Revolutionizing Surgery: How AI Enhances Scheduling and Operating Room Efficiency
The integration of artificial intelligence (AI) into healthcare has been a game-changer, particularly in the realm of surgery. As hospitals and surgical centers strive to improve patient outcomes while managing costs, AI technologies are emerging as vital tools for enhancing scheduling and operating room efficiency. This article delves into the multifaceted ways AI is transforming surgical practices, focusing on five key areas: predictive analytics for scheduling, real-time data management, resource allocation, patient flow optimization, and the future of AI in surgical environments.
1. Predictive Analytics for Scheduling
One of the most significant challenges in surgical settings is the efficient scheduling of procedures. Traditional scheduling methods often lead to bottlenecks, delays, and underutilization of operating rooms. AI-driven predictive analytics can revolutionize this process by analyzing historical data to forecast surgical needs accurately.
Predictive analytics utilizes algorithms that process vast amounts of data, including patient demographics, historical surgery times, and even seasonal trends in surgical demand. By leveraging this data, hospitals can create more accurate schedules that minimize downtime and maximize the use of operating rooms.
- Data-Driven Decision Making: AI systems can analyze past surgical data to identify patterns and predict future needs. For instance, if a hospital notices an increase in orthopedic surgeries during winter months, it can allocate more resources during that time.
- Reduced Wait Times: By accurately predicting the number of surgeries needed, hospitals can reduce patient wait times significantly. A study published in the Journal of Surgical Research found that hospitals using AI for scheduling reduced patient wait times by up to 30%.
- Improved Patient Satisfaction: Shorter wait times and more efficient scheduling lead to higher patient satisfaction rates. Patients are more likely to recommend facilities that respect their time and provide timely care.
For example, the University of California, San Francisco (UCSF) implemented an AI-based scheduling system that reduced surgical delays by 25%. By analyzing historical data and real-time variables, the system could adjust schedules dynamically, ensuring that operating rooms were utilized effectively.
Moreover, predictive analytics can also help in managing cancellations and rescheduling. By identifying patients at higher risk of cancellation based on historical data, hospitals can proactively reach out to these patients to confirm their appointments, thereby reducing last-minute cancellations and optimizing the surgical schedule.
2. Real-Time Data Management
In the fast-paced environment of an operating room, real-time data management is crucial for ensuring that surgical teams have access to the information they need when they need it. AI technologies can facilitate this by integrating various data sources and providing actionable insights in real time.
AI systems can pull data from electronic health records (EHRs), imaging systems, and even wearable devices to provide a comprehensive view of a patient’s health status. This integration allows surgical teams to make informed decisions quickly, which is vital during complex procedures.
- Enhanced Communication: AI can streamline communication among surgical team members by providing a centralized platform for sharing information. This reduces the chances of miscommunication and ensures that everyone is on the same page.
- Real-Time Monitoring: AI can monitor vital signs and other critical parameters during surgery, alerting the surgical team to any abnormalities. For instance, systems like the OR Black Box can analyze audio and video data from surgeries to provide insights into team performance and patient safety.
- Data-Driven Adjustments: If unexpected complications arise during surgery, AI can analyze real-time data to suggest alternative approaches or interventions, enhancing the surgical team’s ability to respond effectively.
A case study at the Cleveland Clinic demonstrated the effectiveness of real-time data management. By implementing an AI system that integrated EHRs and surgical data, the clinic improved surgical outcomes and reduced complications by 15%. Surgeons had access to real-time data on patient vitals and surgical history, allowing them to make informed decisions during procedures.
Furthermore, AI can assist in post-operative care by analyzing data from the operating room and predicting potential complications. This proactive approach can lead to better patient outcomes and reduced readmission rates.
3. Resource Allocation
Efficient resource allocation is critical in surgical settings, where the availability of staff, equipment, and facilities can significantly impact patient care. AI can optimize resource allocation by analyzing data to ensure that the right resources are available at the right time.
AI systems can assess the availability of surgical instruments, staff schedules, and operating room availability to create a comprehensive resource management plan. This ensures that surgical teams have everything they need to perform procedures without unnecessary delays.
- Optimized Staff Scheduling: AI can analyze staff availability and skill sets to create optimal schedules that ensure the right personnel are present for each surgery. This reduces the likelihood of last-minute staffing issues that can delay procedures.
- Equipment Management: AI can track the usage of surgical instruments and equipment, alerting staff when maintenance is needed or when supplies are running low. This proactive approach minimizes downtime due to equipment failure.
- Cost Efficiency: By optimizing resource allocation, hospitals can reduce operational costs. A study by the American College of Surgeons found that hospitals using AI for resource management saw a 20% reduction in operational costs.
An example of effective resource allocation through AI can be seen at Mount Sinai Health System, which implemented an AI-driven resource management system. The system analyzed historical data to predict surgical needs and allocate resources accordingly, resulting in a 30% increase in operating room utilization.
Moreover, AI can assist in managing surgical supply chains, ensuring that necessary materials are available when needed. This is particularly important in high-demand surgical environments where delays in supplies can lead to postponed surgeries and increased costs.
4. Patient Flow Optimization
Patient flow optimization is essential for ensuring that surgical patients receive timely care while minimizing delays and bottlenecks in the system. AI can play a pivotal role in streamlining patient flow from pre-operative assessments to post-operative recovery.
AI systems can analyze patient data to predict flow patterns, helping hospitals manage patient admissions and discharges more effectively. By understanding peak times for surgeries and patient arrivals, hospitals can allocate resources accordingly and reduce congestion.
- Pre-Operative Assessments: AI can streamline the pre-operative assessment process by analyzing patient data to identify potential risks and necessary evaluations. This ensures that patients are adequately prepared for surgery, reducing the likelihood of cancellations.
- Post-Operative Care: AI can monitor patients in recovery, analyzing vital signs and other data to identify any complications early. This proactive approach can lead to quicker interventions and improved patient outcomes.
- Discharge Planning: AI can assist in discharge planning by analyzing patient recovery data and predicting when patients are ready to leave the hospital. This helps to free up beds for incoming patients and reduces wait times.
A notable example of patient flow optimization through AI is the implementation of an AI-driven patient management system at Johns Hopkins Hospital. The system analyzed patient data to predict flow patterns, resulting in a 40% reduction in patient wait times for surgeries.
Additionally, AI can enhance communication between departments, ensuring that surgical teams are aware of patient statuses and any changes in schedules. This improved communication can lead to more efficient patient flow and better overall care.
5. The Future of AI in Surgical Environments
The future of AI in surgical environments is promising, with ongoing advancements in technology and data analytics. As AI continues to evolve, its applications in surgery are expected to expand, leading to even greater efficiencies and improved patient outcomes.
Emerging technologies such as machine learning and natural language processing are paving the way for more sophisticated AI systems that can analyze complex data sets and provide actionable insights. These advancements will enable surgical teams to make more informed decisions and enhance the overall quality of care.
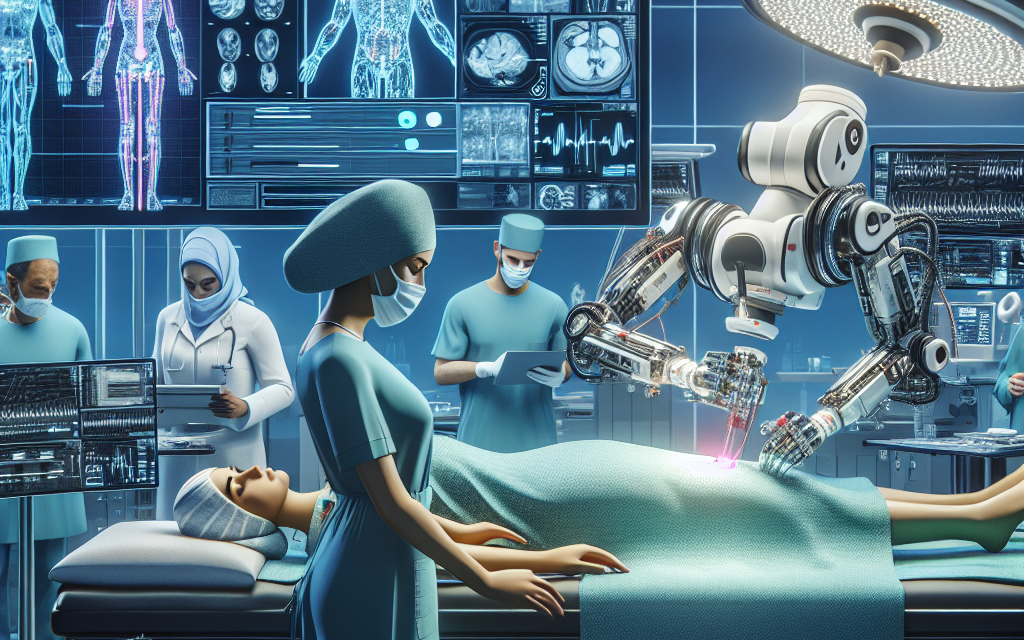
- Robotic Surgery: The integration of AI with robotic surgery systems is expected to revolutionize surgical procedures. AI can enhance the precision and accuracy of robotic systems, leading to minimally invasive surgeries with faster recovery times.
- Telemedicine and Remote Surgery: AI can facilitate telemedicine and remote surgery by providing real-time data and analytics to surgeons operating from different locations. This could expand access to surgical care in underserved areas.
- Personalized Medicine: AI can analyze genetic and health data to tailor surgical approaches to individual patients, leading to more personalized and effective treatments.
As hospitals continue to adopt AI technologies, it is essential to address challenges such as data privacy, ethical considerations, and the need for ongoing training for healthcare professionals. Ensuring that surgical teams are equipped to work alongside AI systems will be crucial for maximizing their potential benefits.
Conclusion
The integration of AI into surgical practices is revolutionizing the way surgeries are scheduled and conducted. From predictive analytics that enhance scheduling efficiency to real-time data management that supports informed decision-making, AI is proving to be an invaluable asset in the operating room. By optimizing resource allocation and improving patient flow, AI is helping hospitals provide better care while reducing costs.
As we look to the future, the potential for AI in surgical environments is vast. With advancements in technology and ongoing research, we can expect to see even more innovative applications that will further enhance surgical efficiency and patient outcomes. Embracing these changes will be essential for healthcare providers aiming to stay at the forefront of surgical excellence.
In summary, AI is not just a tool; it is a transformative force that is reshaping the landscape of surgery. By harnessing its capabilities, healthcare providers can improve operational efficiency, enhance patient care, and ultimately save lives.