Iowa Enacts Stricter Regulations on Pharmacy Benefit Managers
In recent years, the role of Pharmacy Benefit Managers (PBMs) has come under increasing scrutiny across the United States. These intermediaries between insurers, pharmacies, and drug manufacturers have been criticized for their lack of transparency and the impact they have on drug pricing. In response to growing concerns, Iowa has taken significant steps to regulate PBMs more strictly. This article explores the implications of these regulations, the motivations behind them, and their potential impact on the healthcare landscape in Iowa and beyond.
Understanding Pharmacy Benefit Managers
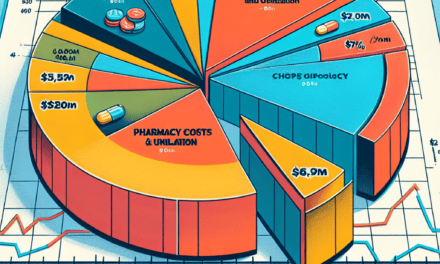
Pharmacy Benefit Managers are entities that manage prescription drug benefits on behalf of health insurers, Medicare Part D drug plans, and large employers. Their primary functions include negotiating discounts with drug manufacturers, managing formularies (lists of covered drugs), and processing prescription claims. While PBMs claim to reduce costs and improve access to medications, their practices have raised questions about transparency and fairness.
The Role of PBMs in the Healthcare System
PBMs play a crucial role in the healthcare system, acting as intermediaries that influence the cost and accessibility of medications. Their responsibilities include:
- Negotiating Discounts: PBMs negotiate prices with drug manufacturers, aiming to secure lower costs for insurers and patients.
- Formulary Management: They create and maintain formularies, determining which drugs are covered and at what tier, which can significantly affect patient access to medications.
- Claims Processing: PBMs handle the processing of prescription claims, ensuring that pharmacies are reimbursed for the medications dispensed.
- Utilization Management: They implement programs to manage the use of medications, such as prior authorization and step therapy, to control costs.
Despite these functions, the lack of transparency in PBM operations has led to concerns about their impact on drug prices and patient access. Critics argue that PBMs often prioritize profits over patient care, leading to higher out-of-pocket costs for consumers.
The Controversy Surrounding PBMs
The controversy surrounding PBMs stems from several key issues:
- Lack of Transparency: Many PBMs do not disclose the rebates they negotiate with drug manufacturers, leading to questions about whether these savings are passed on to consumers.
- High Out-of-Pocket Costs: Patients often face high copays for medications, even when PBMs negotiate lower prices, raising concerns about affordability.
- Impact on Pharmacies: Independent pharmacies often struggle to compete with larger chains due to the reimbursement rates set by PBMs, which can lead to closures and reduced access to care.
These issues have prompted states like Iowa to take action, seeking to regulate PBMs more effectively to protect consumers and ensure fair practices.
The Legislative Landscape in Iowa
Iowa’s decision to enact stricter regulations on PBMs is part of a broader trend among states seeking to address the challenges posed by these entities. The Iowa legislature has introduced several bills aimed at increasing transparency and accountability in PBM operations.
Key Legislative Changes
In 2023, Iowa passed a series of laws aimed at regulating PBMs more stringently. Some of the key provisions include:
- Transparency Requirements: PBMs are now required to disclose the rebates they receive from drug manufacturers and how these savings are passed on to consumers.
- Fair Reimbursement Practices: The legislation mandates that PBMs provide fair reimbursement rates to pharmacies, particularly independent ones, to ensure they can compete effectively.
- Patient Protections: New rules have been established to protect patients from excessive out-of-pocket costs, including limits on copays for certain medications.
- Licensing and Oversight: PBMs must now be licensed in Iowa, subjecting them to state oversight and accountability measures.
These legislative changes reflect a growing recognition of the need for greater oversight of PBMs and a commitment to protecting consumers from potential abuses.
The Motivations Behind Stricter Regulations
The motivations for enacting stricter regulations on PBMs in Iowa are multifaceted. Key factors include:
- Consumer Advocacy: Advocacy groups have long pushed for reforms to protect consumers from high drug prices and lack of transparency in PBM practices.
- Rising Drug Costs: The increasing cost of prescription medications has become a significant concern for many Iowans, prompting lawmakers to take action.
- Impact on Local Pharmacies: The struggles faced by independent pharmacies in Iowa have highlighted the need for fair reimbursement practices and support for local businesses.
These motivations have converged to create a legislative environment conducive to reform, with lawmakers responding to the concerns of their constituents.
Impact on Patients and Healthcare Providers
The new regulations on PBMs in Iowa are expected to have significant implications for both patients and healthcare providers. Understanding these impacts is crucial for stakeholders across the healthcare spectrum.
Benefits for Patients
One of the primary goals of the new regulations is to improve patient access to affordable medications. Some anticipated benefits for patients include:
- Lower Out-of-Pocket Costs: By requiring PBMs to disclose rebates and pass savings on to consumers, patients may see a reduction in their copays for prescription medications.
- Increased Access to Medications: Fair reimbursement practices for pharmacies may lead to improved access to medications, particularly in rural areas where independent pharmacies play a vital role.
- Enhanced Transparency: Patients will have greater visibility into the costs associated with their medications, allowing them to make more informed choices about their healthcare.
These benefits could lead to improved health outcomes for patients, as access to necessary medications becomes more equitable and affordable.
Challenges for Healthcare Providers
While the regulations aim to protect patients, they may also present challenges for healthcare providers, particularly pharmacies. Some potential challenges include:
- Compliance Costs: Pharmacies may face increased administrative burdens and costs associated with complying with new regulations, which could impact their bottom line.
- Market Adjustments: As PBMs adjust their practices in response to regulations, pharmacies may need to adapt their business models to remain competitive.
- Potential Pushback from PBMs: PBMs may resist changes and seek to influence legislation or regulations in ways that could undermine the intended benefits for patients and providers.
Healthcare providers will need to navigate these challenges while continuing to prioritize patient care and access to medications.
Case Studies: Other States Taking Action
Iowa is not alone in its efforts to regulate PBMs. Several other states have enacted similar measures, providing valuable case studies for understanding the potential impact of such regulations.
Case Study: Ohio
Ohio has been at the forefront of PBM regulation, implementing a series of reforms aimed at increasing transparency and accountability. Key measures include:
- Rebate Disclosure: Ohio requires PBMs to disclose the rebates they negotiate with drug manufacturers, ensuring that consumers benefit from lower prices.
- Pharmacy Reimbursement Rates: The state has established minimum reimbursement rates for pharmacies, helping to support independent providers.
- Patient Protections: Ohio has implemented measures to protect patients from excessive out-of-pocket costs, similar to those enacted in Iowa.
The results of these reforms have been promising, with reports indicating that patients are experiencing lower drug costs and improved access to medications.
Case Study: Arkansas
Arkansas has also taken significant steps to regulate PBMs, focusing on transparency and fair practices. Key initiatives include:
- Licensing Requirements: Arkansas requires PBMs to be licensed, subjecting them to state oversight and accountability measures.
- Reimbursement Transparency: The state mandates that PBMs disclose their reimbursement rates to pharmacies, promoting fair competition.
- Consumer Protections: Arkansas has implemented consumer protection measures to ensure that patients are not unfairly burdened by high drug costs.
These initiatives have led to positive outcomes for patients and pharmacies, demonstrating the potential benefits of regulatory action.
The Future of PBM Regulation in Iowa
The enactment of stricter regulations on PBMs in Iowa marks a significant step toward addressing the challenges posed by these entities. However, the future of PBM regulation remains uncertain, as stakeholders continue to navigate the complexities of the healthcare landscape.
Potential Challenges Ahead
As Iowa moves forward with its new regulations, several challenges may arise:
- Resistance from PBMs: PBMs may push back against regulations, seeking to influence legislation or undermine enforcement efforts.
- Implementation Issues: Ensuring that new regulations are effectively implemented and enforced will require ongoing oversight and resources.
- Market Dynamics: Changes in the PBM landscape may lead to shifts in market dynamics, impacting pharmacies and patients in unforeseen ways.
Addressing these challenges will be crucial for ensuring that the intended benefits of regulation are realized.
Looking Ahead: Opportunities for Improvement
Despite the challenges, there are also opportunities for improvement in Iowa’s healthcare system:
- Collaboration with Stakeholders: Engaging with healthcare providers, patients, and advocacy groups can help ensure that regulations are effective and responsive to community needs.
- Data-Driven Decision Making: Utilizing data to assess the impact of regulations on drug pricing and access can inform future policy decisions.
- Continued Advocacy: Ongoing advocacy efforts can help maintain momentum for reform and ensure that patient interests remain a priority.
By capitalizing on these opportunities, Iowa can continue to lead the way in PBM regulation and improve the healthcare landscape for its residents.
Conclusion
The enactment of stricter regulations on Pharmacy Benefit Managers in Iowa represents a significant step toward addressing the challenges posed by these entities. By increasing transparency, ensuring fair reimbursement practices, and protecting patients from excessive costs, Iowa aims to create a more equitable healthcare system. While challenges remain, the potential benefits for patients and healthcare providers are substantial. As other states look to Iowa as a model for reform, the ongoing dialogue around PBM regulation will be crucial in shaping the future of healthcare in the United States.
In summary, the actions taken by Iowa reflect a growing recognition of the need for accountability in the healthcare system. By prioritizing patient access and affordability, Iowa is setting a precedent that could inspire similar reforms across the nation, ultimately leading to a more transparent and equitable healthcare landscape.