Integrating Physical and Mental Healthcare: The Role of the ACO Primary Care Flex Model
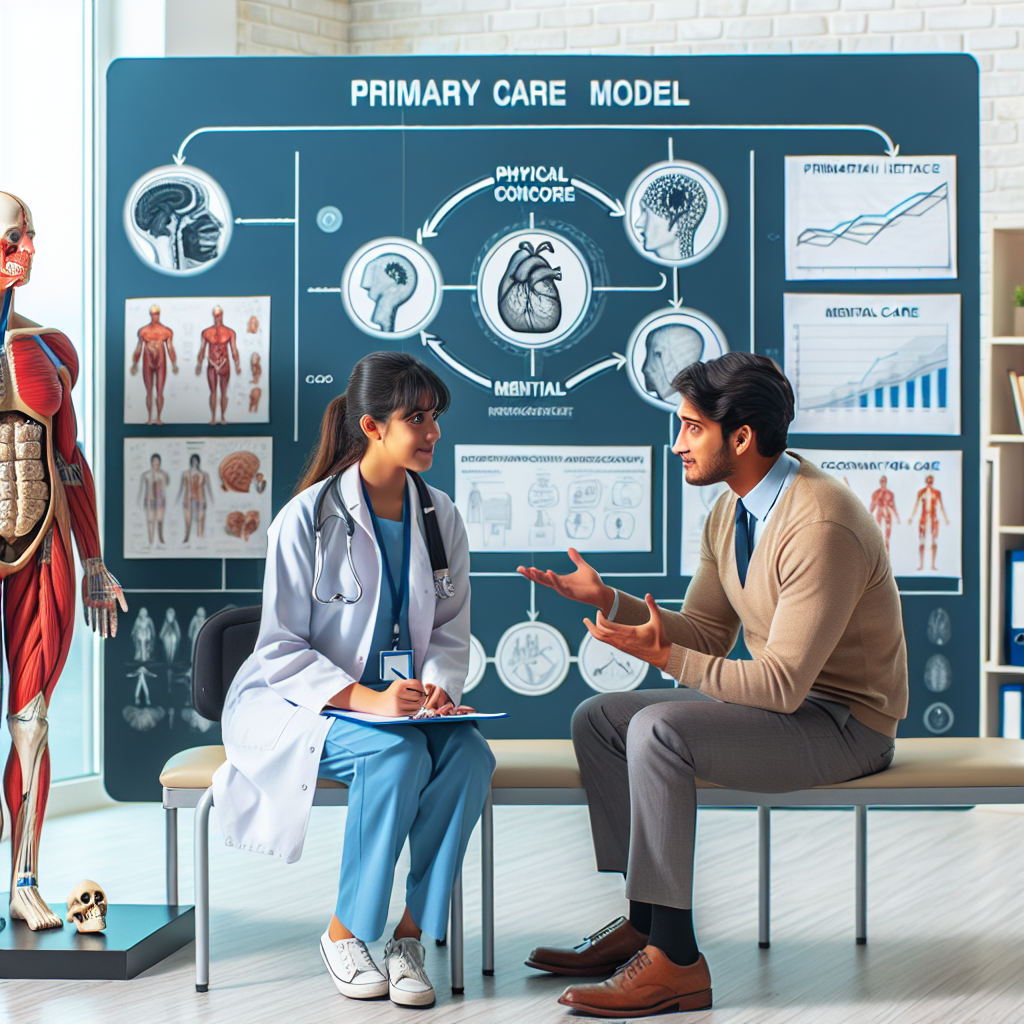
The integration of physical and mental healthcare has become a critical focus in modern medicine, driven by the recognition that mental health significantly impacts physical health and vice versa. Accountable Care Organizations (ACOs) have emerged as a promising model to facilitate this integration, particularly through the Primary Care Flex Model. This article explores the role of the ACO Primary Care Flex Model in integrating physical and mental healthcare, examining its structure, benefits, challenges, and real-world applications.
Understanding the ACO Primary Care Flex Model
The ACO Primary Care Flex Model is a healthcare delivery approach designed to improve patient outcomes by fostering collaboration among healthcare providers. This model emphasizes flexibility in care delivery, allowing primary care providers to tailor services to meet the unique needs of their patients. By integrating physical and mental healthcare, the model aims to provide comprehensive care that addresses all aspects of a patient’s health.
Structure of the ACO Primary Care Flex Model
The ACO Primary Care Flex Model is structured around a network of healthcare providers who work collaboratively to deliver coordinated care. This network typically includes primary care physicians, specialists, mental health professionals, and other healthcare providers. The model is designed to be patient-centered, with a focus on delivering personalized care that meets the individual needs of each patient.
Key components of the model include:
- Integrated Care Teams: Multidisciplinary teams that include primary care providers, mental health professionals, and other specialists work together to develop and implement comprehensive care plans.
- Care Coordination: A focus on coordinating care across different providers and settings to ensure seamless transitions and continuity of care.
- Patient Engagement: Encouraging patients to take an active role in their healthcare by involving them in decision-making and care planning.
- Data Sharing: Utilizing electronic health records and other technologies to facilitate communication and information sharing among providers.
- Performance Measurement: Monitoring and evaluating the quality and outcomes of care to identify areas for improvement.
Benefits of Integrating Physical and Mental Healthcare
Integrating physical and mental healthcare offers numerous benefits for patients, providers, and the healthcare system as a whole. By addressing both physical and mental health needs, the ACO Primary Care Flex Model can improve patient outcomes, enhance patient satisfaction, and reduce healthcare costs.
Some of the key benefits include:
- Improved Health Outcomes: By addressing mental health issues alongside physical health conditions, patients are more likely to experience better overall health outcomes.
- Enhanced Patient Experience: Patients receive more comprehensive and coordinated care, leading to higher levels of satisfaction and engagement.
- Reduced Healthcare Costs: By preventing complications and reducing the need for emergency care, integrated care can lead to significant cost savings for the healthcare system.
- Increased Provider Collaboration: Providers work together more effectively, leading to improved communication and coordination of care.
- Better Management of Chronic Conditions: Integrated care can help patients better manage chronic conditions by addressing both physical and mental health needs.
Challenges in Implementing the ACO Primary Care Flex Model
While the ACO Primary Care Flex Model offers many benefits, there are also significant challenges to its implementation. These challenges can hinder the integration of physical and mental healthcare and limit the model’s effectiveness.
Some of the key challenges include:
- Fragmented Healthcare System: The existing healthcare system is often fragmented, with separate providers and systems for physical and mental health care. This fragmentation can make it difficult to coordinate care and share information.
- Reimbursement and Funding Issues: Traditional reimbursement models may not adequately support integrated care, leading to financial challenges for providers.
- Workforce Shortages: There is a shortage of mental health professionals, which can limit access to care and hinder integration efforts.
- Stigma and Cultural Barriers: Stigma surrounding mental health can prevent patients from seeking care and hinder integration efforts.
- Data Privacy Concerns: Sharing patient information across providers raises concerns about data privacy and security.
Case Studies: Successful Integration of Physical and Mental Healthcare
Several healthcare organizations have successfully implemented the ACO Primary Care Flex Model to integrate physical and mental healthcare. These case studies provide valuable insights into the model’s effectiveness and the strategies used to overcome challenges.
One example is the Montefiore Medical Center in New York, which has implemented an integrated care model that includes primary care, mental health, and social services. By using a team-based approach and focusing on care coordination, Montefiore has improved patient outcomes and reduced healthcare costs.
Another example is the Cherokee Health Systems in Tennessee, which has integrated behavioral health services into its primary care clinics. By co-locating mental health professionals with primary care providers, Cherokee Health Systems has improved access to care and enhanced patient satisfaction.
Future Directions for the ACO Primary Care Flex Model
The future of the ACO Primary Care Flex Model is promising, with opportunities for further integration and innovation. As healthcare systems continue to evolve, the model can be adapted to meet the changing needs of patients and providers.
Some potential future directions include:
- Expanding Telehealth Services: Telehealth can enhance access to care and facilitate integration by allowing providers to collaborate remotely.
- Leveraging Technology: Advanced technologies, such as artificial intelligence and machine learning, can support data analysis and care coordination.
- Focusing on Population Health: The model can be used to address social determinants of health and improve outcomes for entire populations.
- Enhancing Patient Engagement: Innovative approaches to patient engagement, such as digital health tools and personalized care plans, can empower patients to take an active role in their healthcare.
- Strengthening Partnerships: Collaborations between healthcare organizations, community agencies, and policymakers can support integration efforts and address systemic challenges.
Conclusion
The integration of physical and mental healthcare through the ACO Primary Care Flex Model represents a significant advancement in healthcare delivery. By fostering collaboration among providers and focusing on patient-centered care, the model has the potential to improve health outcomes, enhance patient satisfaction, and reduce healthcare costs. While challenges remain, successful case studies demonstrate the model’s effectiveness and provide valuable insights for future implementation. As healthcare systems continue to evolve, the ACO Primary Care Flex Model offers a promising framework for delivering comprehensive, integrated care that addresses the full spectrum of patient needs.