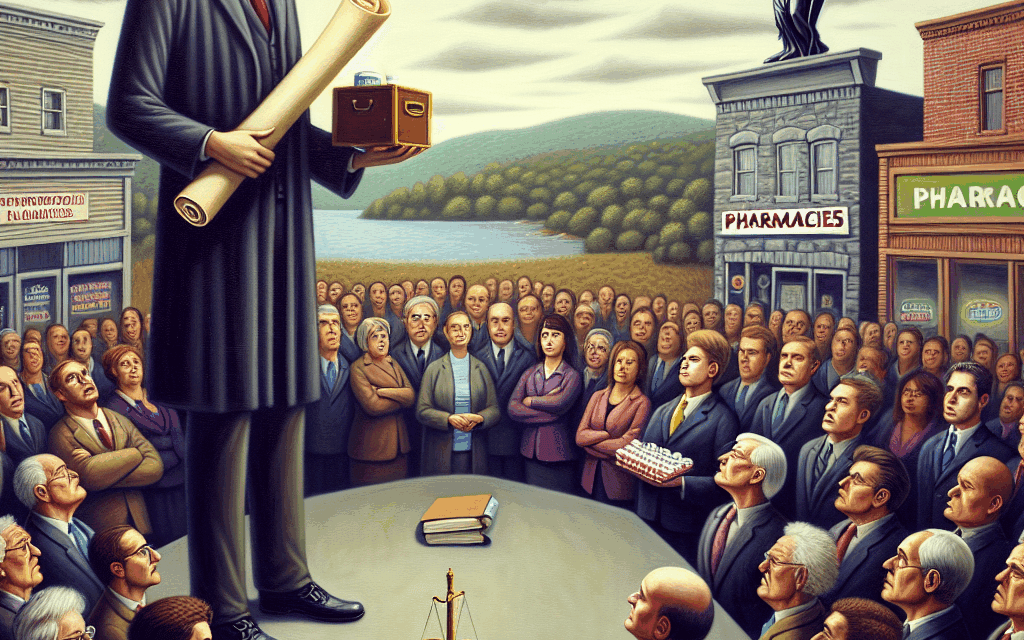
PBM Lobby Challenges Arkansas Law Mandating Drug Middlemen to Sell to Pharmacies
The landscape of prescription drug pricing in the United States is complex and often contentious, particularly when it comes to the role of Pharmacy Benefit Managers (PBMs). In Arkansas, a new law aimed at regulating these drug middlemen has sparked significant debate and legal challenges. This article delves into the intricacies of the Arkansas law, the role of PBMs, the implications of the law, and the ongoing challenges posed by the PBM lobby. We will explore the following subtopics in detail:
- The Role of Pharmacy Benefit Managers in the Drug Supply Chain
- Overview of the Arkansas Law Mandating PBM Sales to Pharmacies
- Legal Challenges and Responses from the PBM Lobby
- Impact of the Law on Drug Pricing and Access to Medications
- Future Implications for PBMs and State Legislation
The Role of Pharmacy Benefit Managers in the Drug Supply Chain
Pharmacy Benefit Managers (PBMs) serve as intermediaries between insurers, pharmacies, and drug manufacturers. Their primary role is to manage prescription drug benefits on behalf of health insurers, aiming to control costs and improve the quality of care. However, their operations have come under scrutiny for a variety of reasons, including lack of transparency and potential conflicts of interest.
PBMs negotiate discounts and rebates with drug manufacturers, which can significantly influence the prices that consumers pay at the pharmacy counter. They also determine which drugs are covered by insurance plans and at what tier they will be placed, affecting out-of-pocket costs for patients. The following are key functions of PBMs:
- Negotiation of Drug Prices: PBMs leverage their purchasing power to negotiate lower prices from manufacturers, which can lead to substantial savings for insurers and, ideally, for consumers.
- Formulary Management: PBMs create formularies, which are lists of covered medications. They categorize drugs into tiers that dictate co-pays and coverage levels, influencing patient access to medications.
- Pharmacy Network Management: PBMs establish networks of pharmacies that patients can use to fill prescriptions, often negotiating reimbursement rates with these pharmacies.
- Clinical Management Programs: Many PBMs implement programs aimed at improving medication adherence and managing chronic diseases, which can enhance patient outcomes.
- Data Analytics: PBMs utilize data to track prescription trends and outcomes, which can inform their strategies and negotiations.
Despite these functions, PBMs have faced criticism for their lack of transparency. Critics argue that the rebates negotiated by PBMs are not always passed on to consumers, leading to higher out-of-pocket costs. Additionally, the complexity of the drug pricing system can obscure the true cost of medications, making it difficult for patients to understand their financial responsibilities.
In recent years, there has been a growing movement to reform the PBM industry, with advocates calling for greater transparency and accountability. This has led to legislative efforts in various states, including Arkansas, to regulate PBM practices more closely.
Overview of the Arkansas Law Mandating PBM Sales to Pharmacies
In 2021, Arkansas passed a law aimed at increasing transparency and accountability among PBMs. The law mandates that PBMs must sell drugs directly to pharmacies at the same price they charge insurers. This legislation was designed to address concerns about the pricing practices of PBMs and to ensure that pharmacies can compete fairly in the marketplace.
The law arose from a growing recognition that PBMs often exert significant control over drug pricing and distribution, which can disadvantage independent pharmacies. By requiring PBMs to sell drugs to pharmacies at the same price they charge insurers, the law aims to level the playing field and promote competition.
Key provisions of the Arkansas law include:
- Direct Sales Requirement: PBMs must sell drugs to pharmacies at the same price they charge health plans, eliminating the potential for price manipulation.
- Transparency Measures: The law requires PBMs to disclose their pricing structures and any rebates received from manufacturers, promoting greater transparency in drug pricing.
- Protection for Independent Pharmacies: The law aims to protect independent pharmacies from being undercut by larger chains or PBMs that may have more negotiating power.
- Consumer Protections: By promoting competition, the law seeks to lower drug prices for consumers and improve access to medications.
The passage of this law was met with enthusiasm from many independent pharmacists and consumer advocates who viewed it as a necessary step toward reforming the PBM industry. However, it also drew immediate backlash from the PBM lobby, which argued that the law would disrupt the existing drug supply chain and lead to unintended consequences.
Legal Challenges and Responses from the PBM Lobby
Following the enactment of the Arkansas law, the PBM lobby quickly mobilized to challenge its legality. Major PBMs, including CVS Caremark and Express Scripts, filed lawsuits against the state, arguing that the law violates federal regulations and disrupts the established drug distribution system.
The primary legal arguments presented by the PBM lobby include:
- Federal Preemption: PBMs argue that the law conflicts with federal regulations governing the drug supply chain, particularly the Employee Retirement Income Security Act (ERISA), which sets standards for health benefit plans.
- Market Disruption: The PBM lobby contends that the law could lead to market instability, potentially resulting in drug shortages and increased costs for consumers.
- Constitutional Concerns: Some PBMs have raised constitutional arguments, claiming that the law infringes on their rights to conduct business freely and could lead to discriminatory practices against certain companies.
In response to these challenges, Arkansas officials have defended the law as a necessary measure to protect consumers and promote fair competition in the pharmacy market. They argue that the law is designed to address the significant power imbalance between PBMs and independent pharmacies, which has been exacerbated by the lack of transparency in drug pricing.
The legal battles surrounding the Arkansas law have drawn national attention, as they highlight the broader issues of drug pricing and the role of PBMs in the healthcare system. As the case progresses through the courts, it could set important precedents for similar legislation in other states.
Impact of the Law on Drug Pricing and Access to Medications
The Arkansas law mandating PBMs to sell drugs directly to pharmacies has the potential to significantly impact drug pricing and access to medications for consumers. By promoting transparency and competition, the law aims to lower costs and improve access for patients, particularly those who rely on independent pharmacies for their medications.
One of the primary goals of the law is to reduce the overall cost of prescription drugs. By requiring PBMs to sell drugs at the same price they charge insurers, the law seeks to eliminate the hidden markups that can inflate prices for consumers. This could lead to lower co-pays and out-of-pocket expenses for patients, making medications more affordable.
Additionally, the law could enhance access to medications for patients in rural or underserved areas. Independent pharmacies often play a crucial role in providing access to medications in these communities, and by leveling the playing field, the law could help ensure that these pharmacies remain viable options for patients.
However, the impact of the law is not without potential drawbacks. Critics argue that mandating PBM sales to pharmacies could lead to unintended consequences, such as:
- Increased Costs for Insurers: If PBMs are forced to sell drugs at higher prices, insurers may pass these costs onto consumers in the form of higher premiums.
- Potential Drug Shortages: Some experts warn that the law could disrupt the supply chain, leading to shortages of certain medications if PBMs are unable to negotiate favorable terms with manufacturers.
- Market Consolidation: Larger pharmacy chains may be better positioned to absorb any increased costs, potentially leading to further consolidation in the pharmacy market and reduced competition.
As the law is implemented and its effects are monitored, it will be essential to assess its impact on drug pricing and access to medications. Ongoing data collection and analysis will be crucial in determining whether the law achieves its intended goals or if adjustments are needed to address any emerging challenges.
Future Implications for PBMs and State Legislation
The legal challenges to the Arkansas law and its potential implications for PBMs highlight a critical juncture in the ongoing debate over drug pricing and healthcare reform in the United States. As states grapple with the complexities of regulating PBMs, the outcomes of these legal battles could shape future legislation across the country.
Several key trends and implications are emerging from the situation in Arkansas:
- Increased State-Level Regulation: The Arkansas law may inspire other states to pursue similar legislation aimed at regulating PBM practices and promoting transparency in drug pricing.
- Potential for Federal Action: As states take action to address drug pricing issues, there may be increased pressure on federal lawmakers to implement comprehensive reforms at the national level.
- Continued Advocacy for Transparency: Consumer advocates and healthcare organizations are likely to continue pushing for greater transparency in drug pricing, which could lead to further reforms in the PBM industry.
- Impact on Pharmacy Business Models: The evolving regulatory landscape may force pharmacies to adapt their business models in response to changing market dynamics and pricing structures.
- Legal Precedents: The outcomes of the legal challenges in Arkansas could set important precedents for future litigation involving PBMs and state regulations, influencing how similar laws are crafted and enforced.
As the situation unfolds, stakeholders across the healthcare spectrum will be closely monitoring developments in Arkansas and beyond. The ongoing dialogue surrounding PBMs, drug pricing, and access to medications is likely to remain a focal point of healthcare policy discussions in the coming years.
Conclusion
The challenges posed by the PBM lobby against Arkansas’s law mandating drug middlemen to sell directly to pharmacies underscore the complexities of the U.S. healthcare system. As PBMs continue to play a significant role in drug pricing and distribution, the need for transparency and accountability has never been more critical.
The Arkansas law represents a bold step toward reforming the PBM industry and promoting fair competition among pharmacies. While the legal challenges ahead may shape the future of this legislation, the broader implications for drug pricing and access to medications are profound. As states consider similar measures, the outcomes of these efforts will be closely watched by advocates, policymakers, and consumers alike.
Ultimately, the ongoing debate over PBMs and drug pricing highlights the need for a comprehensive approach to healthcare reform that prioritizes transparency, affordability, and access for all patients. As stakeholders continue to navigate this complex landscape, the lessons learned from Arkansas may serve as a valuable guide for future efforts to improve the healthcare system.