The Payer Pod: Strategies for Health Plan Success in 2025
As the healthcare landscape continues to evolve, health plans face unprecedented challenges and opportunities. The emergence of value-based care, technological advancements, and changing consumer expectations are reshaping the way health plans operate. In this article, we will explore the concept of the “Payer Pod” and outline strategies that health plans can adopt to ensure success in 2025. We will delve into five key subtopics: the importance of data analytics, the role of consumer engagement, the integration of technology, the shift towards value-based care, and the necessity of strategic partnerships.
1. The Importance of Data Analytics
Data analytics has become a cornerstone of effective decision-making in the healthcare industry. For health plans, leveraging data analytics can lead to improved patient outcomes, reduced costs, and enhanced operational efficiency. In 2025, health plans that harness the power of data will be better positioned to thrive in a competitive market.
Understanding Population Health Management
Population health management (PHM) involves analyzing data to identify health trends and risks within specific populations. By utilizing data analytics, health plans can segment their members based on various factors such as demographics, health conditions, and utilization patterns. This segmentation allows for targeted interventions that can improve health outcomes.
- Risk Stratification: Health plans can use predictive analytics to identify high-risk members who may require more intensive care management. For example, a study by the American Journal of Managed Care found that health plans that implemented risk stratification saw a 20% reduction in hospital readmissions.
- Chronic Disease Management: Data analytics can help health plans develop tailored programs for managing chronic diseases. By analyzing claims data, health plans can identify members with conditions such as diabetes or hypertension and provide them with personalized care plans.
Enhancing Operational Efficiency
Data analytics can also streamline operations within health plans. By analyzing internal processes, health plans can identify inefficiencies and areas for improvement. For instance, a health plan may discover that certain claims processing workflows are causing delays, leading to member dissatisfaction.
- Claims Processing: By utilizing machine learning algorithms, health plans can automate claims processing, reducing the time it takes to adjudicate claims and improving member satisfaction.
- Cost Management: Data analytics can help health plans identify high-cost areas and implement cost-saving measures. For example, a health plan may analyze prescription drug utilization and negotiate better rates with pharmaceutical companies.
Case Study: A Successful Data-Driven Health Plan
One notable example of a health plan successfully leveraging data analytics is the Blue Cross Blue Shield of Massachusetts (BCBSMA). BCBSMA implemented a comprehensive data analytics strategy that allowed them to identify high-risk members and develop targeted interventions. As a result, they reported a 15% reduction in emergency room visits among high-risk members within the first year of implementation.
2. The Role of Consumer Engagement
In 2025, consumer engagement will be a critical factor in the success of health plans. As patients become more empowered and informed, health plans must adapt their strategies to meet the evolving expectations of their members.
Personalized Communication
Effective communication is key to engaging members. Health plans should focus on personalized communication strategies that resonate with their members. This can include tailored messaging based on individual health needs, preferences, and behaviors.
- Targeted Outreach: Health plans can use data analytics to segment their member base and create targeted outreach campaigns. For example, a health plan may send reminders for preventive screenings to members who are due for them.
- Multichannel Communication: Engaging members through various channels—such as email, text messages, and mobile apps—can enhance communication effectiveness. A study by the Pew Research Center found that 81% of Americans own a smartphone, making mobile communication a vital tool for health plans.
Empowering Members with Tools and Resources
Health plans should provide members with the tools and resources they need to take charge of their health. This includes access to educational materials, wellness programs, and digital health tools.
- Health Education: Providing educational resources on topics such as nutrition, exercise, and chronic disease management can empower members to make informed health decisions.
- Digital Health Tools: Offering mobile apps that allow members to track their health metrics, schedule appointments, and communicate with care teams can enhance engagement and improve health outcomes.
Case Study: Engaging Members through Technology
A prime example of effective consumer engagement is the health plan Aetna, which launched a mobile app that allows members to access their health information, schedule appointments, and receive personalized health tips. Aetna reported a 30% increase in member engagement within the first year of the app’s launch, demonstrating the impact of technology on consumer engagement.
3. The Integration of Technology
Technology is transforming the healthcare landscape, and health plans must embrace innovative solutions to remain competitive. In 2025, the integration of technology will be essential for improving care delivery, enhancing member experiences, and optimizing operations.
Telehealth Services
The COVID-19 pandemic accelerated the adoption of telehealth services, and this trend is expected to continue in 2025. Health plans should invest in telehealth solutions to provide members with convenient access to care.
- Increased Access to Care: Telehealth can help bridge gaps in care, especially for members in rural or underserved areas. A study by the Journal of the American Medical Association found that telehealth visits increased by 154% during the pandemic, highlighting its potential to improve access.
- Cost-Effectiveness: Telehealth can reduce healthcare costs by minimizing the need for in-person visits and hospitalizations. Health plans that offer telehealth services can also benefit from lower overall claims costs.
Artificial Intelligence and Machine Learning
Artificial intelligence (AI) and machine learning (ML) are revolutionizing the way health plans operate. These technologies can enhance decision-making, improve risk assessment, and streamline administrative processes.
- Predictive Analytics: AI can analyze vast amounts of data to identify patterns and predict future health outcomes. Health plans can use predictive analytics to identify members at risk for chronic conditions and intervene early.
- Fraud Detection: AI can help health plans detect fraudulent claims by analyzing patterns in claims data. This can lead to significant cost savings and improved integrity within the healthcare system.
Case Study: AI in Action
UnitedHealth Group has successfully integrated AI into its operations to enhance care delivery and improve member outcomes. By utilizing AI algorithms to analyze claims data, UnitedHealth Group identified potential fraud cases and saved millions in fraudulent claims. Additionally, their AI-driven predictive analytics helped identify high-risk members, allowing for timely interventions.
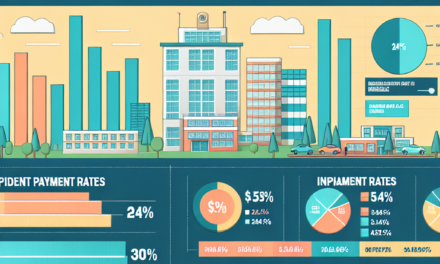
4. The Shift Towards Value-Based Care
The transition from fee-for-service to value-based care is a significant trend in the healthcare industry. In 2025, health plans that embrace value-based care models will be better positioned to improve patient outcomes and reduce costs.
Understanding Value-Based Care Models
Value-based care focuses on delivering high-quality care while controlling costs. Health plans can adopt various value-based care models, including accountable care organizations (ACOs), bundled payments, and pay-for-performance programs.
- Accountable Care Organizations (ACOs): ACOs are groups of healthcare providers that work together to coordinate care for a specific population. Health plans that partner with ACOs can benefit from improved care coordination and reduced costs.
- Bundled Payments: Bundled payment models involve paying a single price for a set of services related to a specific condition or procedure. This encourages providers to work together to deliver efficient care.
Measuring Quality and Outcomes
To succeed in value-based care, health plans must establish metrics to measure quality and outcomes. This includes tracking key performance indicators (KPIs) such as hospital readmission rates, patient satisfaction scores, and preventive care utilization.
- Quality Improvement Initiatives: Health plans can implement quality improvement initiatives based on data analysis to enhance care delivery. For example, a health plan may focus on reducing hospital readmissions by implementing post-discharge follow-up programs.
- Patient-Centered Care: Engaging patients in their care decisions and prioritizing their preferences can lead to better health outcomes. Health plans should encourage shared decision-making between patients and providers.
Case Study: Value-Based Care Success
The Medicare Shared Savings Program (MSSP) is an example of a successful value-based care initiative. ACOs participating in the MSSP have reported significant savings while improving quality metrics. According to the Centers for Medicare & Medicaid Services (CMS), ACOs saved Medicare $1.9 billion in 2019 while achieving higher quality scores compared to traditional fee-for-service models.
5. The Necessity of Strategic Partnerships
In an increasingly complex healthcare environment, strategic partnerships will be essential for health plans to succeed in 2025. Collaborating with various stakeholders can enhance care delivery, expand service offerings, and improve member experiences.
Collaborating with Providers
Building strong relationships with healthcare providers is crucial for health plans. Collaborative partnerships can lead to improved care coordination and better health outcomes for members.
- Integrated Care Models: Health plans can work with providers to develop integrated care models that prioritize seamless transitions between different levels of care. This can reduce fragmentation and improve patient experiences.
- Shared Savings Programs: Collaborating with providers on shared savings programs can incentivize both parties to focus on quality and cost-effective care delivery.
Engaging with Technology Vendors
As technology continues to play a pivotal role in healthcare, health plans should seek partnerships with technology vendors to enhance their capabilities. This includes collaborating with companies that specialize in telehealth, data analytics, and AI solutions.
- Innovative Solutions: Partnering with technology vendors can provide health plans with access to innovative solutions that improve operational efficiency and member engagement.
- Scalability: Collaborating with established technology vendors can help health plans scale their operations and adapt to changing market demands.
Case Study: Successful Partnerships
Anthem, Inc. has successfully formed strategic partnerships with various healthcare providers and technology companies to enhance its service offerings. By collaborating with telehealth providers, Anthem expanded access to virtual care for its members, resulting in increased member satisfaction and improved health outcomes.
Conclusion
The healthcare landscape is rapidly changing, and health plans must adapt to thrive in 2025. By embracing data analytics, enhancing consumer engagement, integrating technology, shifting towards value-based care, and forming strategic partnerships, health plans can position themselves for success. The Payer Pod concept emphasizes the importance of collaboration and innovation in navigating the complexities of the healthcare system. As health plans implement these strategies, they will not only improve their operational efficiency but also enhance the overall health and well-being of their members.
In summary, the key takeaways for health plans looking to succeed in 2025 include:
- Leverage data analytics for population health management and operational efficiency.
- Engage consumers through personalized communication and digital health tools.
- Integrate technology, including telehealth and AI, to enhance care delivery.
- Adopt value-based care models to improve patient outcomes and control costs.
- Form strategic partnerships with providers and technology vendors to expand capabilities.
By focusing on these strategies, health plans can navigate the challenges of the evolving healthcare landscape and achieve long-term success.