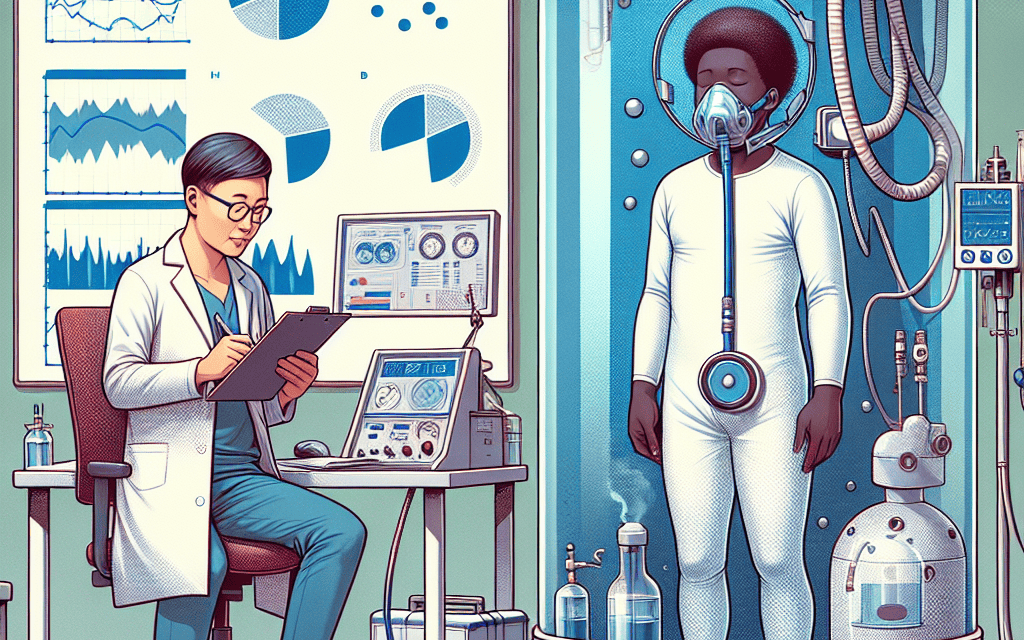
Exploring the Health Benefits of Hyperbaric Oxygen Therapy: A Scientific Perspective
Hyperbaric Oxygen Therapy (HBOT) has gained significant attention in recent years as a treatment modality for various medical conditions. This therapy involves breathing pure oxygen in a pressurized environment, which can enhance the body’s natural healing processes. In this article, we will explore the health benefits of HBOT from a scientific perspective, delving into its mechanisms, applications, and the evidence supporting its use.
1. Understanding Hyperbaric Oxygen Therapy
Hyperbaric Oxygen Therapy is defined as a medical treatment that involves the inhalation of 100% oxygen while in a pressurized chamber. The therapy is typically administered in a hyperbaric chamber, where atmospheric pressure is increased to greater than sea level. This increase in pressure allows more oxygen to dissolve in the blood plasma, leading to enhanced oxygen delivery to tissues throughout the body.
The fundamental principle behind HBOT is based on Henry’s Law, which states that the amount of gas that dissolves in a liquid is proportional to the pressure of that gas above the liquid. In the context of HBOT, this means that under higher pressure, more oxygen can be absorbed into the bloodstream, which can be beneficial for various medical conditions.
HBOT is not a new concept; it has been used since the early 20th century, primarily for treating decompression sickness in divers. Over the years, its applications have expanded to include a range of conditions, from chronic wounds to neurological disorders. The therapy is typically administered in sessions lasting from 30 minutes to two hours, depending on the condition being treated.
2. Mechanisms of Action
The therapeutic effects of HBOT can be attributed to several mechanisms that enhance healing and recovery. Understanding these mechanisms is crucial for appreciating the potential benefits of this therapy.
2.1 Enhanced Oxygen Delivery
One of the primary mechanisms of HBOT is the increased availability of oxygen to tissues. Under normal circumstances, oxygen is transported in the blood primarily by hemoglobin in red blood cells. However, during HBOT, oxygen is also dissolved directly into the plasma, allowing for greater oxygen delivery to hypoxic tissues. This is particularly beneficial in conditions where blood flow is compromised, such as in chronic wounds or after radiation therapy.
2.2 Anti-Inflammatory Effects
HBOT has been shown to exert anti-inflammatory effects, which can be beneficial in various medical conditions. The therapy can reduce the production of pro-inflammatory cytokines and promote the release of anti-inflammatory mediators. This modulation of the inflammatory response can aid in the healing process and reduce tissue damage.
2.3 Angiogenesis Promotion
Another significant mechanism of HBOT is its ability to promote angiogenesis, the formation of new blood vessels. Increased oxygen levels stimulate the production of vascular endothelial growth factor (VEGF), a key protein involved in blood vessel formation. This is particularly important in conditions such as diabetic ulcers, where poor circulation hampers healing.
2.4 Enhanced Stem Cell Mobilization
Recent studies have suggested that HBOT may enhance the mobilization of stem cells from the bone marrow into the bloodstream. These stem cells play a crucial role in tissue repair and regeneration. By increasing the availability of stem cells, HBOT may facilitate faster healing and recovery from injuries.
2.5 Bactericidal Effects
HBOT has demonstrated bactericidal effects against certain types of bacteria, particularly anaerobic bacteria that thrive in low-oxygen environments. The high levels of oxygen can inhibit the growth of these pathogens, making HBOT a valuable adjunctive treatment for infections, particularly in cases of chronic osteomyelitis or non-healing wounds.
3. Clinical Applications of Hyperbaric Oxygen Therapy
HBOT has a wide range of clinical applications, with several conditions showing promising results from this therapy. Below are some of the most notable applications supported by scientific evidence.
3.1 Wound Healing
Chronic wounds, such as diabetic foot ulcers and pressure sores, pose significant challenges in medical treatment. HBOT has been shown to enhance wound healing by improving oxygen delivery, reducing inflammation, and promoting angiogenesis. A study published in the journal “Wound Repair and Regeneration” found that patients receiving HBOT for diabetic foot ulcers had a significantly higher rate of complete healing compared to those receiving standard care alone.
3.2 Radiation Injury
Patients undergoing radiation therapy for cancer often experience tissue damage due to radiation exposure. HBOT has been used as a treatment for radiation-induced tissue injury, particularly in cases of osteoradionecrosis (bone death due to radiation). Research indicates that HBOT can improve healing and reduce complications in these patients, making it a valuable adjunctive therapy.
3.3 Neurological Conditions
HBOT has shown promise in treating various neurological conditions, including traumatic brain injury (TBI) and stroke. A study published in “Neurorehabilitation and Neural Repair” reported that patients with TBI who received HBOT demonstrated improved cognitive function and reduced symptoms of post-concussion syndrome. Similarly, stroke patients may benefit from HBOT by enhancing recovery and reducing brain damage.
3.4 Infections
As mentioned earlier, HBOT has bactericidal effects, making it useful in treating certain infections. It is particularly effective against anaerobic infections, such as those caused by Clostridium species. A systematic review published in “The Journal of Infection” concluded that HBOT is a valuable adjunctive treatment for chronic osteomyelitis and other difficult-to-treat infections.
3.5 Sports Medicine and Recovery
A growing area of interest is the use of HBOT in sports medicine and recovery. Athletes often experience injuries that require rapid healing and recovery. Some studies suggest that HBOT may enhance recovery from sports-related injuries by reducing inflammation, promoting tissue repair, and improving overall performance. However, more research is needed to establish standardized protocols and outcomes in this area.
4. Evidence and Research Supporting HBOT
The efficacy of Hyperbaric Oxygen Therapy has been supported by numerous studies and clinical trials. Understanding the evidence behind its applications is essential for evaluating its role in modern medicine.
4.1 Systematic Reviews and Meta-Analyses
Several systematic reviews and meta-analyses have been conducted to assess the effectiveness of HBOT for various conditions. For instance, a meta-analysis published in “The Cochrane Database of Systematic Reviews” evaluated the use of HBOT for chronic wounds and found that it significantly improved healing rates compared to standard care. Such reviews provide a comprehensive overview of the available evidence and help guide clinical practice.
4.2 Randomized Controlled Trials
Randomized controlled trials (RCTs) are considered the gold standard in clinical research. Numerous RCTs have investigated the effects of HBOT on conditions such as diabetic foot ulcers, radiation injuries, and traumatic brain injuries. For example, an RCT published in “JAMA Surgery” demonstrated that patients with diabetic foot ulcers who received HBOT had a higher rate of healing compared to those receiving placebo treatment.
4.3 Case Studies
In addition to large-scale studies, individual case studies have highlighted the potential benefits of HBOT in specific patients. For instance, a case study published in “The Journal of Hyperbaric Medicine” described a patient with severe radiation-induced tissue damage who experienced significant improvement after undergoing HBOT. Such case studies provide valuable insights into the therapy’s effectiveness in real-world scenarios.
4.4 Guidelines and Recommendations
Various medical organizations have developed guidelines for the use of HBOT in specific conditions. The Undersea and Hyperbaric Medical Society (UHMS) provides recommendations for the use of HBOT in conditions such as carbon monoxide poisoning, decompression sickness, and chronic non-healing wounds. These guidelines are based on the available evidence and help clinicians make informed decisions regarding treatment.
4.5 Limitations and Controversies
Despite the promising evidence supporting HBOT, there are limitations and controversies surrounding its use. Some critics argue that the therapy is overused for conditions with limited evidence, leading to unnecessary costs and potential risks. Additionally, the lack of standardized protocols for treatment duration and pressure levels can lead to variability in outcomes. Ongoing research is essential to address these concerns and refine the application of HBOT in clinical practice.
5. Safety and Considerations
While HBOT is generally considered safe, it is essential to be aware of potential risks and contraindications associated with the therapy. Understanding these factors is crucial for ensuring patient safety and optimizing treatment outcomes.
5.1 Potential Risks and Side Effects
HBOT is associated with some risks, although serious complications are rare. Common side effects include:
- Barotrauma: Damage to the ears or lungs due to pressure changes.
- Oxygen toxicity: High levels of oxygen can lead to seizures or lung damage in rare cases.
- Claustrophobia: Some patients may experience anxiety or discomfort in the hyperbaric chamber.
It is essential for healthcare providers to monitor patients closely during treatment and address any concerns that may arise.
5.2 Contraindications
Certain medical conditions may contraindicate the use of HBOT. These include:
- Untreated pneumothorax: A collapsed lung can be exacerbated by increased pressure.
- Certain types of chemotherapy: Some chemotherapeutic agents may interact negatively with oxygen therapy.
- Severe respiratory conditions: Patients with certain lung diseases may not tolerate increased oxygen levels.
Before initiating HBOT, a thorough medical evaluation is necessary to identify any contraindications and ensure patient safety.
5.3 Patient Selection
Successful outcomes with HBOT depend on appropriate patient selection. Not all patients will benefit from this therapy, and it is essential to identify those who are most likely to experience positive results. Factors to consider include:
- The underlying condition being treated.
- The severity and duration of the condition.
- Overall health status and comorbidities.
Healthcare providers should engage in shared decision-making with patients, discussing the potential benefits and risks of HBOT to ensure informed consent.
5.4 Future Directions
The field of hyperbaric medicine is continually evolving, with ongoing research exploring new applications and optimizing treatment protocols. Future studies may focus on:
- Identifying additional conditions that may benefit from HBOT.
- Standardizing treatment protocols to enhance consistency and outcomes.
- Investigating the long-term effects of HBOT on various health conditions.
As research progresses, HBOT may become an integral part of modern medical practice, offering new hope for patients with challenging health issues.
Conclusion
Hyperbaric Oxygen Therapy represents a fascinating intersection of science and medicine, offering a range of health benefits supported by a growing body of evidence. From enhancing wound healing to promoting recovery from neurological injuries, HBOT has demonstrated its potential as a valuable therapeutic tool.
As we continue to explore the mechanisms and applications of this therapy, it is essential to approach its use with a scientific perspective, grounded in evidence-based practice. While there are risks and limitations associated with HBOT, careful patient selection and adherence to established guidelines can optimize outcomes and ensure patient safety.
In summary, Hyperbaric Oxygen Therapy holds promise for various medical conditions, and ongoing research will undoubtedly uncover new insights into its efficacy and applications. As we advance our understanding of this therapy, it is crucial to remain open to its potential while maintaining a critical eye on the evidence supporting its use.