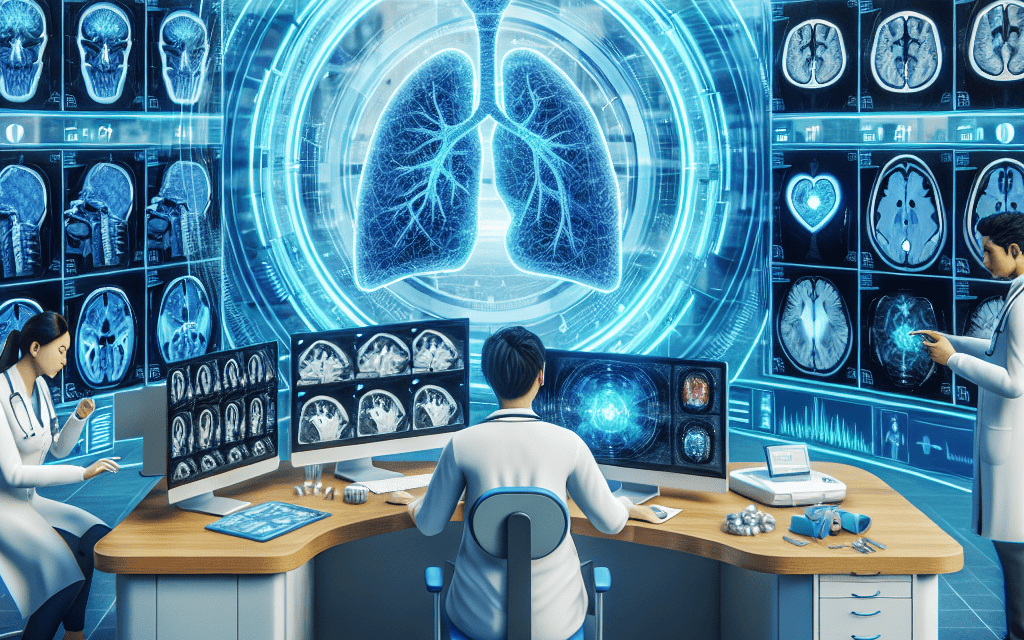
Exploring the Diverse Applications and Advantages of AI in Radiology
Artificial Intelligence (AI) is revolutionizing various fields, and radiology is no exception. The integration of AI technologies into radiology is enhancing diagnostic accuracy, improving workflow efficiency, and ultimately leading to better patient outcomes. This article delves into the diverse applications and advantages of AI in radiology, exploring its impact on diagnostics, workflow optimization, predictive analytics, patient engagement, and ethical considerations.
1. Enhancing Diagnostic Accuracy
One of the most significant applications of AI in radiology is its ability to enhance diagnostic accuracy. Traditional radiology relies heavily on the expertise of radiologists, who interpret medical images to identify abnormalities. However, human error is an inherent risk in this process. AI algorithms, particularly those based on deep learning, have shown remarkable promise in improving diagnostic precision.
AI systems can analyze vast amounts of imaging data quickly and accurately, identifying patterns that may be missed by the human eye. For instance, studies have demonstrated that AI can outperform radiologists in detecting certain conditions, such as breast cancer in mammograms. A study published in the journal *Nature* found that an AI model reduced false positives and false negatives in breast cancer detection, leading to improved diagnostic accuracy.
- Deep Learning Algorithms: These algorithms are trained on large datasets of medical images, allowing them to learn and recognize complex patterns. For example, convolutional neural networks (CNNs) have been particularly effective in image classification tasks.
- Image Segmentation: AI can assist in segmenting images to isolate areas of interest, such as tumors or lesions, making it easier for radiologists to focus on critical regions.
- Multi-modal Imaging: AI can integrate data from various imaging modalities (e.g., MRI, CT, X-ray) to provide a comprehensive view of a patient’s condition, enhancing diagnostic capabilities.
Moreover, AI can continuously learn and improve its algorithms as more data becomes available. This adaptability ensures that AI systems remain up-to-date with the latest medical knowledge and imaging techniques, further enhancing their diagnostic capabilities.
2. Optimizing Workflow Efficiency
In addition to improving diagnostic accuracy, AI is also streamlining workflow processes in radiology departments. The increasing volume of imaging studies has led to bottlenecks in radiology workflows, resulting in delays in diagnosis and treatment. AI technologies can help alleviate these challenges by automating routine tasks and optimizing resource allocation.
AI-powered tools can assist in triaging cases based on urgency, ensuring that critical cases are prioritized. For instance, an AI system can analyze incoming imaging studies and flag those that require immediate attention, allowing radiologists to focus on high-priority cases first. This triaging capability not only improves patient care but also enhances overall departmental efficiency.
- Automated Reporting: AI can generate preliminary reports based on image analysis, allowing radiologists to review and finalize reports more quickly. This automation reduces the time spent on routine reporting tasks.
- Scheduling Optimization: AI algorithms can analyze historical data to predict patient volumes and optimize scheduling, ensuring that radiology departments are adequately staffed during peak times.
- Resource Management: AI can assist in managing imaging equipment and resources, predicting maintenance needs, and minimizing downtime.
By optimizing workflow efficiency, AI not only enhances the productivity of radiology departments but also improves the overall patient experience. Patients benefit from faster diagnoses and reduced waiting times, leading to timely interventions and better health outcomes.
3. Predictive Analytics in Radiology
Predictive analytics is another area where AI is making significant strides in radiology. By analyzing historical data and identifying trends, AI can help predict patient outcomes and disease progression. This capability is particularly valuable in managing chronic conditions and guiding treatment decisions.
For example, AI algorithms can analyze imaging data alongside patient demographics and clinical history to predict the likelihood of disease recurrence or progression. This information can be invaluable for oncologists and other specialists in developing personalized treatment plans.
- Risk Stratification: AI can stratify patients based on their risk profiles, allowing healthcare providers to tailor interventions and monitoring strategies accordingly.
- Longitudinal Studies: By analyzing imaging data over time, AI can identify subtle changes that may indicate disease progression, enabling earlier interventions.
- Clinical Decision Support: AI can provide real-time recommendations to radiologists based on predictive models, enhancing clinical decision-making.
Moreover, predictive analytics can extend beyond individual patient care. By aggregating data across populations, AI can identify trends and patterns that inform public health initiatives and resource allocation. For instance, AI can help predict outbreaks of diseases based on imaging data and other health indicators, enabling proactive responses from healthcare systems.
4. Enhancing Patient Engagement and Experience
AI is also playing a crucial role in enhancing patient engagement and experience in radiology. As patients become more involved in their healthcare decisions, AI technologies can facilitate communication and education, empowering patients to take an active role in their health.
AI-driven chatbots and virtual assistants can provide patients with information about their imaging procedures, answer common questions, and guide them through the process. This support can alleviate anxiety and improve patient satisfaction. For example, a study found that patients who received pre-procedural education through AI tools reported lower anxiety levels compared to those who did not.
- Personalized Communication: AI can analyze patient data to tailor communication strategies, ensuring that patients receive relevant information based on their specific needs and preferences.
- Follow-up Care: AI can assist in scheduling follow-up appointments and sending reminders, ensuring that patients adhere to their care plans.
- Patient Portals: AI can enhance patient portals by providing personalized insights and recommendations based on imaging results, fostering a collaborative approach to healthcare.
By improving patient engagement, AI not only enhances the overall patient experience but also contributes to better health outcomes. Engaged patients are more likely to adhere to treatment plans, attend follow-up appointments, and communicate effectively with their healthcare providers.
5. Ethical Considerations and Challenges
While the advantages of AI in radiology are substantial, it is essential to address the ethical considerations and challenges associated with its implementation. As AI technologies become more integrated into clinical practice, concerns regarding data privacy, algorithmic bias, and the role of radiologists must be carefully considered.
Data privacy is a significant concern, as AI systems require access to large datasets of medical images and patient information. Ensuring that patient data is protected and used ethically is paramount. Healthcare organizations must implement robust data governance frameworks to safeguard patient privacy while leveraging AI technologies.
- Algorithmic Bias: AI algorithms can inadvertently perpetuate biases present in training data, leading to disparities in diagnostic accuracy across different populations. It is crucial to ensure that AI systems are trained on diverse datasets to mitigate this risk.
- Radiologist Role: The integration of AI into radiology raises questions about the future role of radiologists. While AI can enhance diagnostic capabilities, it is essential to recognize that human expertise remains invaluable in interpreting complex cases and making clinical decisions.
- Regulatory Frameworks: As AI technologies evolve, regulatory frameworks must adapt to ensure the safe and effective use of AI in clinical practice. Collaboration between healthcare providers, technology developers, and regulatory bodies is essential to establish guidelines and standards.
Addressing these ethical considerations is crucial for the responsible implementation of AI in radiology. By fostering transparency, accountability, and inclusivity, the healthcare industry can harness the full potential of AI while minimizing risks.
Conclusion
The integration of AI in radiology is transforming the field, offering diverse applications and significant advantages. From enhancing diagnostic accuracy to optimizing workflow efficiency, predictive analytics, improving patient engagement, and addressing ethical considerations, AI is reshaping the landscape of radiology.
As healthcare continues to evolve, the collaboration between radiologists and AI technologies will be essential in delivering high-quality patient care. By embracing these advancements while addressing ethical challenges, the radiology community can leverage AI to improve outcomes and enhance the overall healthcare experience.
In summary, the future of radiology is bright with the promise of AI. As we continue to explore its diverse applications, it is crucial to remain vigilant in addressing the challenges that accompany this technological revolution. With a thoughtful approach, AI can be a powerful ally in the pursuit of excellence in radiology and patient care.