Evaluating Healthcare: A Global Comparison of the U.S. System

The healthcare system in the United States is often a topic of intense debate and scrutiny. With its unique blend of private and public funding, the U.S. healthcare system stands apart from those of other developed nations. This article aims to provide a comprehensive evaluation of the U.S. healthcare system by comparing it with systems in other countries. We will explore various aspects such as cost, quality, accessibility, and outcomes, providing a detailed analysis of how the U.S. measures up on the global stage.
1. Healthcare Expenditure: A Financial Overview
One of the most striking features of the U.S. healthcare system is its high expenditure. The United States spends more on healthcare per capita than any other country in the world. In 2020, healthcare spending in the U.S. reached approximately $4.1 trillion, which equates to about 19.7% of the nation’s GDP. This section will delve into the reasons behind these high costs and compare them with other countries.
Several factors contribute to the high cost of healthcare in the U.S. These include administrative costs, high prices for medical services and pharmaceuticals, and the prevalence of chronic diseases. Administrative costs alone account for about 8% of total healthcare spending, which is significantly higher than in other countries. The complexity of billing and insurance-related activities in the U.S. adds to these costs.
Pharmaceutical prices in the U.S. are also among the highest in the world. For instance, the cost of insulin in the U.S. is several times higher than in countries like Canada and the UK. This is partly due to the lack of price regulation and the influence of pharmaceutical companies in the U.S. market.
In contrast, countries with universal healthcare systems, such as the UK and Canada, have mechanisms in place to control costs. These include negotiating drug prices and setting limits on the fees that healthcare providers can charge. As a result, these countries spend significantly less on healthcare while achieving comparable or better health outcomes.
- Administrative costs: 8% of total spending
- Pharmaceutical prices: Among the highest globally
- Chronic disease prevalence: A significant cost driver
Despite the high expenditure, the U.S. does not necessarily achieve better health outcomes compared to other countries. This raises questions about the efficiency and effectiveness of the U.S. healthcare system, which will be explored further in subsequent sections.
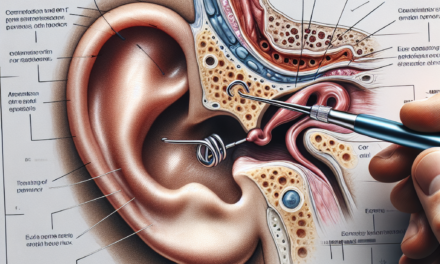
2. Quality of Care: Measuring Outcomes
Quality of care is a critical component of any healthcare system. It encompasses various factors, including patient safety, effectiveness of treatments, and patient satisfaction. In this section, we will evaluate the quality of care in the U.S. and compare it with other countries.
The U.S. healthcare system is renowned for its advanced medical technology and highly skilled healthcare professionals. It leads in medical research and innovation, contributing to groundbreaking treatments and procedures. However, when it comes to overall health outcomes, the U.S. often lags behind other developed nations.
For example, the U.S. has a higher infant mortality rate compared to countries like Sweden and Japan. According to the World Health Organization, the U.S. ranks 33rd in infant mortality among OECD countries. Additionally, life expectancy in the U.S. is lower than in many other developed countries, with significant disparities based on socioeconomic status and race.
One area where the U.S. excels is in cancer treatment. The country has some of the highest survival rates for certain types of cancer, thanks to early detection and access to cutting-edge treatments. However, these successes are not uniformly distributed across all areas of healthcare.
- Infant mortality rate: Higher than many OECD countries
- Life expectancy: Lower than other developed nations
- Cancer treatment: High survival rates
Patient satisfaction is another important measure of quality. Surveys indicate that while Americans appreciate the quality of care they receive, they are often dissatisfied with the cost and complexity of accessing healthcare services. This dissatisfaction is a recurring theme that highlights the need for systemic reforms.
3. Accessibility: Barriers to Care
Accessibility to healthcare services is a fundamental aspect of any healthcare system. It determines whether individuals can obtain necessary medical care without facing financial or logistical barriers. In this section, we will examine the accessibility of healthcare in the U.S. and compare it with other countries.
The U.S. healthcare system is characterized by a mix of private and public insurance programs. While programs like Medicare and Medicaid provide coverage for specific populations, a significant portion of the population relies on employer-sponsored insurance or individual plans. Despite these options, millions of Americans remain uninsured or underinsured.
According to the U.S. Census Bureau, approximately 28 million Americans were uninsured in 2020. This lack of insurance coverage creates significant barriers to accessing healthcare services, as uninsured individuals are less likely to seek preventive care and more likely to delay treatment due to cost concerns.
In contrast, countries with universal healthcare systems, such as the UK and Canada, provide coverage for all citizens, ensuring that financial barriers do not prevent individuals from accessing necessary care. These systems are funded through taxation and offer a basic level of coverage to all residents.
- Uninsured Americans: Approximately 28 million in 2020
- Universal coverage: Achieved in countries like the UK and Canada
- Financial barriers: A significant issue in the U.S.
Geographic disparities also affect accessibility in the U.S. Rural areas often face shortages of healthcare providers, leading to longer travel times and wait times for patients. Telemedicine has emerged as a potential solution to these challenges, but its adoption varies across regions.
4. Health Equity: Addressing Disparities
Health equity is a critical consideration in evaluating any healthcare system. It involves ensuring that all individuals have fair and just access to healthcare services, regardless of their socioeconomic status, race, or geographic location. This section will explore health equity in the U.S. and compare it with other countries.
The U.S. healthcare system is marked by significant disparities in health outcomes based on race and socioeconomic status. For example, African Americans and Hispanic Americans experience higher rates of chronic diseases and lower life expectancy compared to their white counterparts. These disparities are influenced by factors such as access to care, quality of care, and social determinants of health.
Efforts to address health disparities in the U.S. include initiatives to expand access to care, improve cultural competence among healthcare providers, and address social determinants of health. However, progress has been slow, and disparities persist.
In contrast, countries with universal healthcare systems often achieve better health equity. For example, Sweden’s healthcare system is designed to provide equal access to care for all citizens, regardless of their socioeconomic status. This is achieved through policies that prioritize equity and social welfare.
- Racial disparities: Significant in the U.S.
- Socioeconomic disparities: Affect access and outcomes
- Universal systems: Often achieve better equity
Addressing health disparities requires a multifaceted approach that includes policy changes, community engagement, and efforts to address social determinants of health. The U.S. can learn from other countries’ experiences in promoting health equity and reducing disparities.
5. Innovations and Reforms: The Path Forward
Innovation and reform are essential for improving healthcare systems and addressing existing challenges. In this section, we will explore recent innovations and reforms in the U.S. healthcare system and compare them with initiatives in other countries.
The U.S. has been at the forefront of medical innovation, with significant advancements in areas such as telemedicine, personalized medicine, and digital health technologies. These innovations have the potential to improve access to care, enhance patient outcomes, and reduce costs.
Telemedicine, in particular, has gained traction during the COVID-19 pandemic, providing a convenient and cost-effective way for patients to access healthcare services. The expansion of telehealth services has been supported by policy changes that allow for reimbursement and regulatory flexibility.
Reforms in the U.S. healthcare system have focused on expanding access to care and controlling costs. The Affordable Care Act (ACA), enacted in 2010, aimed to increase insurance coverage and reduce healthcare costs. While the ACA has achieved some success in expanding coverage, challenges remain in terms of affordability and access.
- Telemedicine: Expanded during the COVID-19 pandemic
- Affordable Care Act: Aimed to expand coverage
- Digital health: Innovations in personalized medicine
Other countries have implemented successful reforms that the U.S. can learn from. For example, Germany’s healthcare system combines statutory health insurance with private options, providing comprehensive coverage while maintaining cost control. Similarly, Japan’s healthcare system emphasizes preventive care and cost-effective treatments.
As the U.S. continues to grapple with healthcare challenges, it can benefit from adopting best practices from other countries and fostering innovation to create a more efficient and equitable healthcare system.
Conclusion
The U.S. healthcare system is a complex and multifaceted entity that presents both strengths and challenges. While it excels in medical innovation and advanced treatments, it faces significant issues related to cost, accessibility, and equity. By comparing the U.S. system with those of other countries, we gain valuable insights into potential areas for improvement.
Key takeaways from this analysis include the need to address high healthcare costs, improve access to care, and reduce health disparities. Innovations such as telemedicine and digital health technologies offer promising solutions, but systemic reforms are necessary to achieve lasting change.
Ultimately, the path forward for the U.S. healthcare system involves learning from global best practices, fostering innovation, and prioritizing health equity to ensure that all individuals have access to high-quality, affordable healthcare services.