Enhancing Healthcare Access for Underserved Communities
Access to healthcare is a fundamental human right, yet millions of individuals in underserved communities face significant barriers to obtaining the medical care they need. These barriers can stem from a variety of factors, including socioeconomic status, geographic location, cultural differences, and systemic inequities. This article explores the multifaceted issue of healthcare access for underserved communities, examining the challenges they face and proposing actionable solutions to enhance access. We will delve into five key areas: the impact of socioeconomic factors, the role of telehealth, community health initiatives, policy reforms, and the importance of cultural competence in healthcare delivery.
The Impact of Socioeconomic Factors
Socioeconomic status is one of the most significant determinants of health. Individuals from low-income backgrounds often experience a range of barriers that limit their access to healthcare services. These barriers can include financial constraints, lack of transportation, and inadequate health insurance coverage.
According to the U.S. Census Bureau, approximately 10.5% of Americans live in poverty, and this figure is even higher in certain communities, particularly among racial and ethnic minorities. The consequences of poverty on health are profound:
- Financial Constraints: Many individuals in underserved communities cannot afford out-of-pocket expenses for medical care, leading to delayed treatment or avoidance of healthcare altogether.
- Lack of Transportation: Geographic isolation can make it difficult for individuals to reach healthcare facilities, particularly in rural areas where public transportation options are limited.
- Inadequate Health Insurance: Many low-income individuals are either uninsured or underinsured, which restricts their access to necessary medical services.
Case studies illustrate the impact of these socioeconomic factors. For instance, a study conducted in rural Appalachia found that residents faced significant barriers to accessing healthcare due to a lack of nearby facilities and transportation options. As a result, many individuals delayed seeking care until their conditions worsened, leading to higher rates of chronic diseases and preventable hospitalizations.
Addressing these socioeconomic barriers requires a multifaceted approach. Community-based organizations can play a crucial role in providing resources and support to underserved populations. For example, initiatives that offer transportation services to medical appointments or financial assistance for medical expenses can significantly improve access to care.
The Role of Telehealth
Telehealth has emerged as a powerful tool for enhancing healthcare access, particularly in underserved communities. The COVID-19 pandemic accelerated the adoption of telehealth services, demonstrating their potential to bridge gaps in care.
Telehealth offers several advantages:
- Increased Accessibility: Patients can access healthcare services from the comfort of their homes, eliminating transportation barriers.
- Cost-Effectiveness: Telehealth visits are often less expensive than in-person appointments, making healthcare more affordable for low-income individuals.
- Expanded Reach: Telehealth can connect patients with specialists who may not be available in their local area, improving the quality of care.
Research supports the effectiveness of telehealth in improving healthcare access. A study published in the Journal of the American Medical Association found that telehealth services significantly increased the likelihood of patients receiving timely care for chronic conditions such as diabetes and hypertension. Additionally, a survey conducted by the American Medical Association revealed that 60% of patients reported being satisfied with their telehealth experiences, citing convenience and reduced travel time as key benefits.
However, challenges remain. Not all individuals have access to the necessary technology or internet connectivity to utilize telehealth services. To address this issue, community organizations and healthcare providers can work together to provide resources such as internet access points and devices for low-income individuals. Furthermore, training programs can help patients navigate telehealth platforms effectively.
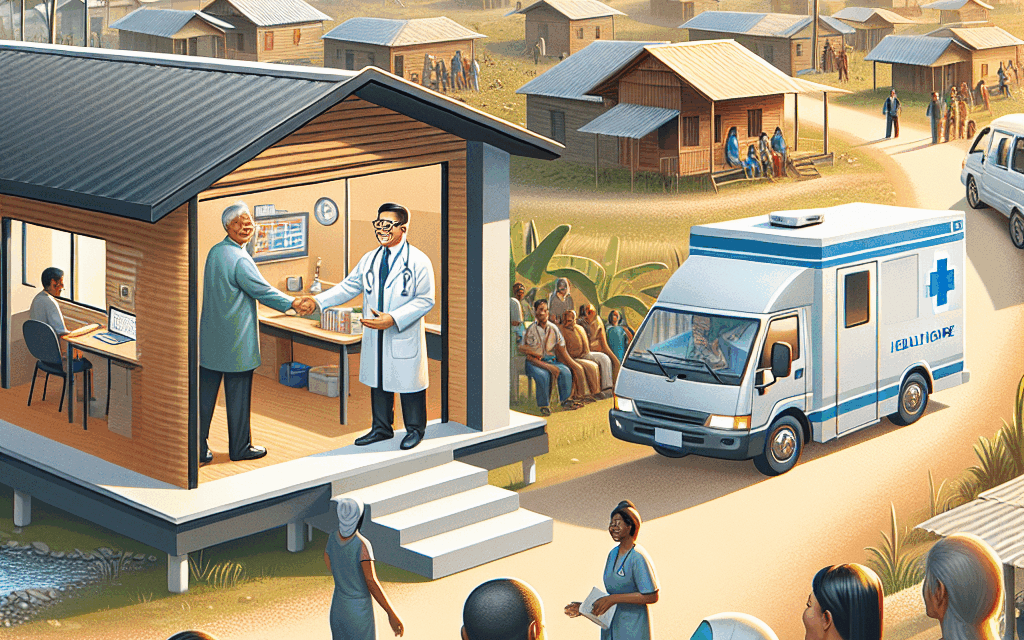
Community Health Initiatives
Community health initiatives are essential for addressing the unique needs of underserved populations. These initiatives often focus on preventive care, education, and outreach, aiming to empower individuals to take charge of their health.
Successful community health initiatives often incorporate the following elements:
- Health Education: Providing information about preventive care, nutrition, and chronic disease management can empower individuals to make informed health choices.
- Outreach Programs: Mobile clinics and community health fairs can bring healthcare services directly to underserved populations, reducing barriers to access.
- Partnerships with Local Organizations: Collaborating with schools, churches, and community centers can enhance outreach efforts and build trust within the community.
One notable example of a successful community health initiative is the “Healthy Corner Store” program, which aims to increase access to fresh fruits and vegetables in food deserts. By partnering with local corner stores, this initiative provides training and resources to store owners, enabling them to offer healthier food options. As a result, communities experience improved nutrition and reduced rates of diet-related diseases.
Another example is the use of community health workers (CHWs) who serve as liaisons between healthcare providers and underserved populations. CHWs can provide education, support, and navigation assistance, helping individuals access the care they need. Research has shown that CHWs can improve health outcomes and reduce healthcare costs by addressing social determinants of health.
Policy Reforms
Policy reforms play a critical role in enhancing healthcare access for underserved communities. Policymakers must prioritize initiatives that address systemic inequities and ensure that all individuals have access to quality healthcare services.
Key areas for policy reform include:
- Expanding Medicaid: Expanding Medicaid eligibility can provide millions of low-income individuals with access to healthcare services. States that have expanded Medicaid have seen significant reductions in uninsured rates and improved health outcomes.
- Investing in Community Health Centers: Community health centers provide comprehensive care to underserved populations. Increased funding for these centers can enhance their capacity to serve more patients and offer a wider range of services.
- Addressing Social Determinants of Health: Policymakers should prioritize initiatives that address the social determinants of health, such as housing, education, and employment, which significantly impact health outcomes.
Case studies from states that have implemented successful policy reforms provide valuable insights. For example, California’s expansion of Medi-Cal (the state’s Medicaid program) has resulted in increased access to care for low-income individuals, leading to improved health outcomes and reduced emergency room visits. Similarly, Massachusetts’ investment in community health centers has helped reduce health disparities among racial and ethnic minorities.
Advocacy efforts are also crucial in driving policy change. Grassroots organizations and community leaders can mobilize support for healthcare reforms, ensuring that the voices of underserved populations are heard in the policymaking process.
The Importance of Cultural Competence in Healthcare Delivery
Cultural competence is essential for providing effective healthcare to diverse populations. Healthcare providers must understand and respect the cultural beliefs, values, and practices of the communities they serve to deliver high-quality care.
Key components of cultural competence include:
- Awareness of Cultural Differences: Healthcare providers should be aware of the cultural backgrounds of their patients and how these backgrounds may influence health beliefs and behaviors.
- Effective Communication: Providers should use clear and respectful communication, taking into account language barriers and health literacy levels.
- Building Trust: Establishing trust with patients is crucial for encouraging them to seek care and adhere to treatment plans.
Research has shown that culturally competent care can lead to improved health outcomes. A study published in the American Journal of Public Health found that patients who received care from culturally competent providers were more likely to adhere to treatment plans and report higher satisfaction with their care.
Training programs focused on cultural competence can help healthcare providers develop the skills necessary to serve diverse populations effectively. For example, the National Center for Cultural Competence offers resources and training for healthcare organizations to enhance their cultural competence.
Additionally, involving community members in the design and delivery of healthcare services can ensure that care is tailored to the specific needs of the population. Community advisory boards can provide valuable insights and feedback, helping healthcare organizations better understand the cultural context of the communities they serve.
Conclusion
Enhancing healthcare access for underserved communities is a complex challenge that requires a multifaceted approach. By addressing socioeconomic barriers, leveraging telehealth, implementing community health initiatives, advocating for policy reforms, and promoting cultural competence, we can work towards a more equitable healthcare system.
Key takeaways from this article include:
- The significant impact of socioeconomic factors on healthcare access and the need for targeted interventions.
- The potential of telehealth to improve access, particularly in rural and underserved areas.
- The importance of community health initiatives in empowering individuals and addressing health disparities.
- The critical role of policy reforms in ensuring equitable access to healthcare services.
- The necessity of cultural competence in healthcare delivery to meet the diverse needs of patients.
By working collaboratively across sectors and engaging with underserved communities, we can create a healthcare system that is accessible, equitable, and responsive to the needs of all individuals. The journey towards enhancing healthcare access is ongoing, but with commitment and innovation, we can make significant strides in improving health outcomes for underserved populations.