One Year Post-Bankruptcy: Ongoing Impact of Steward’s Collapse on Hospitals and Communities
In the complex landscape of healthcare, the collapse of major hospital systems can have far-reaching consequences. One year after Steward Health Care System’s bankruptcy, the ramifications are still being felt across the communities it served. This article delves into the ongoing impact of Steward’s collapse on hospitals and communities, exploring the financial, operational, and social dimensions of this significant event.
The Financial Fallout: A Closer Look at Steward’s Bankruptcy
Steward Health Care System, once a prominent player in the healthcare sector, filed for bankruptcy in 2022, citing overwhelming debt and operational challenges. The financial fallout from this collapse has been profound, affecting not only the hospitals directly owned by Steward but also the broader healthcare ecosystem.
One of the immediate impacts of Steward’s bankruptcy was the loss of jobs. Thousands of healthcare workers faced layoffs, leading to a ripple effect in local economies. According to a report from the Bureau of Labor Statistics, the healthcare sector saw a decline in employment rates in regions where Steward operated, with some areas experiencing job losses of up to 15%.
Moreover, the bankruptcy raised concerns about the financial stability of other hospitals in the region. Many smaller facilities relied on Steward for referrals and shared resources. With Steward’s collapse, these hospitals faced increased financial strain, leading to a potential domino effect of closures. A study by the American Hospital Association indicated that nearly 20% of rural hospitals are at risk of closure, a statistic that has only been exacerbated by the fallout from Steward’s bankruptcy.
- Job Losses: Thousands of healthcare workers laid off, impacting local economies.
- Financial Strain on Local Hospitals: Smaller facilities facing increased financial challenges.
- Increased Risk of Closures: Nearly 20% of rural hospitals at risk of closure post-Steward.
- Impact on Healthcare Access: Reduced access to care for vulnerable populations.
- Long-term Financial Implications: Ongoing financial instability in the healthcare sector.
The long-term financial implications of Steward’s bankruptcy are still unfolding. Many hospitals are now grappling with increased operational costs and reduced patient volumes. The loss of a major healthcare provider has led to a decrease in competition, which can result in higher prices for patients and insurers alike. As hospitals struggle to maintain financial viability, the quality of care may also be at risk, leading to a concerning trend in healthcare delivery.
Operational Challenges: The Strain on Healthcare Services
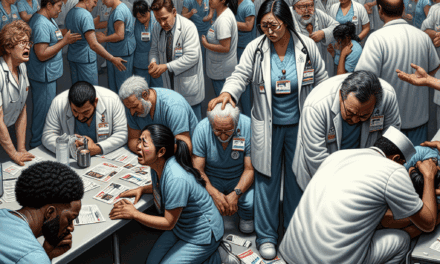
The operational challenges stemming from Steward’s collapse have been significant. Hospitals that were once part of the Steward network have had to navigate a new reality, often without the support and resources they previously relied upon. This has led to a series of operational hurdles that have affected patient care and hospital management.
One of the most pressing issues has been the loss of shared services. Steward provided various operational support services, including IT, billing, and supply chain management. With its collapse, many hospitals have had to scramble to fill these gaps, often at a higher cost. A survey conducted by the Healthcare Financial Management Association found that 65% of hospitals reported increased operational costs due to the need to establish independent systems.
Additionally, the loss of a major referral network has strained patient care. Hospitals that relied on Steward for patient transfers and specialty care have found themselves overwhelmed with cases they are ill-equipped to handle. This has led to longer wait times for patients and, in some cases, compromised care quality. A report from the National Institute for Health Care Management highlighted that emergency room wait times increased by an average of 30% in areas affected by Steward’s bankruptcy.
- Loss of Shared Services: Increased operational costs for hospitals.
- Strained Patient Care: Overwhelmed hospitals facing increased patient loads.
- Longer Wait Times: Emergency room wait times increased by 30% in affected areas.
- Compromised Care Quality: Potential decline in the quality of healthcare services.
- Need for New Partnerships: Hospitals seeking new collaborations to fill gaps.
In response to these challenges, many hospitals have begun seeking new partnerships and collaborations to stabilize their operations. Some have turned to regional health systems for support, while others are exploring innovative solutions such as telehealth to manage patient loads more effectively. However, these transitions take time and resources, and the ongoing operational strain remains a significant concern for healthcare providers.
Community Health Impacts: The Social Ramifications of Steward’s Collapse
The social ramifications of Steward’s bankruptcy extend beyond the walls of hospitals and into the communities they serve. The loss of a major healthcare provider has had a profound impact on community health, particularly for vulnerable populations who rely on these services for their well-being.
One of the most significant concerns is the reduction in access to care. Many communities that once had multiple healthcare options now find themselves with fewer choices, leading to increased barriers to accessing necessary services. A study by the Robert Wood Johnson Foundation found that communities with fewer healthcare providers experience higher rates of chronic diseases and poorer health outcomes.
Moreover, the psychological impact of losing a major healthcare provider cannot be overlooked. Communities often view hospitals as cornerstones of their health infrastructure, and their collapse can lead to feelings of insecurity and fear. A survey conducted by the Pew Research Center found that 70% of respondents in affected areas expressed concern about their ability to access healthcare services in the future.
- Reduced Access to Care: Increased barriers for vulnerable populations.
- Higher Rates of Chronic Diseases: Communities with fewer providers facing worse health outcomes.
- Psychological Impact: Feelings of insecurity and fear among community members.
- Community Trust Erosion: Loss of trust in the healthcare system.
- Increased Health Disparities: Widening gap in health equity among populations.
The erosion of community trust in the healthcare system is another critical issue. As residents grapple with the uncertainty surrounding their healthcare options, many have become disillusioned with the system as a whole. This loss of trust can lead to decreased engagement with healthcare services, further exacerbating health disparities in already vulnerable populations.
Policy Responses: Government and Institutional Actions
In the wake of Steward’s bankruptcy, various stakeholders have begun to respond to the crisis through policy initiatives and institutional actions. Governments at both the state and federal levels have recognized the need to address the fallout from this collapse and are exploring various strategies to stabilize the healthcare landscape.
One of the primary responses has been the introduction of financial assistance programs aimed at supporting struggling hospitals. For instance, several states have allocated emergency funds to help hospitals cover operational costs and maintain essential services. A report from the National Conference of State Legislatures indicated that over 15 states have implemented such programs in response to the crisis.
Additionally, policymakers are exploring regulatory changes to facilitate mergers and acquisitions among healthcare providers. By encouraging consolidation, governments hope to create more robust healthcare systems that can withstand financial pressures. However, this approach has raised concerns about potential monopolies and reduced competition, which could ultimately harm patients.
- Financial Assistance Programs: Emergency funds allocated to struggling hospitals.
- Regulatory Changes: Encouraging mergers and acquisitions among providers.
- Community Health Initiatives: Programs aimed at improving access to care.
- Telehealth Expansion: Increased support for telehealth services.
- Long-term Strategic Planning: Developing sustainable healthcare models.
Community health initiatives have also gained traction as a response to the crisis. Many organizations are working to improve access to care through outreach programs, mobile clinics, and telehealth services. These efforts aim to bridge the gap left by Steward’s collapse and ensure that vulnerable populations continue to receive the care they need.
Looking Ahead: The Future of Healthcare Post-Steward
As we reflect on the ongoing impact of Steward’s collapse, it is essential to consider the future of healthcare in the affected communities. The lessons learned from this crisis can inform strategies for building a more resilient healthcare system that can withstand future challenges.
One critical area of focus will be the need for diversification in healthcare delivery. Hospitals must explore innovative models that prioritize community engagement and address the unique needs of their populations. This may include expanding telehealth services, enhancing preventive care programs, and fostering partnerships with community organizations.
Additionally, there is a growing recognition of the importance of addressing social determinants of health. Factors such as housing, education, and access to nutritious food play a significant role in overall health outcomes. By adopting a holistic approach to healthcare that considers these determinants, providers can work towards improving health equity and reducing disparities.
- Diversification in Healthcare Delivery: Exploring innovative models for care.
- Community Engagement: Prioritizing the unique needs of populations.
- Expansion of Telehealth Services: Enhancing access to care through technology.
- Addressing Social Determinants of Health: Focusing on factors that impact health outcomes.
- Building Resilient Healthcare Systems: Preparing for future challenges.
Ultimately, the future of healthcare post-Steward will depend on the collective efforts of policymakers, healthcare providers, and communities. By learning from the past and embracing innovative solutions, there is an opportunity to create a more equitable and sustainable healthcare system that serves all individuals effectively.
Conclusion: Key Takeaways from Steward’s Collapse
The collapse of Steward Health Care System has left an indelible mark on hospitals and communities, with ongoing impacts that continue to unfold one year later. From financial fallout and operational challenges to social ramifications and policy responses, the consequences of this event are far-reaching.
As we look ahead, it is crucial to recognize the lessons learned from this crisis. The need for diversification in healthcare delivery, community engagement, and addressing social determinants of health are paramount for building a resilient healthcare system. By working collaboratively, stakeholders can ensure that the mistakes of the past do not define the future of healthcare.
In summary, the ongoing impact of Steward’s collapse serves as a reminder of the fragility of our healthcare systems and the importance of proactive measures to safeguard the health and well-being of our communities. Through innovation, collaboration, and a commitment to equity, we can pave the way for a brighter future in healthcare.