Surge in Private Equity Acquisitions of Disability Care Centers
The landscape of disability care centers is undergoing a significant transformation, driven largely by a surge in private equity (PE) acquisitions. This trend has sparked discussions about the implications for care quality, operational efficiency, and the overall sustainability of these essential services. In this article, we will explore the factors contributing to this surge, the impact on care quality, the financial motivations behind these acquisitions, the regulatory environment, and the future outlook for disability care centers in the context of private equity involvement.
Understanding the Surge in Private Equity Acquisitions
Private equity firms have increasingly turned their attention to the healthcare sector, particularly disability care centers. This trend can be attributed to several factors, including demographic shifts, the increasing demand for specialized care, and the potential for operational improvements.
Demographic Shifts and Increased Demand
One of the primary drivers of the surge in private equity acquisitions is the aging population. According to the U.S. Census Bureau, the number of Americans aged 65 and older is projected to reach 94.7 million by 2060, nearly doubling from 52 million in 2018. This demographic shift is leading to a higher prevalence of disabilities and chronic conditions, thereby increasing the demand for disability care services.
Moreover, the rise in awareness and advocacy for individuals with disabilities has led to a greater emphasis on quality care. Families are seeking facilities that not only provide basic services but also focus on enhancing the quality of life for their loved ones. This demand creates a lucrative opportunity for private equity firms looking to invest in and improve these facilities.
Operational Improvements and Efficiency
Private equity firms are known for their ability to streamline operations and implement best practices across their portfolio companies. In the context of disability care centers, this can mean adopting new technologies, improving staff training, and enhancing patient care protocols. For instance, many PE firms are investing in electronic health records (EHR) systems that improve patient tracking and care coordination.
Additionally, private equity firms often bring in experienced management teams that can identify inefficiencies and implement cost-saving measures. This operational expertise can lead to improved financial performance, which is attractive to investors. A study by the National Investment Center for Seniors Housing & Care (NIC) found that facilities owned by private equity firms often report higher occupancy rates and better financial metrics compared to their non-PE counterparts.
Market Trends and Investment Opportunities
The healthcare sector, particularly disability care, is viewed as a stable investment due to its essential nature. Unlike other industries that may be more susceptible to economic downturns, the demand for disability care services remains relatively constant. This stability makes it an attractive target for private equity investment.
Furthermore, the COVID-19 pandemic has highlighted the need for robust healthcare infrastructure, including disability care centers. As a result, private equity firms are increasingly looking to invest in facilities that can adapt to changing healthcare needs and provide high-quality care in a post-pandemic world.
The Impact on Care Quality
While the influx of private equity into disability care centers can lead to operational improvements, it also raises concerns about the potential impact on care quality. The profit-driven nature of private equity can sometimes conflict with the mission of providing compassionate and comprehensive care.
Quality of Care Concerns
Critics argue that private equity firms prioritize financial returns over patient care. This can manifest in various ways, such as cost-cutting measures that reduce staffing levels or limit access to essential services. A report by the American Health Care Association (AHCA) found that facilities owned by private equity firms often have lower staffing levels compared to non-PE facilities, which can negatively impact the quality of care provided to residents.
Moreover, the pressure to generate quick returns on investment can lead to a focus on short-term financial gains rather than long-term sustainability. This can result in facilities cutting corners or neglecting necessary upgrades and maintenance, ultimately affecting the living conditions and care provided to residents.
Case Studies: Successes and Failures
Examining specific case studies can provide valuable insights into the impact of private equity on disability care centers. For example, a well-documented case is that of a large private equity firm acquiring a chain of nursing homes. Initially, the firm implemented operational improvements that led to increased efficiency and higher occupancy rates. However, over time, reports emerged of inadequate staffing levels and declining care quality, leading to negative media coverage and regulatory scrutiny.
Conversely, there are also examples of successful private equity investments in disability care that have led to improved outcomes. In one case, a private equity firm invested in a network of disability care centers and focused on enhancing staff training and implementing new technologies. As a result, the facilities reported higher patient satisfaction scores and improved health outcomes, demonstrating that with the right approach, private equity can positively impact care quality.
Regulatory Oversight and Accountability
The regulatory environment plays a crucial role in ensuring that disability care centers maintain high standards of care, regardless of ownership structure. However, the rapid growth of private equity in this sector has raised questions about the adequacy of existing regulations.
Regulatory bodies must adapt to the changing landscape by implementing stricter oversight and accountability measures for facilities owned by private equity firms. This includes regular inspections, transparency in financial reporting, and requirements for maintaining staffing levels that meet the needs of residents.
Financial Motivations Behind Private Equity Acquisitions
Understanding the financial motivations behind private equity acquisitions of disability care centers is essential for grasping the broader implications of this trend. Private equity firms typically seek to generate high returns on their investments, and the healthcare sector offers several avenues for achieving this goal.
Return on Investment (ROI) Expectations
Private equity firms often target industries with predictable cash flows and growth potential, making disability care centers an attractive investment. The steady demand for care services provides a reliable revenue stream, which is appealing to investors looking for stable returns.
Moreover, private equity firms often employ leverage to finance their acquisitions, allowing them to amplify their returns. By using borrowed funds to acquire facilities, they can increase their equity stake and potentially achieve higher returns when they eventually sell the investment. However, this approach also carries risks, particularly if the facilities do not perform as expected.
Cost-Cutting Strategies
To enhance profitability, private equity firms may implement cost-cutting strategies that can impact care quality. These strategies can include reducing staffing levels, renegotiating supplier contracts, and minimizing capital expenditures on facility upgrades. While these measures can improve short-term financial performance, they may also lead to negative consequences for residents and staff.
For example, a study published in the Journal of Health Economics found that nursing homes owned by private equity firms often experience higher rates of staff turnover and lower employee satisfaction. This can create a cycle of instability that ultimately affects the quality of care provided to residents.
Exit Strategies and Market Timing
Private equity firms typically have a defined investment horizon, often ranging from three to seven years. During this period, they focus on enhancing the value of their portfolio companies to prepare for a profitable exit, whether through a sale to another firm or an initial public offering (IPO).
The timing of these exits can significantly impact the facilities’ operations. If a private equity firm is nearing the end of its investment horizon, it may prioritize short-term financial gains over long-term sustainability. This can lead to decisions that compromise care quality, as the firm seeks to maximize its return before selling the facility.
The Regulatory Environment and Its Challenges
The regulatory landscape for disability care centers is complex and varies significantly by state and federal guidelines. As private equity firms continue to acquire these facilities, understanding the regulatory challenges they face is crucial for ensuring compliance and maintaining care quality.
Current Regulations and Compliance Issues
Disability care centers are subject to a myriad of regulations designed to protect residents and ensure quality care. These regulations cover various aspects, including staffing ratios, safety standards, and resident rights. However, compliance can be challenging, particularly for facilities undergoing ownership changes.
Private equity acquisitions can lead to disruptions in compliance as new management teams implement changes. For instance, a facility may experience a temporary decline in staffing levels during the transition period, which can raise concerns about compliance with state and federal regulations.
Advocacy for Stronger Regulations
As the trend of private equity acquisitions continues, advocacy groups are calling for stronger regulations to protect residents in disability care centers. These groups argue that increased oversight is necessary to ensure that facilities prioritize patient care over profit maximization.
Proposed measures include stricter staffing requirements, enhanced transparency in financial reporting, and regular audits of facilities owned by private equity firms. By advocating for these changes, stakeholders aim to create a regulatory environment that holds all facilities accountable for the quality of care they provide.
The Role of State and Federal Agencies
State and federal agencies play a critical role in regulating disability care centers and ensuring compliance with established standards. However, the rapid growth of private equity in this sector has raised questions about the adequacy of existing oversight mechanisms.
Agencies must adapt to the changing landscape by increasing their capacity for monitoring and enforcement. This may involve hiring additional inspectors, implementing more frequent inspections, and enhancing data collection efforts to track facility performance over time.
The Future Outlook for Disability Care Centers
The future of disability care centers in the context of private equity acquisitions is uncertain, with both opportunities and challenges on the horizon. As the demand for specialized care continues to grow, private equity firms will likely remain active in this sector.
Potential for Innovation and Improvement
One of the potential benefits of private equity involvement in disability care centers is the opportunity for innovation and improvement. With access to capital and operational expertise, private equity firms can invest in new technologies and best practices that enhance care quality.
For example, telehealth services have gained traction in recent years, allowing disability care centers to provide remote consultations and support. Private equity firms that invest in these technologies can improve access to care and enhance the overall patient experience.
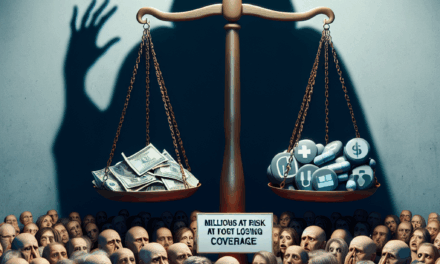
Challenges Ahead: Balancing Profit and Care Quality
Despite the potential for innovation, the challenge remains to balance profit motives with the need for high-quality care. As private equity firms seek to maximize returns, there is a risk that care quality may be compromised in favor of financial gains.
Stakeholders, including families, advocacy groups, and regulatory agencies, must remain vigilant in holding private equity firms accountable for their impact on care quality. This includes advocating for stronger regulations and ensuring that facilities prioritize the well-being of residents.
The Role of Stakeholders in Shaping the Future
The future of disability care centers will depend on the collective efforts of various stakeholders, including private equity firms, regulatory agencies, advocacy groups, and families. Collaboration among these groups can help create a more sustainable and compassionate care environment.
For instance, private equity firms can engage with advocacy groups to better understand the needs of residents and families. By prioritizing patient-centered care, they can enhance their reputation and build trust within the communities they serve.
Conclusion
The surge in private equity acquisitions of disability care centers presents both opportunities and challenges. While private equity involvement can lead to operational improvements and increased efficiency, it also raises concerns about the potential impact on care quality. As the demand for disability care services continues to grow, stakeholders must work together to ensure that facilities prioritize the well-being of residents over profit maximization.
By advocating for stronger regulations, promoting transparency, and fostering collaboration among stakeholders, we can create a future where disability care centers provide high-quality, compassionate care for all individuals. The path forward will require vigilance and commitment from all parties involved, but with the right approach, it is possible to achieve a balance between financial sustainability and exceptional care.