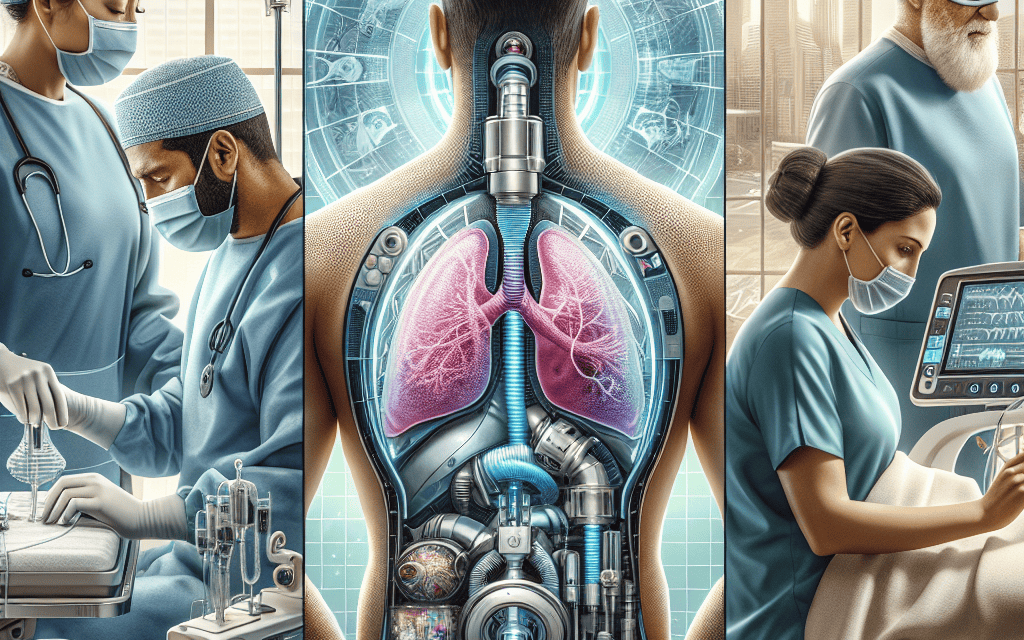
Innovations in MedTech Enhancing Tracheostomy Procedures and Recovery
Tracheostomy, a surgical procedure that involves creating an opening in the neck to place a tube into the windpipe, has been a critical intervention for patients with respiratory distress or obstruction. Over the years, advancements in medical technology (MedTech) have significantly improved the safety, efficiency, and recovery outcomes associated with tracheostomy procedures. This article explores the latest innovations in MedTech that are enhancing tracheostomy procedures and recovery, focusing on five key areas: surgical techniques, device innovations, patient monitoring technologies, rehabilitation advancements, and telemedicine integration.
Surgical Techniques: Minimally Invasive Approaches
Traditionally, tracheostomy procedures were performed using open surgical techniques, which often resulted in longer recovery times and increased risk of complications. However, recent innovations in surgical techniques have led to the development of minimally invasive approaches that offer numerous benefits.
Minimally invasive tracheostomy (MIT) techniques utilize smaller incisions and specialized instruments, allowing for reduced trauma to surrounding tissues. These techniques can be performed using endoscopic guidance, which enhances precision and minimizes complications. For instance, the use of video-assisted thoracoscopic surgery (VATS) has gained popularity in recent years. VATS allows surgeons to visualize the trachea and surrounding structures through small incisions, leading to less postoperative pain and quicker recovery times.
Another significant advancement is the use of percutaneous dilatational tracheostomy (PDT). This technique involves the insertion of a dilator through the skin and into the trachea, allowing for the placement of a tracheostomy tube without the need for extensive dissection. Studies have shown that PDT is associated with lower rates of complications, such as bleeding and infection, compared to traditional open techniques.
- Benefits of Minimally Invasive Techniques:
- Reduced postoperative pain
- Shorter hospital stays
- Lower risk of complications
- Faster recovery times
- Case Study: A study published in the Journal of Thoracic Disease found that patients undergoing PDT had a 30% shorter recovery time compared to those who underwent traditional tracheostomy.
As these minimally invasive techniques continue to evolve, they are expected to become the standard of care for tracheostomy procedures, further enhancing patient outcomes and satisfaction.
Device Innovations: Smart Tracheostomy Tubes
The development of smart tracheostomy tubes represents a significant leap forward in MedTech innovation. These advanced devices are equipped with sensors and monitoring capabilities that provide real-time data on patient status, enhancing safety and facilitating timely interventions.
Smart tracheostomy tubes can monitor various parameters, including airflow, humidity, and temperature. For example, the use of integrated sensors can alert healthcare providers to changes in airflow that may indicate tube obstruction or displacement. This proactive monitoring can prevent complications and reduce the need for emergency interventions.
Additionally, some smart tracheostomy tubes are designed with built-in suction capabilities, allowing for automated clearance of secretions. This feature is particularly beneficial for patients with high secretion levels, as it reduces the risk of aspiration and improves overall respiratory function.
- Key Features of Smart Tracheostomy Tubes:
- Real-time monitoring of airflow and respiratory parameters
- Automated suction capabilities
- Alerts for potential complications
- Data integration with electronic health records (EHRs)
- Case Study: A clinical trial demonstrated that patients using smart tracheostomy tubes experienced a 40% reduction in respiratory complications compared to those with traditional tubes.
As these devices become more widely adopted, they are expected to revolutionize the management of tracheostomy patients, leading to improved outcomes and enhanced quality of life.
Patient Monitoring Technologies: Remote Monitoring and AI Integration
Advancements in patient monitoring technologies have transformed the way healthcare providers manage tracheostomy patients. Remote monitoring systems, powered by artificial intelligence (AI), enable continuous assessment of patient health, allowing for timely interventions and reducing hospital readmissions.
Remote monitoring systems can track vital signs, respiratory patterns, and other health metrics from the comfort of the patient’s home. This technology is particularly beneficial for patients who have recently undergone tracheostomy, as it allows healthcare providers to monitor their recovery without requiring frequent in-person visits.
AI algorithms can analyze data collected from remote monitoring devices to identify trends and predict potential complications. For instance, if a patient’s respiratory rate deviates from the norm, the system can alert healthcare providers to intervene before the situation escalates. This proactive approach not only enhances patient safety but also reduces the burden on healthcare facilities.
- Benefits of Remote Monitoring:
- Continuous assessment of patient health
- Early detection of complications
- Reduced need for hospital visits
- Improved patient engagement and self-management
- Case Study: A study published in the Journal of Medical Internet Research found that patients using remote monitoring systems had a 50% lower rate of hospital readmissions within 30 days post-tracheostomy.
As remote monitoring technologies continue to advance, they are expected to play a crucial role in enhancing the recovery process for tracheostomy patients, ultimately leading to better health outcomes and improved quality of life.
Rehabilitation Advancements: Speech Therapy and Swallowing Rehabilitation
Rehabilitation is a critical component of the recovery process for tracheostomy patients. Innovations in rehabilitation techniques, particularly in speech therapy and swallowing rehabilitation, have significantly improved patient outcomes and quality of life.
Speech therapy for tracheostomy patients has evolved to incorporate advanced techniques and technologies. For instance, the use of electrolarynx devices allows patients who have undergone tracheostomy to produce speech by generating sound vibrations that can be articulated using the mouth. This technology has empowered many patients to regain their ability to communicate effectively.
Additionally, swallowing rehabilitation has become a focal point in the recovery process. Patients with tracheostomies often experience difficulties with swallowing due to changes in airway dynamics. Innovative therapies, such as neuromuscular electrical stimulation (NMES), have shown promise in improving swallowing function. NMES involves applying electrical impulses to the muscles involved in swallowing, enhancing muscle strength and coordination.
- Key Rehabilitation Techniques:
- Electrolarynx devices for speech production
- Neuromuscular electrical stimulation for swallowing rehabilitation
- Individualized therapy plans tailored to patient needs
- Use of teletherapy for remote access to rehabilitation services
- Case Study: A study published in the Archives of Physical Medicine and Rehabilitation found that patients who participated in structured speech and swallowing rehabilitation programs experienced a 60% improvement in communication abilities and swallowing function.
As rehabilitation techniques continue to advance, they are expected to play a vital role in enhancing the overall recovery experience for tracheostomy patients, enabling them to regain their independence and improve their quality of life.
Telemedicine Integration: Enhancing Access to Care
The integration of telemedicine into tracheostomy care has emerged as a game-changer, particularly in the wake of the COVID-19 pandemic. Telemedicine allows healthcare providers to deliver care remotely, improving access to specialized services for tracheostomy patients.
Through telemedicine platforms, patients can consult with healthcare providers, receive follow-up care, and participate in rehabilitation sessions without the need for in-person visits. This is especially beneficial for patients living in rural or underserved areas, where access to specialized tracheostomy care may be limited.
Telemedicine also facilitates better communication between patients and healthcare providers. Patients can easily report symptoms, ask questions, and receive guidance on managing their tracheostomy care. This enhanced communication fosters a collaborative approach to care, empowering patients to take an active role in their recovery.
- Benefits of Telemedicine Integration:
- Improved access to specialized care
- Convenient follow-up consultations
- Enhanced patient-provider communication
- Reduced travel burden for patients
- Case Study: A study published in the Journal of Telemedicine and Telecare found that telemedicine consultations for tracheostomy patients resulted in a 70% satisfaction rate among patients and caregivers.
As telemedicine continues to evolve, it is expected to play an increasingly important role in enhancing the care and recovery of tracheostomy patients, ultimately leading to improved health outcomes and patient satisfaction.
Conclusion
The landscape of tracheostomy care is rapidly evolving, driven by innovations in MedTech that enhance surgical techniques, device capabilities, patient monitoring, rehabilitation, and telemedicine integration. These advancements are not only improving the safety and efficiency of tracheostomy procedures but also significantly enhancing the recovery experience for patients.
Minimally invasive surgical techniques are reducing trauma and recovery times, while smart tracheostomy tubes are providing real-time monitoring and proactive interventions. Remote monitoring technologies are enabling continuous assessment of patient health, and advancements in rehabilitation are empowering patients to regain their communication and swallowing abilities. Finally, telemedicine is enhancing access to care, ensuring that patients receive the support they need throughout their recovery journey.
As these innovations continue to develop and become integrated into standard practice, they hold the promise of transforming tracheostomy care, ultimately leading to better health outcomes and improved quality of life for patients. The future of tracheostomy procedures is bright, and ongoing research and development will undoubtedly yield even more exciting advancements in the years to come.