HHS Watchdog Alleges CVS Medicare Advantage Plan Engaged in Upcoding Practices
The healthcare landscape in the United States is complex, particularly when it comes to Medicare Advantage plans. Recently, the Department of Health and Human Services (HHS) Office of Inspector General (OIG) has raised serious allegations against CVS Health regarding its Medicare Advantage plans. The allegations center around upcoding practices, which could have significant implications for both the company and the millions of beneficiaries enrolled in its plans. This article delves into the details of these allegations, the implications for stakeholders, and the broader context of Medicare Advantage plans.
Understanding Medicare Advantage Plans
Medicare Advantage plans, also known as Medicare Part C, are an alternative to traditional Medicare. These plans are offered by private insurance companies and provide coverage for hospital and medical services. They often include additional benefits such as vision, dental, and wellness programs. Understanding the structure and function of these plans is crucial to grasping the implications of the HHS allegations against CVS.
- Structure of Medicare Advantage Plans: Medicare Advantage plans are required to cover all services that Original Medicare covers, but they can also offer additional benefits. They typically operate under a managed care model, which means they may require members to use a network of doctors and hospitals.
- Payment Model: The Centers for Medicare & Medicaid Services (CMS) pays Medicare Advantage plans a fixed amount per enrollee, which is adjusted based on the health status of the members. This is where upcoding can become a concern, as plans may have an incentive to report higher levels of illness to receive higher payments.
- Enrollment Trends: Enrollment in Medicare Advantage plans has been steadily increasing. As of 2023, over 28 million Americans are enrolled in these plans, representing nearly half of all Medicare beneficiaries. This growth has attracted significant attention from regulators and watchdogs.
- Benefits and Drawbacks: While Medicare Advantage plans can offer lower out-of-pocket costs and additional benefits, they can also limit provider choice and may have more complex rules regarding coverage. Understanding these trade-offs is essential for beneficiaries.
- Regulatory Oversight: The CMS oversees Medicare Advantage plans, ensuring compliance with federal regulations. However, the complexity of the system can lead to challenges in enforcement and oversight.
The Allegations Against CVS Health
The HHS OIG’s allegations against CVS Health are serious and could have far-reaching consequences. The watchdog claims that CVS engaged in upcoding practices, which involve coding a patient’s diagnosis in a way that suggests a higher level of illness than is accurate. This practice can lead to inflated payments from Medicare, raising ethical and legal concerns.
- Definition of Upcoding: Upcoding occurs when healthcare providers report a diagnosis that is more severe than what the patient actually has. This can result in higher reimbursement rates from Medicare, which is based on the reported health status of beneficiaries.
- Specific Allegations: The OIG’s report details instances where CVS allegedly submitted claims that misrepresented the health status of its members. For example, patients with mild conditions may have been coded as having more severe illnesses, leading to increased payments.
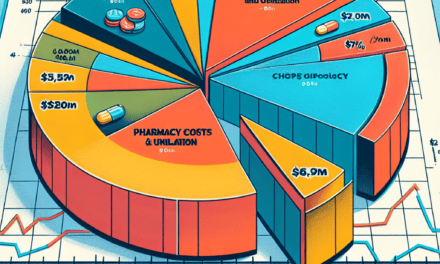
- Impact on Medicare Costs: Upcoding practices can significantly inflate costs for the Medicare program. According to estimates, improper payments due to upcoding could amount to billions of dollars annually, straining the Medicare system and potentially leading to cuts in benefits or increased premiums for beneficiaries.
- Legal Ramifications: If the allegations are proven true, CVS could face substantial penalties, including fines and repayment of overpayments. Additionally, executives could face criminal charges if found complicit in fraudulent activities.
- Response from CVS Health: CVS has publicly denied the allegations, asserting that it adheres to all regulatory guidelines and that its coding practices are compliant with CMS requirements. The company has stated that it is committed to providing high-quality care to its members.
The Broader Implications of Upcoding in Medicare Advantage
The allegations against CVS Health are not isolated; they reflect a broader issue within the Medicare Advantage system. Upcoding practices can have significant implications for the healthcare system, beneficiaries, and taxpayers.
- Impact on Beneficiaries: If upcoding leads to inflated costs for Medicare, beneficiaries may face higher premiums and reduced benefits. This can disproportionately affect low-income seniors who rely on Medicare for their healthcare needs.
- Taxpayer Burden: The financial implications of upcoding extend beyond beneficiaries. Taxpayers ultimately fund Medicare, and inflated payments due to upcoding practices can lead to increased federal spending, which may necessitate cuts in other areas of the budget.
- Market Competition: Upcoding can distort competition among Medicare Advantage plans. Companies that engage in unethical practices may gain an unfair advantage over those that comply with regulations, undermining the integrity of the market.
- Regulatory Response: The HHS OIG’s investigation may prompt increased scrutiny of Medicare Advantage plans as a whole. This could lead to more stringent regulations and oversight, impacting how these plans operate in the future.
- Public Trust: Allegations of fraud and abuse can erode public trust in the healthcare system. If beneficiaries believe that plans are engaging in unethical practices, they may be less likely to enroll in Medicare Advantage plans, which could have long-term consequences for the program.
Case Studies and Examples of Upcoding Practices
To better understand the implications of upcoding practices, it is helpful to examine specific case studies and examples from the healthcare industry. These cases illustrate the potential consequences of such practices and highlight the need for vigilance in regulatory oversight.
- Case Study 1: UnitedHealth Group: In 2017, UnitedHealth Group agreed to pay $125 million to settle allegations of upcoding practices. The company was accused of exaggerating the health status of its Medicare Advantage members to receive higher payments from Medicare. This case underscores the financial risks associated with upcoding and the potential for legal repercussions.
- Case Study 2: Anthem Inc.: In 2020, Anthem faced scrutiny for its coding practices after a whistleblower alleged that the company engaged in upcoding to inflate its risk scores. The case highlighted the challenges of ensuring compliance within large healthcare organizations and the importance of internal controls to prevent fraudulent activities.
- Case Study 3: Aetna: Aetna was also implicated in upcoding allegations, leading to a $1 million settlement in 2019. The case involved claims that Aetna had submitted inaccurate diagnosis codes to increase reimbursement rates. This example illustrates the ongoing challenges in regulating Medicare Advantage plans and the need for robust oversight mechanisms.
- Case Study 4: Humana: Humana faced allegations of upcoding in 2021, with reports indicating that the company had submitted claims that misrepresented the health status of its members. The case prompted investigations by federal regulators and raised questions about the company’s compliance practices.
- Case Study 5: Cigna: Cigna has also been scrutinized for its coding practices, with allegations of upcoding leading to investigations by the OIG. The case highlights the need for transparency and accountability in the Medicare Advantage market.
Future Outlook and Recommendations
The allegations against CVS Health regarding upcoding practices raise important questions about the future of Medicare Advantage plans and the regulatory environment surrounding them. As the healthcare landscape continues to evolve, stakeholders must consider how to address these challenges effectively.
- Increased Oversight: Regulatory agencies must enhance their oversight of Medicare Advantage plans to prevent upcoding and other fraudulent practices. This may involve more frequent audits and stricter penalties for non-compliance.
- Transparency Initiatives: Promoting transparency in coding practices can help build trust among beneficiaries and taxpayers. Insurance companies should be encouraged to disclose their coding methodologies and risk adjustment processes.
- Education and Training: Healthcare providers and insurance companies should invest in education and training programs to ensure that staff understand the importance of accurate coding and the potential consequences of upcoding.
- Whistleblower Protections: Strengthening protections for whistleblowers can encourage individuals to report fraudulent practices without fear of retaliation. This can help uncover unethical behavior and promote accountability within the industry.
- Collaboration with Stakeholders: Collaboration between regulators, insurance companies, and healthcare providers is essential to address the challenges posed by upcoding. By working together, stakeholders can develop solutions that benefit both the healthcare system and beneficiaries.
Conclusion
The allegations against CVS Health regarding upcoding practices in its Medicare Advantage plans highlight significant issues within the healthcare system. As the HHS OIG investigates these claims, it is crucial for stakeholders to understand the implications of upcoding for beneficiaries, taxpayers, and the integrity of the Medicare program. The need for increased oversight, transparency, and collaboration among stakeholders has never been more apparent. By addressing these challenges head-on, we can work towards a more equitable and efficient healthcare system that serves the needs of all Americans.