-
Table of Contents
- Regenerative Medicine: The Future of Healing and Organ Replacement
- The Principles of Regenerative Medicine
- Stem Cell Therapy
- Tissue Engineering
- Biomaterials
- Applications of Regenerative Medicine
- Organ Transplantation
- Wound Healing
- Degenerative Diseases
- Challenges in Regenerative Medicine
- Technical Challenges
- Ethical Challenges
- Regulatory Challenges
Regenerative Medicine: The Future of Healing and Organ Replacement
Regenerative medicine is a rapidly evolving field that holds the promise of revolutionizing the way we approach healing and organ replacement. By harnessing the body’s natural ability to repair and regenerate, this innovative branch of medicine aims to restore function to damaged tissues and organs, offering hope to millions of patients worldwide. In this article, we will explore the various facets of regenerative medicine, including its principles, applications, challenges, and future prospects.
The Principles of Regenerative Medicine
At its core, regenerative medicine is based on the concept of using the body’s own mechanisms to heal and regenerate damaged tissues. This approach contrasts with traditional medicine, which often focuses on treating symptoms rather than addressing the underlying causes of disease. The principles of regenerative medicine can be broadly categorized into three main areas: stem cell therapy, tissue engineering, and biomaterials.
Stem Cell Therapy
Stem cells are the building blocks of regenerative medicine. These undifferentiated cells have the unique ability to develop into various cell types, making them invaluable for repairing damaged tissues. There are two primary types of stem cells used in regenerative medicine: embryonic stem cells and adult stem cells.
Embryonic stem cells are derived from early-stage embryos and have the potential to differentiate into any cell type in the body. However, their use is often controversial due to ethical concerns. Adult stem cells, on the other hand, are found in various tissues throughout the body and are responsible for maintaining and repairing those tissues. They are less versatile than embryonic stem cells but are more widely accepted for therapeutic use.
Recent advancements in stem cell research have led to the development of induced pluripotent stem cells (iPSCs), which are adult cells reprogrammed to behave like embryonic stem cells. This breakthrough has opened new avenues for regenerative medicine, as iPSCs can be generated from a patient’s own cells, reducing the risk of immune rejection.
Tissue Engineering
Tissue engineering involves the creation of artificial tissues and organs using a combination of cells, scaffolds, and growth factors. This approach aims to replace or repair damaged tissues by providing a supportive environment for cell growth and differentiation.
Scaffolds are three-dimensional structures that mimic the extracellular matrix, providing a framework for cells to attach and grow. These scaffolds can be made from natural or synthetic materials and are often designed to degrade over time as the new tissue forms.
Growth factors are signaling molecules that regulate cell behavior, such as proliferation, differentiation, and migration. By incorporating growth factors into tissue-engineered constructs, researchers can enhance the regenerative potential of these therapies.
Biomaterials
Biomaterials play a crucial role in regenerative medicine by providing structural support and facilitating cell interactions. These materials can be natural, such as collagen or hyaluronic acid, or synthetic, such as polymers or ceramics.
The choice of biomaterial depends on the specific application and desired properties, such as biocompatibility, biodegradability, and mechanical strength. Advances in biomaterials research have led to the development of smart materials that can respond to environmental cues, such as changes in temperature or pH, to enhance their regenerative potential.
Applications of Regenerative Medicine
Regenerative medicine has the potential to transform the treatment of a wide range of diseases and injuries. Some of the most promising applications include organ transplantation, wound healing, and the treatment of degenerative diseases.
Organ Transplantation
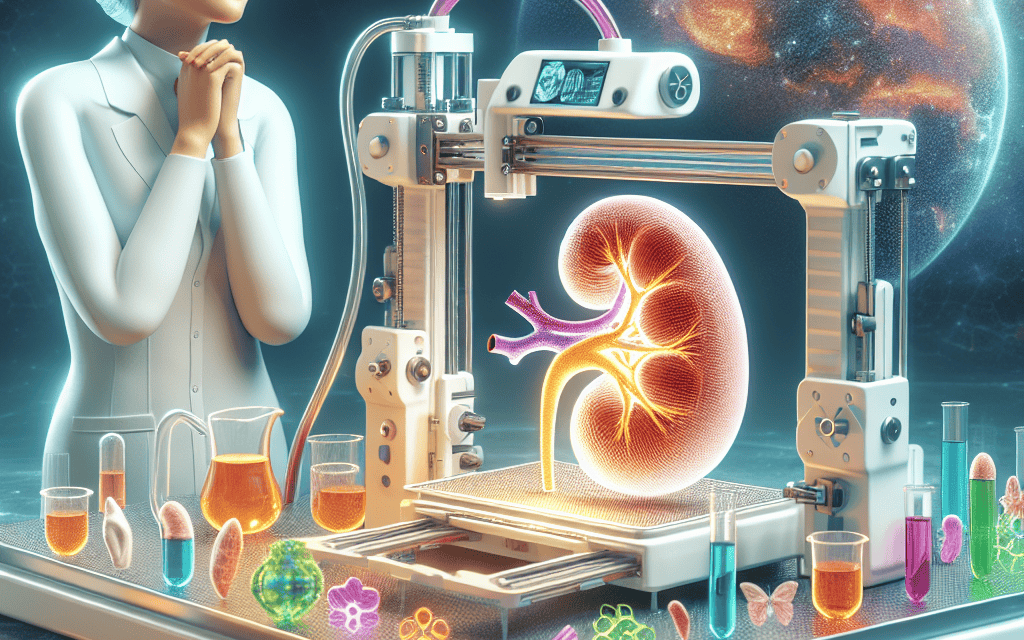
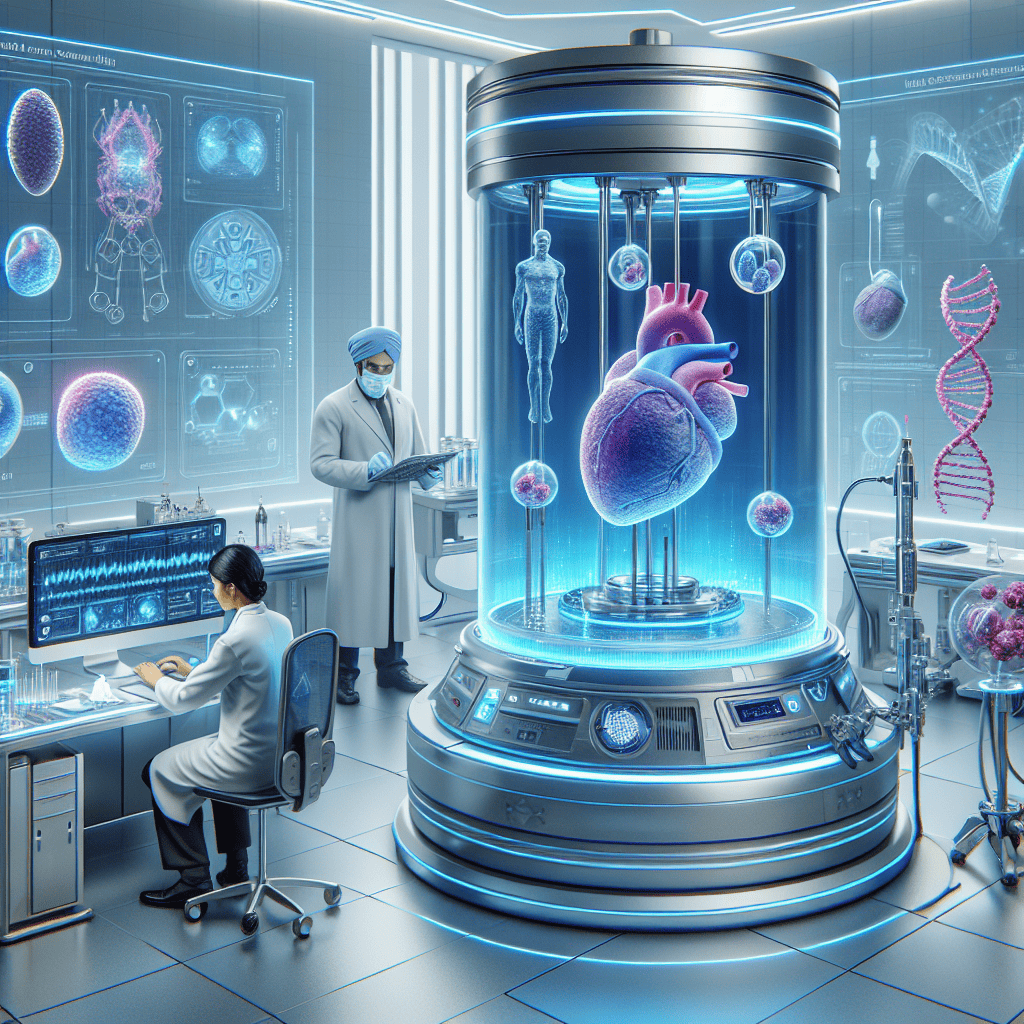
One of the most significant challenges in organ transplantation is the shortage of donor organs. Regenerative medicine offers a potential solution by enabling the growth of functional organs in the laboratory. This approach could eliminate the need for donor organs and reduce the risk of immune rejection.
Researchers have made significant progress in developing bioengineered organs, such as kidneys, livers, and hearts, using a combination of stem cells, scaffolds, and growth factors. While these organs are not yet ready for clinical use, they represent a promising avenue for addressing the organ shortage crisis.
Wound Healing
Chronic wounds, such as diabetic ulcers and pressure sores, are a significant burden on healthcare systems and can lead to severe complications if left untreated. Regenerative medicine offers new strategies for promoting wound healing by enhancing the body’s natural repair processes.
Stem cell therapy has shown promise in accelerating wound healing by promoting the formation of new blood vessels and reducing inflammation. Additionally, tissue-engineered skin substitutes, which consist of scaffolds seeded with skin cells, have been developed to provide a temporary cover for wounds and promote healing.
Degenerative Diseases
Degenerative diseases, such as Parkinson’s disease, Alzheimer’s disease, and osteoarthritis, are characterized by the progressive loss of function in specific tissues or organs. Regenerative medicine offers the potential to halt or even reverse the progression of these diseases by replacing damaged cells and tissues.
For example, stem cell therapy has shown promise in treating Parkinson’s disease by replacing the dopamine-producing neurons that are lost in the disease. Similarly, tissue engineering approaches are being explored for the regeneration of cartilage in osteoarthritis patients.
Challenges in Regenerative Medicine
Despite its potential, regenerative medicine faces several challenges that must be addressed before it can become a mainstream treatment option. These challenges include technical, ethical, and regulatory issues.
Technical Challenges
One of the primary technical challenges in regenerative medicine is the complexity of replicating the intricate structure and function of human tissues and organs. While significant progress has been made in developing simple tissues, such as skin and cartilage, more complex organs, such as the heart and liver, present significant challenges.
Another technical challenge is ensuring the long-term survival and integration of transplanted cells and tissues. Immune rejection remains a significant barrier to the success of regenerative therapies, particularly when using allogeneic (donor-derived) cells.
Ethical Challenges
The use of embryonic stem cells in regenerative medicine raises ethical concerns related to the destruction of human embryos. While the development of iPSCs has alleviated some of these concerns, ethical issues remain regarding the potential for genetic manipulation and the creation of human-animal chimeras.
Additionally, the commercialization of regenerative therapies raises questions about access and equity. Ensuring that these treatments are available to all patients, regardless of socioeconomic status, is a critical ethical consideration.
Regulatory Challenges
The regulatory landscape for regenerative medicine is complex and varies significantly between countries. In the United States, the Food and Drug Administration (FDA) regulates regenerative therapies as biologics, drugs, or medical devices, depending on their composition and intended use.
Regulatory challenges include ensuring the safety and efficacy of regenerative therapies, particularly given the rapid pace of innovation in the field. Balancing the need for rigorous testing with the desire to bring new treatments to patients