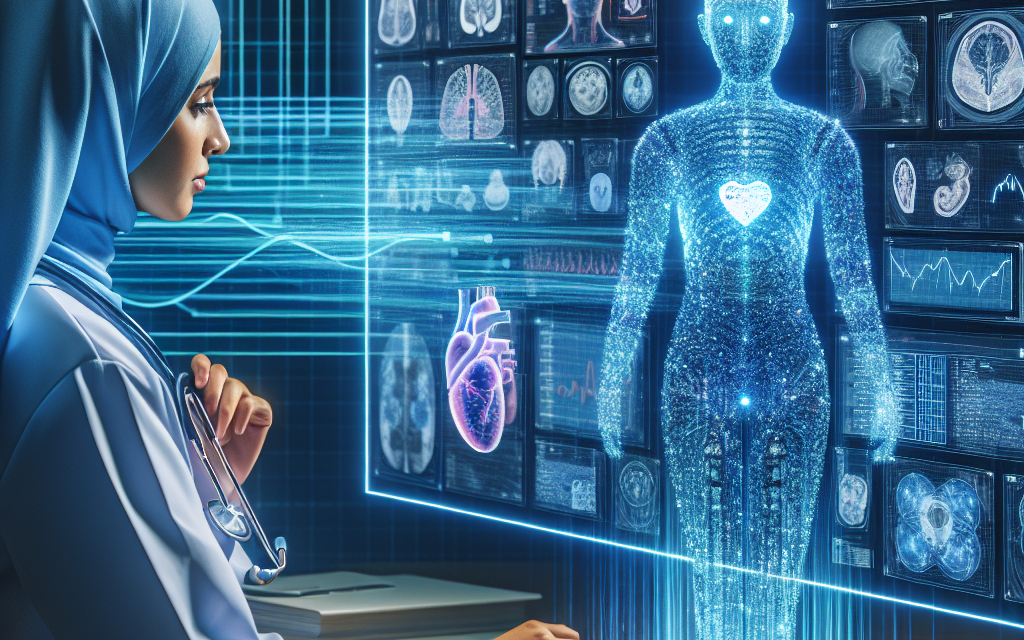
Harmonizing Human Insight and Automated Intelligence in EHRs
Electronic Health Records (EHRs) have revolutionized the way healthcare providers manage patient information. However, the integration of human insight and automated intelligence within these systems remains a complex challenge. This article explores the intersection of human expertise and machine learning in EHRs, emphasizing the importance of harmonizing these elements to enhance patient care, improve clinical outcomes, and streamline healthcare operations.
The Role of EHRs in Modern Healthcare
Electronic Health Records serve as digital versions of patients’ paper charts, providing a comprehensive view of patient health history. EHRs are designed to streamline the clinician’s workflow, improve the quality of care, and enhance patient safety. The adoption of EHRs has been driven by several factors:
- Regulatory Requirements: Government initiatives, such as the HITECH Act, have incentivized healthcare providers to adopt EHR systems.
- Improved Accessibility: EHRs allow for real-time access to patient data, facilitating better decision-making.
- Enhanced Coordination: EHRs enable seamless communication among healthcare providers, improving care coordination.
- Data Analytics: EHRs provide a wealth of data that can be analyzed to improve patient outcomes and operational efficiency.
Despite these advantages, the integration of human insight and automated intelligence in EHRs is crucial for maximizing their potential. While EHRs can store and process vast amounts of data, they lack the nuanced understanding that human clinicians bring to patient care.
Understanding Human Insight in Healthcare
Human insight in healthcare refers to the knowledge, experience, and intuition that healthcare professionals possess. This insight is critical for making informed clinical decisions, diagnosing conditions, and developing treatment plans. Several factors contribute to the value of human insight:
- Clinical Experience: Healthcare professionals draw on years of training and experience to interpret data and make decisions.
- Patient Interaction: Clinicians can assess non-verbal cues and emotional states that are not captured in EHRs.
- Ethical Considerations: Human insight allows for ethical decision-making that considers the patient’s values and preferences.
- Contextual Understanding: Clinicians can contextualize data within the broader scope of a patient’s life, including social determinants of health.
For example, a physician may notice subtle changes in a patient’s behavior or mood that indicate a potential mental health issue, even if the EHR data does not explicitly suggest it. This ability to synthesize information from various sources is what makes human insight invaluable in healthcare.
The Rise of Automated Intelligence in EHRs
Automated intelligence, often referred to as artificial intelligence (AI), has made significant inroads into healthcare, particularly in the realm of EHRs. AI technologies can analyze vast amounts of data quickly and accurately, providing insights that can enhance clinical decision-making. Key applications of AI in EHRs include:
- Predictive Analytics: AI algorithms can identify patterns in patient data to predict outcomes, such as the likelihood of hospital readmission.
- Natural Language Processing (NLP): NLP enables EHRs to extract meaningful information from unstructured data, such as clinical notes.
- Clinical Decision Support: AI can provide real-time recommendations based on patient data, helping clinicians make informed decisions.
- Automated Documentation: AI can assist in generating clinical documentation, reducing the administrative burden on healthcare providers.
For instance, a study published in the Journal of the American Medical Association found that AI algorithms could accurately predict patient deterioration by analyzing EHR data, allowing for timely interventions. This demonstrates the potential of automated intelligence to enhance patient safety and improve outcomes.
Challenges in Harmonizing Human Insight and Automated Intelligence
While the integration of human insight and automated intelligence in EHRs holds great promise, several challenges must be addressed to achieve effective harmonization:
- Data Quality: The effectiveness of AI algorithms depends on the quality of the data fed into them. Inaccurate or incomplete data can lead to erroneous conclusions.
- Trust in AI: Clinicians may be hesitant to rely on AI recommendations if they do not understand how the algorithms work or if they lack transparency.
- Workflow Integration: Integrating AI tools into existing workflows can be challenging, requiring changes in processes and training for healthcare providers.
- Ethical Concerns: The use of AI raises ethical questions regarding patient privacy, data security, and the potential for bias in algorithms.
Addressing these challenges requires a collaborative approach that involves healthcare providers, technology developers, and policymakers. For example, organizations can implement training programs to educate clinicians about AI tools and their benefits, fostering trust and acceptance.
Case Studies: Successful Integration of Human Insight and AI in EHRs
Several healthcare organizations have successfully integrated human insight and automated intelligence in their EHR systems, leading to improved patient care and operational efficiency. Here are a few notable case studies:
- Mount Sinai Health System: Mount Sinai implemented an AI-driven clinical decision support system that analyzes EHR data to identify patients at risk for sepsis. The system alerts clinicians in real-time, allowing for timely interventions. As a result, the health system reported a significant reduction in sepsis-related mortality rates.
- Geisinger Health System: Geisinger developed an AI tool that analyzes patient data to recommend personalized treatment plans for chronic diseases. By combining AI insights with clinician expertise, the health system improved patient adherence to treatment and reduced hospital readmissions.
- Partners HealthCare: Partners HealthCare utilized natural language processing to extract information from unstructured clinical notes in their EHRs. This enabled clinicians to access relevant patient information more efficiently, enhancing decision-making and improving care coordination.
These case studies illustrate the potential benefits of harmonizing human insight and automated intelligence in EHRs. By leveraging the strengths of both elements, healthcare organizations can enhance patient outcomes and streamline operations.
Future Directions: The Path to Harmonization
The future of EHRs lies in the successful integration of human insight and automated intelligence. To achieve this, several strategies can be employed:
- Interdisciplinary Collaboration: Encouraging collaboration between clinicians, data scientists, and technology developers can lead to the creation of AI tools that align with clinical workflows and enhance decision-making.
- Continuous Training: Ongoing education and training for healthcare providers on AI technologies can foster trust and improve adoption rates.
- Patient-Centric Design: EHR systems should be designed with the end-user in mind, ensuring that they are intuitive and user-friendly for clinicians.
- Ethical Frameworks: Establishing ethical guidelines for the use of AI in healthcare can address concerns related to bias, privacy, and data security.
As technology continues to evolve, the potential for harmonizing human insight and automated intelligence in EHRs will only grow. By embracing this integration, healthcare organizations can enhance patient care, improve clinical outcomes, and create a more efficient healthcare system.
Conclusion
The harmonization of human insight and automated intelligence in Electronic Health Records is essential for maximizing the potential of these systems. While EHRs provide valuable data and insights, the expertise and intuition of healthcare professionals remain irreplaceable. By addressing the challenges of data quality, trust, workflow integration, and ethical concerns, healthcare organizations can successfully integrate AI tools into their EHR systems.
Case studies from leading healthcare organizations demonstrate the tangible benefits of this integration, including improved patient outcomes and enhanced operational efficiency. Looking ahead, a collaborative approach that emphasizes interdisciplinary teamwork, continuous training, patient-centric design, and ethical frameworks will be crucial for achieving successful harmonization.
In conclusion, the future of healthcare lies in the seamless integration of human insight and automated intelligence, paving the way for a more effective, efficient, and patient-centered healthcare system.