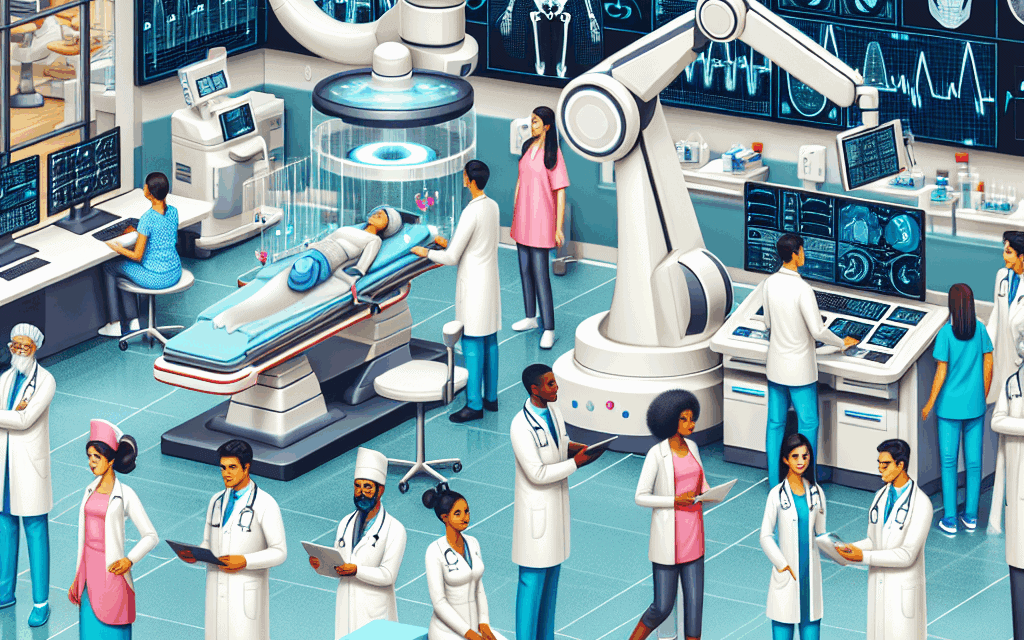
Enhancing Patient Care Through Technological Innovations
In the rapidly evolving landscape of healthcare, technological innovations are playing a pivotal role in enhancing patient care. From telemedicine to artificial intelligence, these advancements are not only improving the efficiency of healthcare delivery but also significantly enhancing patient outcomes. This article explores five key areas where technology is transforming patient care: Telemedicine, Electronic Health Records (EHRs), Artificial Intelligence (AI) in diagnostics, Wearable Health Technology, and Patient Engagement Tools. Each section delves into the specifics of how these innovations are reshaping the healthcare experience for patients and providers alike.
Telemedicine: Bridging the Gap in Healthcare Access
Telemedicine has emerged as a revolutionary approach to healthcare delivery, particularly highlighted during the COVID-19 pandemic. It allows patients to consult healthcare providers remotely, eliminating geographical barriers and reducing the need for in-person visits.
One of the most significant advantages of telemedicine is its ability to increase access to care. Patients in rural or underserved areas can connect with specialists without the need for extensive travel. According to a report by the American Hospital Association, telehealth visits increased by 154% in March 2020 compared to the previous year, showcasing its rapid adoption during a critical time.
- Convenience and Flexibility: Telemedicine offers patients the convenience of scheduling appointments that fit their lifestyles. This flexibility can lead to higher patient satisfaction and adherence to treatment plans.
- Cost-Effectiveness: By reducing the need for physical office space and associated overhead costs, telemedicine can lower healthcare costs for both providers and patients. A study published in the Journal of Medical Internet Research found that telehealth can save patients an average of $100 per visit.
- Continuity of Care: Telemedicine facilitates ongoing communication between patients and providers, ensuring that care is continuous and comprehensive. This is particularly beneficial for chronic disease management, where regular check-ins are crucial.
However, telemedicine is not without its challenges. Issues such as technology access, digital literacy, and reimbursement policies can hinder its effectiveness. Nevertheless, as technology continues to advance and more healthcare systems adopt telehealth solutions, it is poised to become a staple in patient care.
Electronic Health Records (EHRs): Streamlining Patient Information
Electronic Health Records (EHRs) have transformed the way patient information is stored, accessed, and shared among healthcare providers. EHRs provide a digital version of a patient’s paper chart, making it easier for providers to track patient history, medications, and treatment plans.
The implementation of EHRs has led to significant improvements in patient care. For instance, a study published in the New England Journal of Medicine found that EHRs can reduce medication errors by up to 50%. This is largely due to features such as computerized physician order entry (CPOE), which helps prevent adverse drug interactions.
- Improved Coordination of Care: EHRs enable seamless sharing of patient information among different healthcare providers. This is particularly important for patients with multiple specialists, as it ensures that all providers have access to the same information, reducing the risk of miscommunication.
- Enhanced Patient Safety: EHRs come equipped with alerts and reminders that can notify providers of potential issues, such as allergies or contraindications. This proactive approach to patient safety can significantly reduce the likelihood of medical errors.
- Data Analytics and Population Health Management: EHRs allow for the aggregation of patient data, which can be analyzed to identify trends and improve population health outcomes. For example, healthcare organizations can track vaccination rates or monitor chronic disease management across different demographics.
Despite their benefits, EHRs also face criticism, particularly regarding usability and the burden they place on healthcare providers. Many clinicians report that EHR systems can be cumbersome and time-consuming, detracting from patient interaction. As technology evolves, however, there is hope for more user-friendly systems that enhance rather than hinder patient care.
Artificial Intelligence (AI) in Diagnostics: Revolutionizing Decision-Making
Artificial Intelligence (AI) is making significant strides in the field of diagnostics, offering healthcare providers powerful tools to enhance decision-making and improve patient outcomes. AI algorithms can analyze vast amounts of data quickly and accurately, identifying patterns that may be missed by human clinicians.
One of the most promising applications of AI in healthcare is in imaging diagnostics. For example, AI systems have been developed to analyze radiology images for signs of conditions such as cancer. A study published in the journal Nature found that an AI algorithm outperformed human radiologists in detecting breast cancer in mammograms, achieving a reduction in false positives and false negatives.
- Early Detection of Diseases: AI can assist in the early detection of diseases, which is crucial for conditions like cancer where early intervention can significantly improve survival rates. By analyzing patient data and imaging, AI can flag potential issues for further investigation.
- Personalized Treatment Plans: AI can analyze a patient’s genetic information and medical history to recommend personalized treatment plans. This approach is particularly beneficial in oncology, where treatments can be tailored to the specific characteristics of a patient’s tumor.
- Operational Efficiency: AI can streamline administrative tasks, such as scheduling and billing, allowing healthcare providers to focus more on patient care. By automating routine tasks, AI can help reduce burnout among healthcare professionals.
While the potential of AI in diagnostics is immense, ethical considerations and the need for regulatory oversight remain critical. Ensuring that AI systems are transparent, unbiased, and secure is essential for their successful integration into healthcare.
Wearable Health Technology: Empowering Patients
Wearable health technology has gained popularity in recent years, providing patients with tools to monitor their health in real-time. Devices such as smartwatches and fitness trackers can track vital signs, physical activity, and even sleep patterns, empowering patients to take charge of their health.
The integration of wearable technology into patient care has several benefits. For instance, a study published in the Journal of the American Medical Association found that patients with heart conditions who used wearable devices to monitor their heart rate and rhythm experienced fewer hospitalizations and improved health outcomes.
- Real-Time Health Monitoring: Wearable devices allow for continuous monitoring of health metrics, enabling early detection of potential health issues. For example, smartwatches can alert users to irregular heartbeats, prompting timely medical intervention.
- Encouraging Healthy Behaviors: Many wearable devices come with features that promote physical activity and healthy habits. By setting goals and tracking progress, patients are more likely to engage in regular exercise and maintain a healthy lifestyle.
- Data Sharing with Healthcare Providers: Wearable devices can sync data with EHRs, allowing healthcare providers to access real-time information about their patients’ health. This data can inform treatment decisions and enhance patient-provider communication.
Despite their advantages, wearable health technology also faces challenges, including data privacy concerns and the need for patient education on how to use these devices effectively. As technology continues to advance, addressing these issues will be crucial for maximizing the benefits of wearable health technology.
Patient Engagement Tools: Fostering Active Participation
Patient engagement tools are designed to foster active participation in healthcare, empowering patients to take an active role in their health management. These tools include patient portals, mobile health apps, and educational resources that facilitate communication between patients and providers.
Research has shown that engaged patients are more likely to adhere to treatment plans and experience better health outcomes. A study published in Health Affairs found that patients who used patient portals were more likely to manage their chronic conditions effectively, leading to reduced hospitalizations and emergency room visits.
- Access to Health Information: Patient engagement tools provide patients with easy access to their health information, including lab results, medication lists, and appointment schedules. This transparency fosters a sense of ownership over one’s health.
- Enhanced Communication: Tools such as secure messaging allow patients to communicate with their healthcare providers easily. This can lead to quicker responses to questions and concerns, improving the overall patient experience.
- Educational Resources: Many patient engagement tools offer educational materials that help patients understand their conditions and treatment options. This knowledge empowers patients to make informed decisions about their health.
While patient engagement tools have the potential to enhance care, challenges such as digital literacy and access to technology must be addressed. Ensuring that all patients can benefit from these innovations is essential for equitable healthcare delivery.
Conclusion
The integration of technological innovations in healthcare is transforming patient care in profound ways. From telemedicine and EHRs to AI diagnostics, wearable technology, and patient engagement tools, these advancements are enhancing access, improving safety, and empowering patients to take charge of their health.
As healthcare continues to evolve, it is crucial for providers, policymakers, and technology developers to work collaboratively to address the challenges associated with these innovations. By doing so, we can ensure that the benefits of technology are realized by all patients, ultimately leading to a healthier society.
In summary, the future of patient care is bright, driven by technological advancements that promise to enhance the quality of care and improve health outcomes. Embracing these innovations will be key to navigating the complexities of modern healthcare and ensuring that patients receive the best possible care.