The Limitations of Rigid Technologies in Modern Healthcare Systems
In the rapidly evolving landscape of healthcare, technology plays a pivotal role in enhancing patient care, streamlining operations, and improving outcomes. However, the integration of rigid technologies—those that are inflexible, difficult to adapt, or slow to evolve—poses significant challenges to modern healthcare systems. This article explores the limitations of such technologies, examining their impact on patient care, operational efficiency, data management, and overall healthcare delivery. We will delve into five key subtopics: the inflexibility of rigid technologies, the challenges of interoperability, the impact on patient-centered care, the financial implications, and the future of healthcare technology.
1. The Inflexibility of Rigid Technologies
Rigid technologies in healthcare often refer to systems and tools that are not designed to adapt to the changing needs of healthcare providers and patients. This inflexibility can manifest in various ways, from outdated software systems to medical devices that cannot be easily updated or modified.
One of the primary limitations of rigid technologies is their inability to accommodate the dynamic nature of healthcare. For instance, as new medical guidelines emerge or as patient populations change, healthcare providers may find themselves constrained by technologies that do not allow for easy updates or modifications. This can lead to a disconnect between the latest evidence-based practices and the tools available to clinicians.
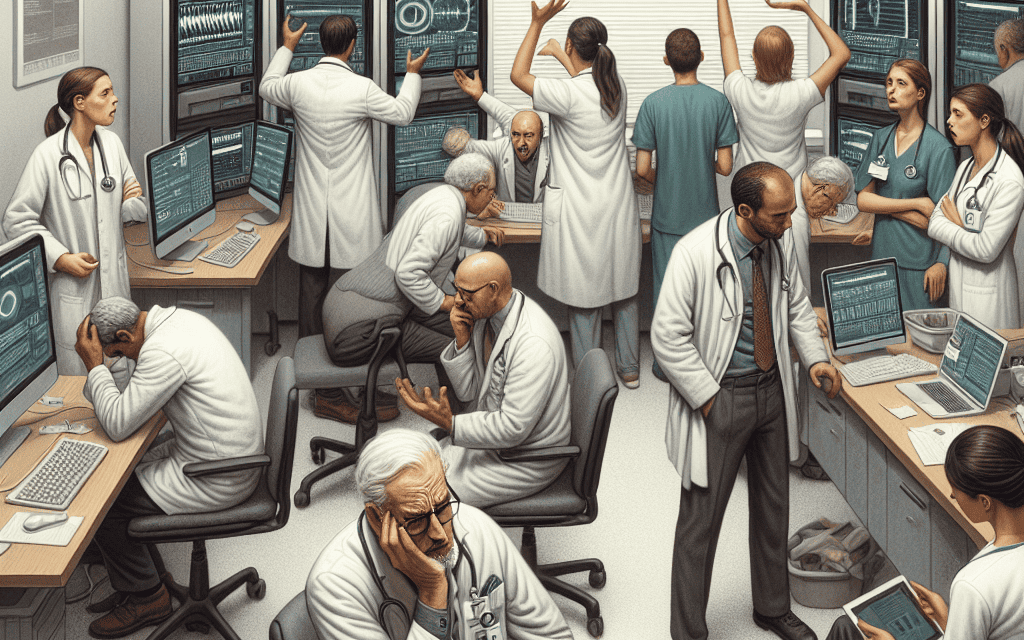
- Case Study: Electronic Health Records (EHRs) – Many EHR systems are built on legacy platforms that are difficult to modify. A study by the American Medical Association found that nearly 50% of physicians reported that their EHR systems did not meet their needs, primarily due to inflexibility in adapting to new workflows.
- Impact on Innovation – Rigid technologies can stifle innovation within healthcare organizations. When staff are forced to work within the confines of outdated systems, they may be less likely to explore new methods or technologies that could improve patient care.
Moreover, the inflexibility of rigid technologies can lead to increased frustration among healthcare providers. Clinicians often spend more time navigating cumbersome systems than focusing on patient care. This not only affects job satisfaction but can also lead to burnout, which is a growing concern in the healthcare industry.
In summary, the inflexibility of rigid technologies can hinder the ability of healthcare providers to deliver high-quality care, adapt to new challenges, and innovate in their practices. As the healthcare landscape continues to evolve, the need for more flexible and adaptable technologies becomes increasingly critical.
2. Challenges of Interoperability
Interoperability refers to the ability of different healthcare systems and technologies to communicate and exchange data seamlessly. Rigid technologies often lack the necessary interoperability, creating silos of information that can impede patient care and operational efficiency.
The challenges of interoperability are particularly evident in the context of electronic health records (EHRs). Many healthcare organizations use different EHR systems that do not communicate with one another, leading to fragmented patient information. This can result in incomplete patient histories, duplicated tests, and ultimately, suboptimal care.
- Statistics on Interoperability – According to a report from the Office of the National Coordinator for Health Information Technology, only 30% of hospitals reported that they could electronically send, receive, and integrate patient information from outside sources.
- Case Study: Care Coordination – A study published in the Journal of the American Medical Association highlighted that patients with chronic conditions often see multiple specialists. When these specialists use different EHR systems that do not communicate, it can lead to medication errors and conflicting treatment plans.
The lack of interoperability not only affects patient safety but also increases administrative burdens. Healthcare providers may spend significant time manually entering data or reconciling discrepancies between different systems. This inefficiency can detract from the time available for direct patient care.
Furthermore, the inability to share data across systems can hinder research and public health initiatives. For example, during the COVID-19 pandemic, the lack of interoperable systems made it challenging to track the spread of the virus and coordinate responses across different healthcare entities.
In conclusion, the challenges of interoperability associated with rigid technologies can have far-reaching implications for patient care, operational efficiency, and public health. As healthcare continues to advance, the need for systems that can communicate and share data seamlessly is paramount.
3. Impact on Patient-Centered Care
Patient-centered care is a model that emphasizes the involvement of patients in their own healthcare decisions, focusing on their individual needs and preferences. Rigid technologies can significantly impede the delivery of patient-centered care by creating barriers to communication and engagement.
One of the key limitations of rigid technologies is their tendency to prioritize efficiency over patient experience. For example, many EHR systems are designed to streamline administrative tasks, but they often do so at the expense of meaningful patient interactions. Clinicians may find themselves spending more time inputting data into rigid systems than engaging with patients, which can lead to a diminished patient experience.
- Case Study: Telehealth – The rise of telehealth during the COVID-19 pandemic highlighted the importance of flexible technologies. Providers using rigid telehealth platforms faced challenges in adapting to the unique needs of patients, such as those with limited technology access or those requiring additional support during virtual visits.
- Patient Engagement Tools – Many patient engagement tools are not designed to integrate with existing healthcare systems, leading to fragmented communication. Patients may receive information through multiple channels, making it difficult for them to stay informed about their care.
Moreover, rigid technologies can limit the ability of healthcare providers to personalize care. For instance, if a system does not allow for easy customization of treatment plans or patient education materials, providers may struggle to address the unique needs of each patient.
In summary, the impact of rigid technologies on patient-centered care is profound. By creating barriers to communication and engagement, these technologies can hinder the ability of healthcare providers to deliver personalized, high-quality care. As the focus on patient-centered care continues to grow, the need for more adaptable and user-friendly technologies becomes increasingly important.
4. Financial Implications
The financial implications of rigid technologies in healthcare are significant and multifaceted. While the initial investment in technology may seem justified, the long-term costs associated with inflexibility can outweigh the benefits.
One of the primary financial concerns is the cost of maintaining and upgrading rigid systems. Many healthcare organizations find themselves locked into contracts with technology vendors that offer limited flexibility for updates or modifications. This can lead to increased costs as organizations are forced to invest in additional training, support, and workarounds to compensate for the limitations of their systems.
- Hidden Costs – A study by the Healthcare Information and Management Systems Society (HIMSS) found that healthcare organizations often underestimate the hidden costs associated with rigid technologies, including lost productivity, increased administrative burdens, and potential legal liabilities due to data breaches.
- Return on Investment (ROI) – Rigid technologies may not deliver the expected ROI. For example, a hospital that invests in a rigid EHR system may find that the system does not improve efficiency or patient outcomes as anticipated, leading to wasted resources.
Additionally, the financial implications extend to patient care. When rigid technologies hinder communication and collaboration among providers, it can lead to increased hospital readmissions and complications, which ultimately drive up costs for both patients and healthcare organizations.
In conclusion, the financial implications of rigid technologies in healthcare are significant. The costs associated with maintenance, training, and lost productivity can quickly add up, making it essential for healthcare organizations to carefully consider their technology investments and seek out more flexible solutions.
5. The Future of Healthcare Technology
The future of healthcare technology is poised for transformation as the industry recognizes the limitations of rigid systems. Emerging trends indicate a shift towards more flexible, adaptable technologies that prioritize interoperability, patient-centered care, and innovation.
One of the most promising developments is the rise of cloud-based solutions. These technologies offer greater flexibility and scalability, allowing healthcare organizations to adapt to changing needs without the constraints of rigid systems. Cloud-based EHRs, for example, can be updated more easily and can integrate with other systems, enhancing interoperability.
- Artificial Intelligence (AI) – AI technologies are increasingly being integrated into healthcare systems to enhance decision-making and improve patient outcomes. These systems can analyze vast amounts of data and provide insights that help clinicians deliver personalized care.
- Patient Engagement Platforms – New patient engagement tools are being developed with a focus on user experience and integration. These platforms allow patients to access their health information, communicate with providers, and participate in their care more effectively.
Moreover, the emphasis on value-based care is driving the need for technologies that support collaboration and communication among providers. As healthcare organizations move away from fee-for-service models, the ability to share data and coordinate care becomes increasingly important.
In summary, the future of healthcare technology is moving towards more flexible and adaptable solutions that address the limitations of rigid systems. By embracing innovation and prioritizing interoperability, healthcare organizations can enhance patient care, improve operational efficiency, and ultimately transform the healthcare landscape.
Conclusion
The limitations of rigid technologies in modern healthcare systems are significant and multifaceted. From inflexibility and interoperability challenges to impacts on patient-centered care and financial implications, these technologies can hinder the ability of healthcare providers to deliver high-quality care. As the healthcare landscape continues to evolve, the need for more flexible, adaptable, and interoperable technologies becomes increasingly critical.
Healthcare organizations must recognize the importance of investing in technologies that prioritize innovation, collaboration, and patient engagement. By doing so, they can overcome the limitations of rigid systems and create a more efficient, effective, and patient-centered healthcare environment.