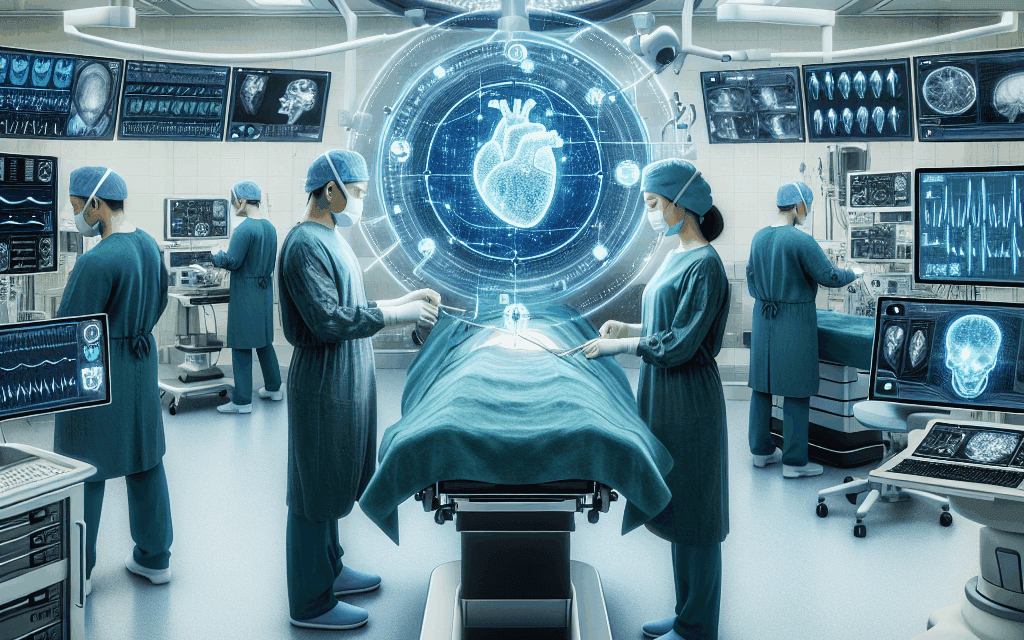
Enhancing Surgical Efficiency: The Role of AI in Hospital Operating Rooms
In recent years, the integration of artificial intelligence (AI) into healthcare has transformed various aspects of patient care, particularly in surgical settings. The operating room (OR) is a critical environment where precision, efficiency, and safety are paramount. As hospitals strive to improve surgical outcomes and reduce costs, AI technologies are emerging as powerful tools to enhance surgical efficiency. This article explores the multifaceted role of AI in hospital operating rooms, examining its applications, benefits, challenges, and future potential.
1. Understanding AI in the Surgical Context
Artificial intelligence encompasses a range of technologies that enable machines to perform tasks that typically require human intelligence. In the surgical context, AI can analyze vast amounts of data, recognize patterns, and make predictions, thereby assisting surgeons in decision-making processes. The application of AI in surgery can be categorized into several areas:
- Preoperative Planning: AI can analyze patient data to assist in surgical planning, predicting potential complications and optimizing surgical approaches.
- Intraoperative Assistance: AI systems can provide real-time data and insights during surgery, enhancing the surgeon’s capabilities.
- Postoperative Monitoring: AI can track patient recovery and identify complications early, improving postoperative care.
By leveraging machine learning algorithms and data analytics, AI can significantly enhance the surgical workflow, leading to improved patient outcomes and operational efficiency.
2. AI-Driven Preoperative Planning
Preoperative planning is a critical phase in the surgical process, where careful consideration of patient-specific factors can lead to better surgical outcomes. AI technologies are increasingly being utilized to enhance this phase through data analysis and predictive modeling.
One of the primary applications of AI in preoperative planning is the analysis of imaging data. Advanced algorithms can process medical images such as CT scans, MRIs, and X-rays to identify anatomical structures and potential complications. For instance, a study published in the journal Surgical Endoscopy demonstrated that AI algorithms could accurately identify tumors in imaging studies, allowing surgeons to tailor their approach based on precise tumor localization.
Moreover, AI can integrate data from various sources, including electronic health records (EHRs), to create comprehensive patient profiles. This integration allows for the identification of risk factors that may complicate surgery. For example, an AI system could analyze a patient’s medical history, comorbidities, and previous surgical outcomes to predict the likelihood of complications during surgery. This predictive capability enables surgeons to make informed decisions about surgical techniques and postoperative care.
Additionally, AI can assist in resource allocation by predicting the duration of surgeries and the required surgical team composition. By analyzing historical data, AI can provide estimates on how long a particular procedure is likely to take, allowing hospitals to optimize scheduling and reduce downtime in the OR.
In summary, AI-driven preoperative planning enhances surgical efficiency by:
- Improving the accuracy of imaging analysis.
- Identifying patient-specific risk factors.
- Optimizing resource allocation and scheduling.
3. Intraoperative AI Assistance
During surgery, the stakes are high, and the need for precision is critical. AI technologies are increasingly being integrated into the OR to provide real-time assistance to surgeons, enhancing their capabilities and improving patient safety.
One of the most promising applications of AI in the OR is the use of robotic surgical systems. These systems, equipped with AI algorithms, can assist surgeons in performing complex procedures with greater precision. For example, the da Vinci Surgical System utilizes AI to enhance the surgeon’s dexterity and control during minimally invasive surgeries. Studies have shown that procedures performed with robotic assistance often result in shorter recovery times and reduced postoperative complications.
AI can also enhance intraoperative imaging by providing real-time feedback on surgical progress. For instance, augmented reality (AR) systems powered by AI can overlay critical information onto the surgical field, allowing surgeons to visualize anatomical structures and navigate complex procedures more effectively. A study published in The Journal of Surgical Research highlighted the use of AR in orthopedic surgeries, where surgeons could visualize bone structures in real-time, leading to improved accuracy in implant placement.
Furthermore, AI can assist in monitoring vital signs and other physiological parameters during surgery. By analyzing data from various monitoring devices, AI systems can detect anomalies and alert the surgical team to potential complications. This capability is particularly valuable in high-risk surgeries where rapid intervention is crucial.
In summary, intraoperative AI assistance enhances surgical efficiency by:
- Improving precision through robotic surgical systems.
- Providing real-time imaging and feedback.
- Monitoring patient vitals and detecting complications early.
4. Postoperative Monitoring and Care
The surgical process does not end when the procedure is completed; postoperative care is equally important for ensuring patient safety and recovery. AI technologies are playing a significant role in enhancing postoperative monitoring and care, leading to improved patient outcomes.
One of the key applications of AI in postoperative care is the use of predictive analytics to identify patients at risk of complications. By analyzing data from EHRs and monitoring devices, AI algorithms can identify patterns that may indicate potential issues, such as infections or readmissions. For example, a study published in The New England Journal of Medicine demonstrated that an AI model could predict postoperative complications with high accuracy, allowing healthcare providers to intervene early and prevent adverse outcomes.
AI can also facilitate remote monitoring of patients after surgery. Wearable devices equipped with AI algorithms can track vital signs and other health metrics, providing real-time data to healthcare providers. This capability allows for timely interventions and reduces the need for patients to return to the hospital for routine check-ups. A pilot study conducted by a leading healthcare institution found that patients who were monitored remotely after surgery experienced fewer complications and shorter recovery times compared to those who received traditional follow-up care.
Moreover, AI can enhance patient engagement in their recovery process. Chatbots and virtual health assistants powered by AI can provide patients with personalized information about their recovery, answer questions, and remind them of medication schedules. This level of engagement can lead to better adherence to postoperative care plans and improved patient satisfaction.
In summary, AI-driven postoperative monitoring enhances surgical efficiency by:
- Predicting complications and enabling early intervention.
- Facilitating remote monitoring and reducing hospital visits.
- Enhancing patient engagement and adherence to care plans.
5. Challenges and Future Directions of AI in Surgery
While the integration of AI in surgical settings offers numerous benefits, it also presents several challenges that must be addressed to fully realize its potential. Understanding these challenges is crucial for healthcare providers, policymakers, and technology developers.
One of the primary challenges is the need for high-quality data to train AI algorithms. AI systems rely on large datasets to learn and make accurate predictions. However, many hospitals may lack comprehensive and standardized data, which can hinder the development of effective AI models. Ensuring data quality and interoperability across different healthcare systems is essential for the successful implementation of AI in surgery.
Another challenge is the need for regulatory approval and validation of AI technologies. The healthcare industry is highly regulated, and any new technology must undergo rigorous testing to ensure its safety and efficacy. This process can be time-consuming and may delay the adoption of innovative AI solutions in surgical settings.
Additionally, there are concerns about the ethical implications of using AI in surgery. Issues such as data privacy, algorithmic bias, and the potential for over-reliance on technology must be carefully considered. Healthcare providers must ensure that AI is used as a tool to augment human decision-making rather than replace it.
Looking ahead, the future of AI in surgery is promising. As technology continues to advance, we can expect to see more sophisticated AI applications that enhance surgical efficiency. For instance, the development of AI-driven surgical simulators could provide surgeons with realistic training experiences, improving their skills and confidence before performing actual procedures.
In summary, the challenges and future directions of AI in surgery include:
- Ensuring high-quality data for training AI algorithms.
- Navigating regulatory approval processes.
- Addressing ethical concerns related to data privacy and algorithmic bias.
- Exploring innovative applications such as AI-driven surgical simulators.
Conclusion
The integration of AI into hospital operating rooms represents a significant advancement in surgical efficiency and patient care. From preoperative planning to intraoperative assistance and postoperative monitoring, AI technologies are transforming the surgical landscape. By leveraging data analytics, predictive modeling, and real-time feedback, AI enhances the capabilities of surgeons, improves patient outcomes, and optimizes hospital resources.
However, the successful implementation of AI in surgery requires addressing challenges related to data quality, regulatory approval, and ethical considerations. As the healthcare industry continues to evolve, embracing AI technologies will be essential for enhancing surgical efficiency and ensuring the highest standards of patient care.
In conclusion, the role of AI in hospital operating rooms is not just a trend; it is a transformative force that has the potential to redefine surgical practices and improve the overall healthcare experience for patients and providers alike.