Severe Mental Illness Increases Mortality Risk from Respiratory Infections Threefold
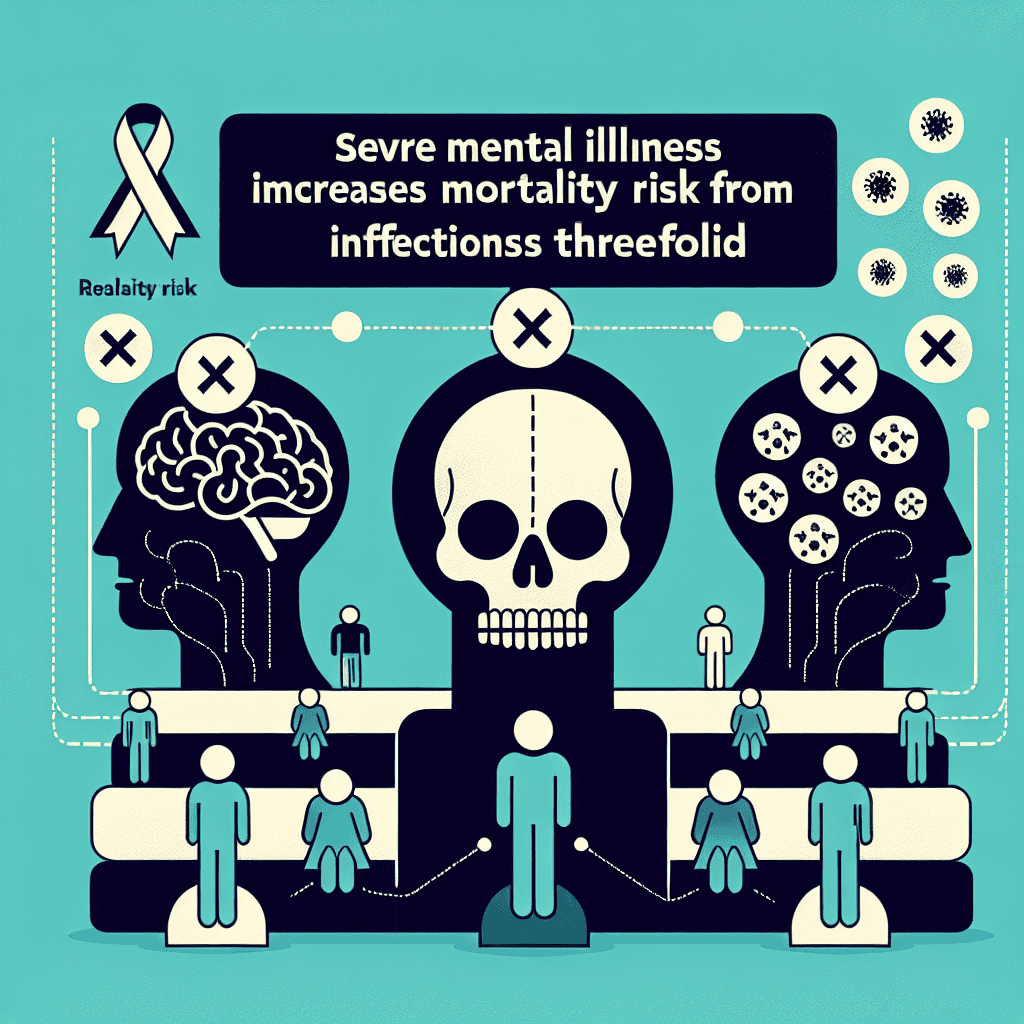
Severe mental illness (SMI) encompasses a range of psychiatric disorders that significantly impair an individual’s ability to function in daily life. These disorders include schizophrenia, bipolar disorder, and major depressive disorder, among others. Recent research has highlighted a concerning link between SMI and an increased risk of mortality from respiratory infections. This article delves into the multifaceted relationship between SMI and respiratory health, exploring the underlying mechanisms, the impact of healthcare disparities, and potential interventions to mitigate this risk.
Understanding Severe Mental Illness and Its Impact on Physical Health
Severe mental illness is characterized by chronic and debilitating psychiatric conditions that affect a person’s thoughts, emotions, and behaviors. These disorders often require long-term treatment and can lead to significant impairments in social and occupational functioning. The impact of SMI extends beyond mental health, as individuals with these conditions frequently experience poorer physical health outcomes compared to the general population.
One of the primary reasons for the increased physical health burden in individuals with SMI is the presence of comorbid conditions. People with SMI are more likely to suffer from chronic diseases such as diabetes, cardiovascular disease, and respiratory illnesses. These comorbidities can be attributed to a combination of factors, including lifestyle choices, medication side effects, and limited access to healthcare services.
Moreover, the stigma associated with mental illness often leads to social isolation and reduced access to healthcare resources. This can result in delayed diagnosis and treatment of physical health conditions, further exacerbating the health disparities faced by individuals with SMI. Understanding the complex interplay between mental and physical health is crucial for developing effective interventions to improve the overall well-being of this vulnerable population.
The Link Between Severe Mental Illness and Respiratory Infections
Respiratory infections, including pneumonia and influenza, are a significant cause of morbidity and mortality worldwide. Individuals with SMI are particularly vulnerable to these infections, with studies indicating a threefold increase in mortality risk compared to the general population. Several factors contribute to this heightened risk, including compromised immune function, lifestyle factors, and healthcare access issues.
Research suggests that individuals with SMI may have an impaired immune response, making them more susceptible to infections. This immune dysfunction can be attributed to both the physiological effects of mental illness and the impact of psychotropic medications. For instance, antipsychotic medications, commonly prescribed for conditions like schizophrenia, have been associated with an increased risk of respiratory infections due to their immunosuppressive effects.
Lifestyle factors also play a significant role in the increased risk of respiratory infections among individuals with SMI. High rates of smoking, poor nutrition, and sedentary behavior are prevalent in this population, all of which can compromise respiratory health. Additionally, individuals with SMI may face barriers to accessing preventive healthcare services, such as vaccinations, further increasing their vulnerability to respiratory infections.
Healthcare Disparities and Their Role in Increased Mortality Risk
Healthcare disparities are a critical factor contributing to the increased mortality risk from respiratory infections in individuals with SMI. These disparities manifest in various forms, including limited access to healthcare services, inadequate treatment of physical health conditions, and a lack of integration between mental and physical healthcare.
Individuals with SMI often face significant barriers to accessing healthcare services, including financial constraints, transportation issues, and stigma. These barriers can lead to delayed or inadequate treatment of respiratory infections, increasing the risk of severe outcomes. Furthermore, healthcare providers may prioritize mental health treatment over physical health concerns, resulting in suboptimal management of comorbid conditions.
The lack of integration between mental and physical healthcare services further exacerbates these disparities. Many healthcare systems operate in silos, with separate providers for mental and physical health. This fragmentation can lead to gaps in care and a lack of coordination between providers, ultimately impacting the quality of care received by individuals with SMI.
Case Studies and Real-World Examples
To illustrate the impact of SMI on respiratory health, consider the case of John, a 45-year-old man with schizophrenia. John has a history of smoking and poor adherence to medical appointments due to his mental health condition. Despite experiencing symptoms of a respiratory infection, John delays seeking medical care, resulting in a severe case of pneumonia that requires hospitalization. This scenario highlights the challenges faced by individuals with SMI in accessing timely and appropriate healthcare.
Another example is Sarah, a 30-year-old woman with bipolar disorder. Sarah’s condition is managed with a combination of mood stabilizers and antipsychotic medications. However, these medications have side effects that impact her immune function, making her more susceptible to respiratory infections. Sarah’s case underscores the need for careful monitoring and management of medication side effects in individuals with SMI.
These case studies demonstrate the complex interplay between mental illness, lifestyle factors, and healthcare access in determining respiratory health outcomes. They also highlight the importance of addressing these factors through targeted interventions and policy changes.
Interventions and Strategies to Mitigate Risk
Addressing the increased mortality risk from respiratory infections in individuals with SMI requires a multifaceted approach. Interventions should focus on improving access to healthcare, promoting healthy lifestyle choices, and enhancing the integration of mental and physical healthcare services.
One potential strategy is to implement integrated care models that provide comprehensive and coordinated care for individuals with SMI. These models involve collaboration between mental health and primary care providers, ensuring that both mental and physical health needs are addressed. Integrated care can improve health outcomes by facilitating early detection and treatment of respiratory infections and other comorbid conditions.
Promoting healthy lifestyle choices is another critical component of risk mitigation. Public health initiatives should focus on reducing smoking rates, improving nutrition, and encouraging physical activity among individuals with SMI. These efforts can help improve respiratory health and reduce the risk of infections.
Finally, increasing access to preventive healthcare services, such as vaccinations, is essential for reducing the incidence of respiratory infections in this population. Healthcare providers should prioritize vaccination efforts and ensure that individuals with SMI receive appropriate preventive care.
Conclusion
The increased mortality risk from respiratory infections in individuals with severe mental illness is a pressing public health concern. This article has explored the complex relationship between SMI and respiratory health, highlighting the role of immune dysfunction, lifestyle factors, and healthcare disparities in driving this risk. By implementing targeted interventions and promoting integrated care models, we can improve health outcomes for individuals with SMI and reduce the burden of respiratory infections. Addressing these challenges requires a concerted effort from healthcare providers, policymakers, and public health organizations to ensure that individuals with SMI receive the comprehensive care they need to thrive.