Humana’s Measured Support for Medicare Advantage
As the healthcare landscape continues to evolve, Medicare Advantage (MA) plans have gained significant traction among seniors seeking comprehensive healthcare coverage. Humana, one of the largest health insurance providers in the United States, has positioned itself as a leader in this sector. This article delves into Humana’s measured support for Medicare Advantage, exploring its offerings, strategies, and the impact on beneficiaries. We will cover five key subtopics: the evolution of Medicare Advantage, Humana’s plan offerings, member engagement strategies, the role of technology in enhancing care, and the future of Medicare Advantage under Humana’s leadership.
The Evolution of Medicare Advantage
Medicare Advantage plans, also known as Medicare Part C, were introduced in the 1990s as a way to provide beneficiaries with an alternative to traditional Medicare. These plans are offered by private insurance companies and must provide at least the same level of coverage as Original Medicare (Parts A and B), but they often include additional benefits such as vision, dental, and wellness programs.
Over the years, Medicare Advantage has evolved significantly, driven by changes in legislation, market demands, and the need for cost-effective healthcare solutions. The Balanced Budget Act of 1997 marked a pivotal moment, allowing for the expansion of MA plans. This legislation aimed to reduce Medicare spending while improving the quality of care. As a result, enrollment in Medicare Advantage plans has surged, with over 26 million beneficiaries enrolled as of 2023, representing nearly 45% of all Medicare beneficiaries.
Several factors have contributed to the growth of Medicare Advantage:
- Cost-Effectiveness: MA plans often provide lower out-of-pocket costs compared to traditional Medicare, making them attractive to seniors.
- Comprehensive Coverage: Many MA plans offer additional benefits that are not covered by Original Medicare, such as prescription drug coverage, preventive services, and wellness programs.
- Personalized Care: MA plans often emphasize care coordination and personalized health management, which can lead to better health outcomes.
Humana has been at the forefront of this evolution, adapting its offerings to meet the changing needs of beneficiaries. The company has consistently focused on enhancing the member experience, ensuring that its plans are not only comprehensive but also accessible and user-friendly.
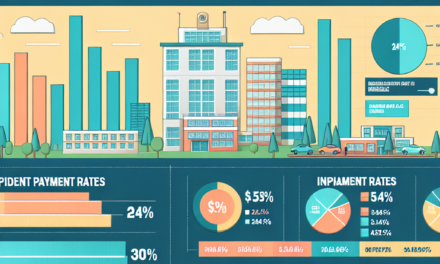
Humana’s Plan Offerings
Humana offers a diverse range of Medicare Advantage plans designed to cater to the varying needs of its members. These plans include Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), and Special Needs Plans (SNPs), each with unique features and benefits.
1. **Health Maintenance Organizations (HMOs):** Humana’s HMO plans require members to choose a primary care physician (PCP) and obtain referrals for specialist care. These plans typically offer lower premiums and out-of-pocket costs, making them an attractive option for cost-conscious seniors. Members benefit from a network of providers, ensuring coordinated care.
2. **Preferred Provider Organizations (PPOs):** Humana’s PPO plans provide more flexibility in choosing healthcare providers. Members can see any doctor or specialist without a referral, although they will pay less if they use in-network providers. This flexibility appeals to seniors who may have established relationships with specific healthcare providers.
3. **Special Needs Plans (SNPs):** Humana offers SNPs tailored for individuals with specific health conditions, such as chronic illnesses or those who are dually eligible for Medicare and Medicaid. These plans provide specialized care management and support services, ensuring that members receive the necessary resources to manage their health effectively.
4. **Additional Benefits:** Humana’s Medicare Advantage plans often include additional benefits that enhance the overall member experience. These may include:
- Prescription drug coverage
- Vision and dental care
- Fitness programs and gym memberships
- Transportation services for medical appointments
- Wellness programs focusing on preventive care
5. **Customization Options:** Humana recognizes that each member has unique healthcare needs. Therefore, the company offers customizable plan options that allow beneficiaries to select the benefits that matter most to them. This level of personalization is a key differentiator in the competitive Medicare Advantage market.
Humana’s commitment to providing a wide array of plan offerings ensures that seniors can find a plan that aligns with their healthcare needs and financial situation. This adaptability has contributed to Humana’s strong position in the Medicare Advantage market.
Member Engagement Strategies
Effective member engagement is crucial for the success of Medicare Advantage plans. Humana has implemented various strategies to enhance member engagement, ensuring that beneficiaries are informed, empowered, and satisfied with their healthcare experience.
1. **Personalized Communication:** Humana employs personalized communication strategies to keep members informed about their benefits, coverage options, and available resources. This includes targeted emails, newsletters, and phone calls tailored to individual member needs. By providing relevant information, Humana helps members make informed decisions about their healthcare.
2. **Health Education Programs:** Humana offers a range of health education programs designed to empower members to take control of their health. These programs cover topics such as chronic disease management, nutrition, and preventive care. By equipping members with knowledge, Humana fosters a proactive approach to health management.
3. **Care Coordination:** Humana emphasizes care coordination to ensure that members receive seamless healthcare services. This involves working closely with primary care physicians, specialists, and other healthcare providers to create a comprehensive care plan. Care coordinators are available to assist members in navigating the healthcare system, scheduling appointments, and accessing necessary services.
4. **Telehealth Services:** The COVID-19 pandemic accelerated the adoption of telehealth services, and Humana has embraced this trend. Members can access virtual consultations with healthcare providers, making it easier to receive care from the comfort of their homes. This convenience is particularly beneficial for seniors with mobility challenges or those living in rural areas.
5. **Feedback Mechanisms:** Humana actively seeks feedback from its members to improve its services continually. Surveys, focus groups, and member forums provide valuable insights into member experiences and preferences. By listening to its members, Humana can make data-driven decisions to enhance its offerings and address any concerns.
Through these member engagement strategies, Humana fosters a sense of community and support among its beneficiaries. This approach not only improves member satisfaction but also leads to better health outcomes, as engaged members are more likely to adhere to treatment plans and preventive measures.
The Role of Technology in Enhancing Care
Technology plays a pivotal role in transforming healthcare delivery, and Humana has embraced innovative solutions to enhance the care experience for its Medicare Advantage members. By leveraging technology, Humana aims to improve access to care, streamline processes, and empower members to take charge of their health.
1. **Digital Health Platforms:** Humana has developed digital health platforms that allow members to access their health information, schedule appointments, and communicate with healthcare providers. These platforms provide a centralized hub for managing health-related tasks, making it easier for members to stay organized and informed.
2. **Mobile Applications:** Humana’s mobile app offers a user-friendly interface for members to access their benefits, find in-network providers, and track their health goals. The app also includes features such as medication reminders and wellness challenges, encouraging members to engage in healthy behaviors.
3. **Data Analytics:** Humana utilizes data analytics to identify trends and patterns in member health. By analyzing claims data and health outcomes, the company can tailor its programs and interventions to address specific health needs. This data-driven approach enables Humana to proactively manage chronic conditions and improve overall member health.
4. **Remote Monitoring:** Humana has implemented remote monitoring solutions that allow healthcare providers to track members’ health metrics from home. This technology is particularly beneficial for individuals with chronic conditions, as it enables timely interventions and reduces the need for hospitalizations.
5. **Artificial Intelligence (AI):** Humana is exploring the use of AI to enhance care delivery. AI algorithms can analyze vast amounts of data to identify high-risk members and predict potential health issues. This proactive approach allows Humana to intervene early and provide targeted support to those who need it most.
By integrating technology into its Medicare Advantage offerings, Humana is not only improving the member experience but also driving better health outcomes. The company’s commitment to innovation positions it as a leader in the evolving healthcare landscape.
The Future of Medicare Advantage Under Humana’s Leadership
The future of Medicare Advantage is bright, with continued growth expected in enrollment and plan offerings. Humana’s leadership in this space is characterized by a commitment to innovation, member-centric care, and strategic partnerships.
1. **Expansion of Plan Offerings:** As the demand for Medicare Advantage plans continues to rise, Humana is likely to expand its offerings to meet the diverse needs of beneficiaries. This may include the introduction of new plan types, enhanced benefits, and tailored solutions for specific populations.
2. **Focus on Value-Based Care:** The shift towards value-based care is reshaping the healthcare landscape, and Humana is at the forefront of this movement. By emphasizing quality over quantity, Humana aims to improve health outcomes while controlling costs. This approach aligns with the goals of Medicare Advantage, which seeks to provide comprehensive care while managing expenditures.
3. **Partnerships and Collaborations:** Humana is likely to continue forming strategic partnerships with healthcare providers, technology companies, and community organizations. These collaborations can enhance care delivery, expand access to services, and improve health outcomes for members.
4. **Advocacy for Policy Changes:** As a leader in the Medicare Advantage space, Humana has a vested interest in advocating for policies that support the growth and sustainability of these plans. This includes engaging with lawmakers and stakeholders to promote initiatives that benefit seniors and improve the overall healthcare system.
5. **Commitment to Health Equity:** Humana recognizes the importance of addressing health disparities among its members. The company is likely to continue its efforts to promote health equity by implementing programs that target underserved populations and address social determinants of health.
In conclusion, Humana’s measured support for Medicare Advantage reflects its commitment to providing high-quality, accessible healthcare for seniors. Through a diverse range of plan offerings, innovative member engagement strategies, and a focus on technology, Humana is well-positioned to lead the way in the evolving Medicare Advantage landscape. As the company continues to adapt to the changing needs of beneficiaries, it remains dedicated to improving health outcomes and enhancing the overall member experience.
Conclusion
Humana’s approach to Medicare Advantage exemplifies a commitment to innovation, member engagement, and comprehensive care. The evolution of Medicare Advantage has created opportunities for insurers like Humana to provide tailored solutions that meet the diverse needs of seniors. With a focus on personalized communication, technology integration, and strategic partnerships, Humana is not only enhancing the member experience but also driving better health outcomes.
As the Medicare Advantage landscape continues to evolve, Humana’s leadership will play a crucial role in shaping the future of healthcare for millions of seniors. By prioritizing value-based care, advocating for policy changes, and addressing health equity, Humana is poised to make a lasting impact on the lives of its members. The company’s measured support for Medicare Advantage reflects a deep understanding of the challenges and opportunities within the healthcare system, positioning it as a trusted partner for seniors navigating their healthcare journey.