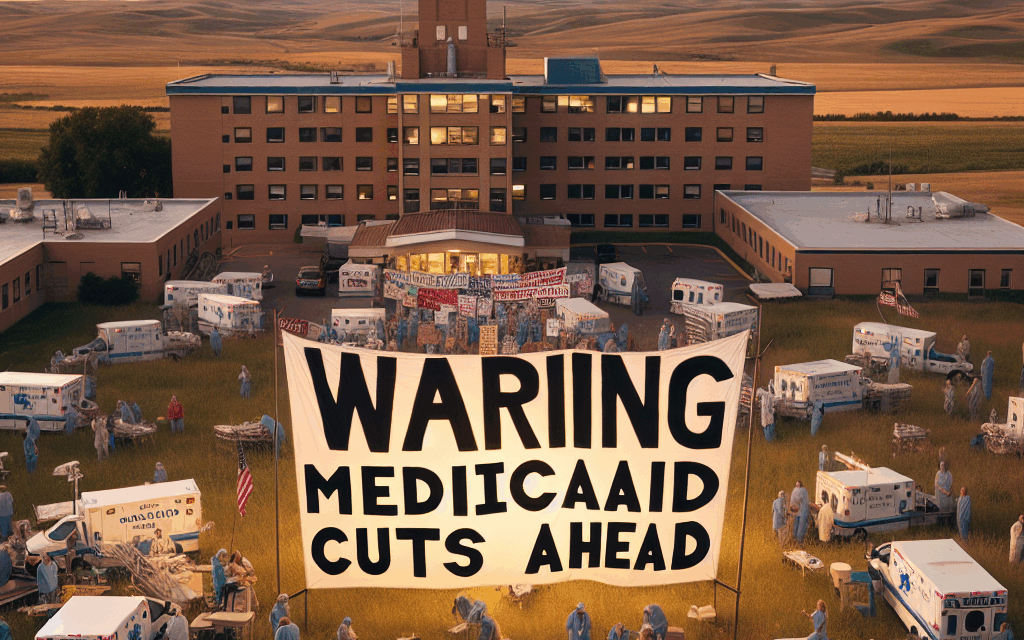
Rural Hospitals Face Crisis as Democrats Warn of Medicaid Cuts
Rural hospitals are a critical component of the healthcare system in the United States, providing essential services to communities that often lack access to larger medical facilities. However, these institutions are facing an unprecedented crisis as political discussions around Medicaid cuts intensify. With Democrats warning of potential reductions in funding, the implications for rural healthcare could be dire. This article explores the multifaceted challenges facing rural hospitals, the potential impact of Medicaid cuts, and the broader implications for public health.
The Importance of Rural Hospitals
Rural hospitals serve as the backbone of healthcare in many underserved areas, providing a range of services from emergency care to maternity services. Their importance cannot be overstated, as they often serve populations that are older, poorer, and sicker than their urban counterparts.
- Access to Care: Rural hospitals are often the only healthcare providers within a significant radius. For many residents, these facilities are their first point of contact with the healthcare system.
- Emergency Services: In emergencies, timely access to care can be a matter of life and death. Rural hospitals provide critical emergency services that can stabilize patients before they are transferred to larger facilities.
- Preventive Care: These hospitals also play a vital role in preventive care, offering screenings and vaccinations that can help reduce the incidence of chronic diseases.
- Economic Impact: Rural hospitals are significant employers in their communities, providing jobs and supporting local economies.
- Community Health Initiatives: Many rural hospitals engage in community health initiatives that address local health disparities and promote wellness.
Despite their importance, rural hospitals are facing numerous challenges, including financial instability, workforce shortages, and increasing operational costs. The potential for Medicaid cuts adds another layer of complexity to an already precarious situation.
The Financial Strain on Rural Hospitals
Financial challenges are a significant concern for rural hospitals, many of which operate on thin margins. The combination of low patient volumes, high operational costs, and reliance on government funding creates a precarious financial environment.
- Low Patient Volume: Rural hospitals often serve fewer patients than urban hospitals, leading to lower revenue. This can make it difficult to cover fixed costs such as salaries and equipment maintenance.
- High Operational Costs: The cost of providing care in rural areas can be higher due to factors such as transportation, staffing, and the need for specialized equipment.
- Medicaid Dependency: Many rural hospitals rely heavily on Medicaid reimbursements, which can be lower than private insurance payments. This dependency makes them vulnerable to changes in Medicaid funding.
- Uncompensated Care: Rural hospitals often provide care to uninsured patients, leading to uncompensated care costs that further strain their finances.
- Declining Reimbursements: Over the years, reimbursement rates from both Medicare and Medicaid have declined, putting additional financial pressure on rural hospitals.
According to the American Hospital Association, nearly 50% of rural hospitals are operating at a loss. This financial instability can lead to service reductions, layoffs, and even closures, which would have devastating effects on rural communities.
The Potential Impact of Medicaid Cuts
Medicaid is a crucial source of funding for rural hospitals, covering a significant portion of their patient population. As discussions around potential cuts to Medicaid funding gain traction, the implications for rural healthcare are alarming.
- Reduced Access to Care: Cuts to Medicaid could lead to reduced services at rural hospitals, making it more difficult for residents to access necessary care.
- Increased Financial Strain: With fewer reimbursements, rural hospitals may struggle to maintain operations, leading to layoffs and service reductions.
- Impact on Vulnerable Populations: Rural populations often include low-income individuals and families who rely on Medicaid for their healthcare needs. Cuts could disproportionately affect these vulnerable groups.
- Potential Closures: The financial strain from Medicaid cuts could lead to the closure of rural hospitals, leaving communities without essential healthcare services.
- Long-term Health Consequences: Reduced access to care can lead to worse health outcomes, increased hospitalizations, and higher long-term healthcare costs.
For example, a study by the North Carolina Rural Health Research Program found that rural hospitals that experienced Medicaid payment cuts saw a significant increase in emergency room visits and hospitalizations for preventable conditions. This highlights the critical role that Medicaid plays in maintaining the health of rural populations.
Political Landscape and Medicaid Funding
The political landscape surrounding Medicaid funding is complex and often contentious. As Democrats warn of potential cuts, the debate over healthcare funding continues to evolve.
- Partisan Divides: The issue of Medicaid funding often falls along partisan lines, with Democrats generally advocating for expanded access and Republicans focusing on budgetary constraints.
- State-Level Decisions: Medicaid is administered at the state level, leading to variations in funding and access across the country. Some states have expanded Medicaid under the Affordable Care Act, while others have not.
- Advocacy Efforts: Various advocacy groups are working to protect Medicaid funding, emphasizing its importance for rural healthcare and the overall health of communities.
- Public Opinion: Public support for Medicaid expansion remains strong, particularly in rural areas where residents understand the importance of access to care.
- Future Proposals: As political discussions continue, proposals for Medicaid reform and funding will likely emerge, impacting the future of rural healthcare.
The political discourse surrounding Medicaid funding is critical, as it shapes the future of healthcare access for millions of Americans. Understanding the implications of these discussions is essential for stakeholders in rural healthcare.
Case Studies: Rural Hospitals in Crisis
To illustrate the impact of financial strain and potential Medicaid cuts, several case studies of rural hospitals facing crisis situations provide valuable insights.
- Case Study 1: Rural Hospital Closure in Texas – In 2018, a rural hospital in Texas closed its doors due to financial instability exacerbated by Medicaid payment cuts. The closure left the community without emergency services, forcing residents to travel over an hour for care.
- Case Study 2: Innovative Solutions in Nebraska – A rural hospital in Nebraska implemented telehealth services to expand access to care and reduce costs. This innovative approach helped the hospital remain financially viable while serving its community.
- Case Study 3: Community Health Initiatives in Kentucky – A rural hospital in Kentucky partnered with local organizations to address health disparities through community health initiatives. These efforts not only improved health outcomes but also strengthened the hospital’s financial position.
- Case Study 4: The Role of Federal Funding – A rural hospital in West Virginia received federal funding to improve its facilities and expand services. This funding was crucial in preventing closure and ensuring continued access to care for the community.
- Case Study 5: The Impact of COVID-19 – The COVID-19 pandemic has further strained rural hospitals, with many facing increased costs and decreased revenues. A case study of a rural hospital in Idaho highlights the challenges faced during the pandemic and the ongoing need for support.
These case studies underscore the diverse challenges and innovative solutions that rural hospitals are employing to navigate the current crisis. They also highlight the urgent need for policy changes to support these vital institutions.
Conclusion: The Path Forward for Rural Hospitals
The crisis facing rural hospitals is a multifaceted issue that requires urgent attention from policymakers, healthcare providers, and communities. As discussions around Medicaid cuts continue, it is essential to recognize the critical role that rural hospitals play in the healthcare system.
- Advocacy for Funding: Continued advocacy for Medicaid funding is crucial to ensure that rural hospitals can maintain operations and provide essential services.
- Innovative Solutions: Embracing innovative solutions such as telehealth and community partnerships can help rural hospitals navigate financial challenges.
- Public Awareness: Raising public awareness about the importance of rural healthcare can mobilize support for policies that protect these institutions.
- Collaboration: Collaboration between rural hospitals, local governments, and community organizations can strengthen healthcare delivery and improve health outcomes.
- Long-term Planning: Developing long-term strategies for sustainability and resilience will be essential for the future of rural healthcare.
In summary, the potential for Medicaid cuts poses a significant threat to rural hospitals and the communities they serve. By understanding the challenges and advocating for necessary changes, stakeholders can work together to ensure that rural healthcare remains accessible and sustainable for future generations.