the accuracy of screw placement by over 90%, significantly reducing the risk of complications.
In summary, advancements in surgical techniques have transformed lumbar fusions, making them safer and more effective. Minimally invasive approaches, endoscopic techniques, and intraoperative navigation systems have all contributed to improved patient outcomes and reduced recovery times.
The Role of Imaging Technologies
Imaging technologies play a crucial role in the planning and execution of lumbar fusion surgeries. Accurate imaging is essential for diagnosing spinal conditions, assessing the extent of damage, and determining the most appropriate surgical approach. Recent advancements in imaging technologies have significantly enhanced the precision of lumbar fusions.
Magnetic resonance imaging (MRI) and computed tomography (CT) scans are commonly used to visualize the spine and surrounding structures. These imaging modalities provide detailed information about the anatomy of the spine, allowing surgeons to identify issues such as herniated discs, spinal stenosis, and degenerative disc disease. A study published in the Journal of Neurosurgery: Spine found that preoperative MRI significantly improved surgical planning and outcomes in patients undergoing lumbar fusion.
In addition to traditional imaging techniques, the emergence of 3D imaging has revolutionized the way surgeons approach lumbar fusions. 3D imaging allows for the creation of detailed models of the spine, enabling surgeons to visualize complex anatomical relationships. This technology is particularly beneficial for patients with unique spinal deformities or previous surgical interventions. A case study involving a patient with scoliosis demonstrated that 3D imaging facilitated a more tailored surgical approach, resulting in a successful fusion and improved alignment.
Moreover, intraoperative imaging technologies, such as fluoroscopy and intraoperative CT, have become integral to lumbar fusion surgeries. These technologies provide real-time imaging during the procedure, allowing surgeons to confirm the correct placement of implants and assess the surgical site. A study published in the Journal of Orthopaedic Surgery and Research found that intraoperative imaging reduced the rate of revision surgeries by 25%, underscoring its importance in enhancing surgical accuracy.
In conclusion, imaging technologies have transformed the landscape of lumbar fusions by providing surgeons with the tools needed for accurate diagnosis and precise surgical planning. The integration of 3D imaging and intraoperative imaging has further enhanced the safety and effectiveness of these procedures.
Innovations in Biomaterials
The choice of biomaterials used in lumbar fusion surgeries has a profound impact on the success of the procedure. Traditional materials, such as autografts and allografts, have been widely used for decades. However, recent innovations in biomaterials are paving the way for improved fusion rates and patient outcomes.
One of the most significant advancements in biomaterials is the development of synthetic bone graft substitutes. These materials are designed to mimic the properties of natural bone and promote osteogenesis, the process of new bone formation. For example, bioactive glass and calcium phosphate ceramics have shown promising results in enhancing bone healing and fusion rates. A study published in the Journal of Bone and Joint Surgery found that patients receiving synthetic grafts had a 20% higher fusion rate compared to those receiving autografts.
Another innovation is the use of bioactive coatings on implants. These coatings promote osseointegration, the process by which bone grows into and anchors to the implant. Research has shown that implants coated with bioactive materials, such as hydroxyapatite, exhibit improved stability and reduced risk of implant failure. A case study involving a patient with a history of implant failure demonstrated that the use of bioactive-coated implants resulted in successful fusion and long-term stability.
Furthermore, the development of resorbable materials has opened new avenues for lumbar fusion surgeries. Resorbable implants gradually dissolve over time, allowing for natural bone growth to take its place. This approach reduces the need for additional surgeries to remove hardware and minimizes complications associated with permanent implants. A study published in the European Spine Journal reported that patients receiving resorbable implants experienced similar fusion rates to those with traditional implants, with fewer complications.
In summary, innovations in biomaterials are transforming lumbar fusions by enhancing fusion rates, promoting osseointegration, and reducing complications. The development of synthetic grafts, bioactive coatings, and resorbable materials represents a significant leap forward in the field of spinal surgery.
The Integration of Robotics and Automation
The integration of robotics and automation into lumbar fusion surgeries is revolutionizing the way these procedures are performed. Robotic-assisted surgery offers enhanced precision, improved outcomes, and reduced variability in surgical techniques.
Robotic systems, such as the Mazor Robotics Renaissance system, allow surgeons to plan and execute surgeries with unparalleled accuracy. These systems use preoperative imaging to create a detailed surgical plan, which is then executed with robotic assistance. A study published in the Journal of Neurosurgery found that robotic-assisted lumbar fusions resulted in a 50% reduction in intraoperative complications compared to traditional techniques.
One of the key benefits of robotic-assisted surgery is the ability to perform complex procedures with minimal invasiveness. The precision of robotic systems allows for smaller incisions and less disruption of surrounding tissues. A case study involving a patient with severe spinal deformity demonstrated that robotic-assisted lumbar fusion resulted in a successful outcome with minimal postoperative pain and a rapid recovery.
Moreover, robotics can enhance the accuracy of screw placement, a critical aspect of lumbar fusion surgeries. Studies have shown that robotic-assisted screw placement achieves a higher accuracy rate compared to traditional freehand techniques. A meta-analysis published in the Spine Journal found that robotic-assisted screw placement had an accuracy rate of over 95%, significantly reducing the risk of complications associated with misplaced screws.
In addition to improving surgical precision, robotics also has the potential to streamline surgical workflows. Automated systems can assist with tasks such as instrument tracking and inventory management, allowing surgical teams to focus on patient care. A study published in the Journal of Robotic Surgery reported that the integration of automation in surgical workflows reduced operating room time by an average of 20%, leading to increased efficiency and cost savings.
In conclusion, the integration of robotics and automation into lumbar fusion surgeries is transforming the field by enhancing precision, improving outcomes, and streamlining surgical workflows. As technology continues to advance, the role of robotics in spinal surgery is expected to expand further.
The Future of Telemedicine in Post-Operative Care
As the healthcare landscape evolves, telemedicine is becoming an increasingly important component of post-operative care for lumbar fusion patients. The ability to provide remote monitoring and follow-up care has the potential to improve patient outcomes and enhance the overall surgical experience.
Telemedicine allows healthcare providers to conduct virtual consultations, enabling patients to receive care from the comfort of their homes. This is particularly beneficial for patients who may have difficulty traveling to follow-up appointments due to pain or mobility issues. A study published in the Journal of Telemedicine and Telecare found that telemedicine consultations for post-operative lumbar fusion patients resulted in high levels of patient satisfaction and reduced no-show rates for follow-up appointments.
Remote monitoring technologies, such as wearable devices and mobile health applications, are also playing a crucial role in post-operative care. These technologies allow patients to track their recovery progress, report symptoms, and communicate with their healthcare providers in real-time. A case study involving a patient who underwent lumbar fusion demonstrated that remote monitoring led to early identification of complications, resulting in timely interventions and improved outcomes.
Furthermore, telemedicine can facilitate education and support for patients during their recovery. Virtual platforms can provide access to educational resources, rehabilitation programs, and support groups, empowering patients to take an active role in their recovery. A study published in the Journal of Orthopaedic Research found that patients who participated in telehealth rehabilitation programs reported higher levels of engagement and satisfaction compared to those receiving traditional in-person rehabilitation.
In conclusion, the future of telemedicine in post-operative care for lumbar fusion patients is promising. By providing remote monitoring, virtual consultations, and educational resources, telemedicine has the potential to enhance patient outcomes and improve the overall surgical experience.
Conclusion
The impact of medical technology on lumbar fusions is profound and multifaceted. Advancements in surgical techniques, imaging technologies, biomaterials, robotics, and telemedicine are transforming the way these procedures are performed and how patients recover. As technology continues to evolve, the future of lumbar fusions looks promising, with the potential for improved outcomes, reduced complications, and enhanced patient experiences.
In summary, the key takeaways from this article include:
- Minimally invasive techniques and endoscopic approaches are revolutionizing surgical methods.
- Advanced imaging technologies, including 3D imaging and intraoperative imaging, enhance surgical precision.
- Innovations in biomaterials improve fusion rates and reduce complications.
- Robotic-assisted surgery enhances precision and streamlines surgical workflows.
- Telemedicine is transforming post-operative care, improving patient outcomes and satisfaction.
As we look to the future, continued research and innovation in medical technology will undoubtedly shape the field of lumbar fusions, ultimately leading to better care for patients suffering from spinal disorders.