NHS England to be Overhauled with a Focus on Streamlined Technology
The National Health Service (NHS) in England has long been a cornerstone of public health, providing essential services to millions. However, as the demands on healthcare systems evolve, so too must the methods by which these services are delivered. The recent push towards overhauling NHS England with a focus on streamlined technology represents a significant shift in how healthcare can be managed, accessed, and delivered. This article explores the implications of this transformation, examining the integration of technology in healthcare, the challenges faced, and the potential benefits for patients and providers alike.
1. The Current State of NHS England
Before delving into the technological overhaul, it is essential to understand the current state of NHS England. The NHS has been under increasing pressure due to rising patient demand, an aging population, and budget constraints. According to NHS Digital, the number of patients waiting for treatment reached a record high of over 6 million in 2022, highlighting the urgent need for reform.
Moreover, the COVID-19 pandemic has exacerbated existing challenges, forcing the NHS to adapt rapidly to new circumstances. Telehealth services surged during the pandemic, with a reported 96% increase in remote consultations. This shift has prompted discussions about the long-term integration of technology into everyday healthcare practices.
- Increased Demand: The aging population and chronic health conditions have led to a surge in demand for healthcare services.
- Budget Constraints: Financial pressures have limited the NHS’s ability to expand services and invest in new technologies.
- COVID-19 Impact: The pandemic has accelerated the adoption of digital health solutions, revealing both opportunities and challenges.
As the NHS navigates these challenges, the integration of technology emerges as a viable solution to streamline operations and improve patient care.
2. The Role of Technology in Healthcare Transformation
Technology has the potential to revolutionize healthcare delivery, making it more efficient and patient-centered. The NHS’s commitment to embracing technology is evident in several key areas:
- Electronic Health Records (EHRs): EHRs allow for the seamless sharing of patient information across different healthcare providers, reducing duplication of tests and improving care coordination.
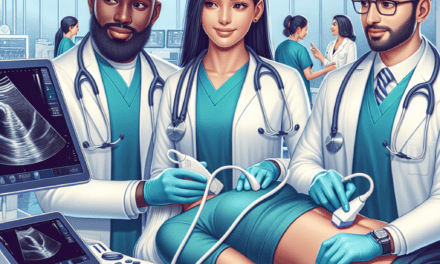
- Telemedicine: Remote consultations have become a staple in healthcare, providing patients with access to medical advice without the need for in-person visits.
- Artificial Intelligence (AI): AI can assist in diagnosing conditions, predicting patient outcomes, and personalizing treatment plans.
- Wearable Technology: Devices that monitor health metrics can empower patients to take control of their health and provide valuable data to healthcare providers.
- Data Analytics: Analyzing large datasets can help identify trends, improve resource allocation, and enhance patient outcomes.
For instance, the use of AI in radiology has shown promise in improving diagnostic accuracy. A study published in the journal “Nature” found that an AI system outperformed human radiologists in detecting breast cancer in mammograms. Such advancements can lead to earlier diagnoses and better treatment outcomes.
Moreover, the integration of telemedicine has proven beneficial for both patients and healthcare providers. A report from the NHS found that 85% of patients were satisfied with their telehealth experience, citing convenience and reduced travel time as significant advantages. This shift not only enhances patient satisfaction but also optimizes healthcare resources.
3. Challenges in Implementing Technology in NHS England
Despite the clear benefits of integrating technology into NHS England, several challenges must be addressed to ensure a successful overhaul:
- Data Privacy and Security: With the increased use of digital health records and telemedicine, safeguarding patient data becomes paramount. Cybersecurity threats pose significant risks to sensitive health information.
- Digital Divide: Not all patients have equal access to technology. Disparities in digital literacy and access to devices can hinder the effectiveness of telehealth services.
- Resistance to Change: Healthcare professionals may be hesitant to adopt new technologies due to concerns about training, workflow disruptions, or skepticism about their efficacy.
- Funding and Resources: Implementing new technologies requires significant investment. Budget constraints may limit the NHS’s ability to adopt and maintain advanced systems.
- Integration with Existing Systems: Ensuring that new technologies work seamlessly with existing healthcare infrastructure can be a complex and time-consuming process.
Addressing these challenges requires a comprehensive strategy that includes training for healthcare professionals, investment in cybersecurity measures, and initiatives to bridge the digital divide. For example, the NHS has launched programs aimed at improving digital literacy among patients, ensuring that everyone can benefit from technological advancements.
4. Case Studies of Successful Technology Integration
Several case studies illustrate the successful integration of technology within healthcare systems, providing valuable lessons for NHS England:
- Babylon Health: This UK-based digital health service offers AI-driven consultations via a mobile app. Patients can describe their symptoms, and the AI provides potential diagnoses and treatment options. Babylon has reported that 90% of users found the service helpful, demonstrating the potential for AI in primary care.
- HealthTap: An American telehealth platform that connects patients with doctors for virtual consultations. HealthTap has successfully reduced wait times and improved access to care, particularly for underserved populations.
- Epic Systems: A leading EHR provider that has transformed how hospitals manage patient data. Epic’s system allows for real-time data sharing among providers, improving care coordination and patient outcomes.
- Remote Patient Monitoring (RPM): Programs like Philips’ RPM have shown success in managing chronic conditions such as diabetes and heart disease. By using connected devices to monitor patients’ health metrics, healthcare providers can intervene early and reduce hospital admissions.
- MyChart: A patient portal that allows individuals to access their health records, schedule appointments, and communicate with healthcare providers. MyChart has improved patient engagement and satisfaction by empowering individuals to take an active role in their healthcare.
These case studies highlight the diverse applications of technology in healthcare and underscore the importance of learning from successful implementations. By adopting best practices from these examples, NHS England can enhance its approach to integrating technology into its services.
5. The Future of NHS England: A Vision for Technology-Driven Healthcare
The future of NHS England hinges on its ability to embrace technology as a fundamental component of healthcare delivery. Several key trends are likely to shape this future:
- Personalized Medicine: Advances in genomics and data analytics will enable healthcare providers to tailor treatments to individual patients, improving outcomes and reducing adverse effects.
- Interoperability: Ensuring that different healthcare systems can communicate effectively will be crucial for seamless patient care. Efforts to standardize data formats and protocols will facilitate this integration.
- Patient Empowerment: As patients gain access to their health data and digital tools, they will become more engaged in their care, leading to better health outcomes.
- AI and Machine Learning: The continued development of AI technologies will enhance diagnostic capabilities, streamline administrative tasks, and improve patient management.
- Telehealth Expansion: The trend towards remote consultations is likely to continue, with telehealth becoming a standard option for many healthcare services.
To realize this vision, NHS England must prioritize investment in technology, foster a culture of innovation, and engage stakeholders at all levels. Collaboration with technology companies, healthcare professionals, and patients will be essential to create a healthcare system that is not only efficient but also equitable and accessible.
Conclusion
The overhaul of NHS England with a focus on streamlined technology represents a pivotal moment in the evolution of healthcare delivery. By embracing digital solutions, the NHS can address pressing challenges, improve patient outcomes, and enhance the overall efficiency of the healthcare system. However, this transformation will require careful planning, investment, and collaboration among all stakeholders.
As we look to the future, it is clear that technology will play an increasingly vital role in shaping the landscape of healthcare. By learning from successful case studies, addressing challenges head-on, and fostering a culture of innovation, NHS England can pave the way for a more effective, patient-centered healthcare system that meets the needs of all citizens.
In summary, the integration of technology into NHS England is not merely a trend but a necessary evolution that promises to enhance the quality of care, improve access to services, and ultimately save lives. The journey ahead may be complex, but the potential rewards are immense, making it a worthy endeavor for the future of public health in England.