HIMSSCast: Understanding Patient Preferences for AI in Healthcare
The integration of artificial intelligence (AI) in healthcare has been a topic of significant discussion and research in recent years. As healthcare systems evolve, understanding patient preferences for AI technologies becomes crucial for successful implementation. HIMSSCast, a podcast by the Healthcare Information and Management Systems Society (HIMSS), delves into these preferences, exploring how AI can enhance patient care while addressing concerns and expectations. This article will explore five key subtopics related to patient preferences for AI in healthcare, providing insights into the current landscape, challenges, and future directions.
1. The Current Landscape of AI in Healthcare
AI technologies are increasingly being adopted in various healthcare settings, from diagnostics to patient management. The current landscape reflects a growing acceptance of AI tools among healthcare providers and patients alike. According to a report by Accenture, the AI health market is expected to reach $6.6 billion by 2021, indicating a robust growth trajectory.
AI applications in healthcare can be categorized into several areas:
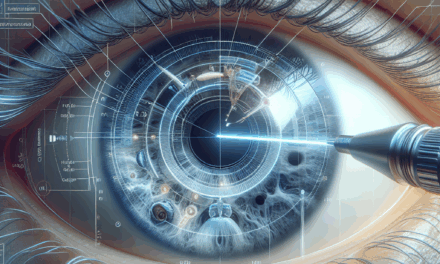
- Diagnostic Tools: AI algorithms are being used to analyze medical images, such as X-rays and MRIs, with remarkable accuracy. For instance, Google’s DeepMind has developed AI that can detect eye diseases as accurately as human specialists.
- Predictive Analytics: AI can analyze patient data to predict health outcomes, enabling proactive interventions. For example, hospitals are using AI to predict patient readmissions, allowing for targeted care plans.
- Personalized Medicine: AI helps tailor treatments based on individual patient data, improving efficacy and reducing side effects. This approach is particularly evident in oncology, where AI analyzes genetic information to recommend personalized therapies.
- Administrative Efficiency: AI streamlines administrative tasks, such as scheduling and billing, freeing up healthcare professionals to focus on patient care.
- Telehealth and Virtual Assistants: AI-powered chatbots and virtual assistants are enhancing telehealth services, providing patients with immediate responses to their queries and facilitating remote consultations.
Despite these advancements, the integration of AI in healthcare is not without challenges. Concerns about data privacy, algorithmic bias, and the potential for job displacement among healthcare workers are prevalent. Understanding patient preferences regarding these issues is essential for fostering trust and acceptance of AI technologies.
2. Patient Attitudes Towards AI in Healthcare
Patient attitudes towards AI in healthcare are shaped by various factors, including personal experiences, cultural beliefs, and awareness of AI technologies. A survey conducted by the Pew Research Center found that 60% of Americans are optimistic about the potential of AI in healthcare, while 40% express concerns about its implications.
Several key themes emerge when examining patient attitudes towards AI:
- Trust in Technology: Trust is a significant factor influencing patient acceptance of AI. Patients are more likely to embrace AI tools when they perceive them as reliable and beneficial. For instance, a study published in the Journal of Medical Internet Research found that patients who had positive experiences with AI-driven tools were more likely to recommend them to others.
- Concerns About Privacy: Data privacy remains a critical concern for patients. Many individuals worry about how their health data will be used and shared. A survey by IBM found that 75% of respondents were concerned about the security of their health information when using AI technologies.
- Desire for Human Interaction: While patients appreciate the efficiency of AI, many still value human interaction in healthcare. A study by the American Medical Association revealed that 70% of patients prefer to discuss their health concerns with a human provider rather than an AI system.
- Awareness and Understanding: Patient awareness of AI technologies significantly impacts their attitudes. Those who are informed about AI’s capabilities and limitations are more likely to have positive perceptions. Educational initiatives can help bridge this knowledge gap.
- Perceived Benefits: Patients are more inclined to accept AI when they perceive clear benefits, such as improved diagnosis accuracy, faster service, and personalized care. Highlighting these advantages can enhance patient acceptance.
Understanding these attitudes is crucial for healthcare providers and technology developers. By addressing patient concerns and emphasizing the benefits of AI, stakeholders can foster a more positive perception of AI technologies in healthcare.
3. Ethical Considerations in AI Implementation
The implementation of AI in healthcare raises several ethical considerations that must be addressed to ensure patient trust and safety. These ethical dilemmas often revolve around issues of bias, transparency, and accountability.
Key ethical considerations include:
- Algorithmic Bias: AI systems are only as good as the data they are trained on. If the training data is biased, the AI’s decisions may also be biased, leading to disparities in care. For example, a study published in the journal Science found that an AI algorithm used in dermatology was less accurate in diagnosing skin conditions in patients with darker skin tones.
- Transparency and Explainability: Patients have the right to understand how AI systems make decisions that affect their health. The “black box” nature of many AI algorithms can lead to mistrust. Efforts to develop explainable AI are essential to ensure that patients can comprehend the rationale behind AI-driven recommendations.
- Informed Consent: Patients should be informed about the use of AI in their care and provide consent for its application. This includes understanding how their data will be used and the potential risks involved.
- Accountability: Determining accountability in cases where AI systems make errors is complex. Clear guidelines must be established to delineate the responsibilities of healthcare providers, technology developers, and institutions.
- Equity in Access: Ensuring equitable access to AI technologies is crucial. Disparities in access to technology can exacerbate existing health inequalities. Policymakers must consider how to make AI tools available to underserved populations.
Addressing these ethical considerations is vital for building trust among patients and ensuring that AI technologies are implemented responsibly in healthcare settings. Engaging patients in discussions about these issues can also enhance their understanding and acceptance of AI.
4. Case Studies: Successful AI Integration in Healthcare
Several healthcare organizations have successfully integrated AI technologies, demonstrating the potential benefits and addressing patient preferences. These case studies provide valuable insights into best practices for AI implementation.
One notable example is the use of AI in radiology at the University of California, San Francisco (UCSF). The institution implemented an AI system to assist radiologists in detecting breast cancer in mammograms. The AI tool was trained on a diverse dataset, which helped reduce algorithmic bias. As a result, the accuracy of breast cancer detection improved significantly, leading to earlier diagnoses and better patient outcomes. Patient feedback indicated a high level of satisfaction with the AI-assisted process, as it reduced wait times for results and increased confidence in diagnoses.
Another successful case is the use of AI in predictive analytics at Mount Sinai Health System in New York City. The health system developed an AI model to predict patient deterioration in real-time. By analyzing electronic health records (EHRs), the model identified patients at risk of complications, allowing healthcare providers to intervene proactively. This initiative not only improved patient outcomes but also garnered positive feedback from patients who appreciated the proactive approach to their care.
In the realm of telehealth, the implementation of AI chatbots at the Cleveland Clinic has transformed patient interactions. The chatbots provide immediate responses to patient inquiries, schedule appointments, and offer health information. Patient surveys revealed that 80% of users found the chatbot helpful, citing convenience and efficiency as key benefits. This case highlights how AI can enhance patient engagement while addressing the demand for timely information.
These case studies illustrate that successful AI integration requires a focus on patient preferences, ethical considerations, and continuous evaluation of outcomes. By learning from these examples, healthcare organizations can develop strategies to implement AI technologies effectively.
5. The Future of AI in Healthcare: Trends and Predictions
The future of AI in healthcare is promising, with several trends and predictions shaping its trajectory. As technology continues to evolve, understanding these trends will be essential for stakeholders in the healthcare ecosystem.
Key trends include:
- Increased Personalization: AI will play a pivotal role in personalizing patient care. By analyzing vast amounts of data, AI can help tailor treatments to individual patients, improving outcomes and patient satisfaction.
- Integration with Wearable Technology: The rise of wearable devices will enhance the capabilities of AI in healthcare. Real-time data from wearables can be analyzed by AI algorithms to monitor patient health continuously and provide timely interventions.
- Expansion of Telehealth Services: The COVID-19 pandemic accelerated the adoption of telehealth, and AI will continue to enhance these services. AI-driven virtual assistants will improve patient interactions, making telehealth more efficient and accessible.
- Focus on Health Equity: Addressing health disparities will be a priority in the future of AI in healthcare. Efforts to ensure equitable access to AI technologies will be essential for promoting health equity among diverse populations.
- Regulatory Developments: As AI technologies become more prevalent, regulatory frameworks will evolve to ensure safety and efficacy. Policymakers will need to establish guidelines that balance innovation with patient protection.
In conclusion, the future of AI in healthcare holds immense potential for improving patient care and outcomes. However, understanding patient preferences, addressing ethical considerations, and learning from successful case studies will be crucial for realizing this potential. By fostering trust and collaboration among patients, healthcare providers, and technology developers, the healthcare industry can harness the power of AI to create a more efficient, personalized, and equitable healthcare system.
Conclusion
As we navigate the complexities of integrating AI into healthcare, understanding patient preferences is paramount. The current landscape of AI in healthcare showcases its potential to enhance diagnostics, personalize treatment, and improve administrative efficiency. However, patient attitudes towards AI reveal a mix of optimism and concern, highlighting the need for transparency, trust, and human interaction.
Ethical considerations surrounding algorithmic bias, informed consent, and accountability must be addressed to foster patient trust. Successful case studies demonstrate that when patient preferences are prioritized, AI can lead to improved outcomes and satisfaction. Looking ahead, trends such as increased personalization, integration with wearable technology, and a focus on health equity will shape the future of AI in healthcare.
Ultimately, the journey towards effective AI integration in healthcare requires collaboration among all stakeholders. By prioritizing patient preferences and addressing ethical concerns, the healthcare industry can unlock the full potential of AI, paving the way for a more efficient, equitable, and patient-centered healthcare system.