Effortless and Relaxed: The Next Generation of Surgical Support
The landscape of surgical support is undergoing a transformative shift, driven by advancements in technology, a focus on patient-centered care, and the need for efficiency in the operating room. As healthcare systems strive to improve outcomes while reducing costs, the next generation of surgical support is emerging, characterized by effortless and relaxed environments that enhance both surgical performance and patient experience. This article delves into five key subtopics that illustrate this evolution: the role of technology in surgical support, the importance of team dynamics, innovations in surgical instruments, the impact of patient-centered design, and the future of surgical training and education.
The Role of Technology in Surgical Support
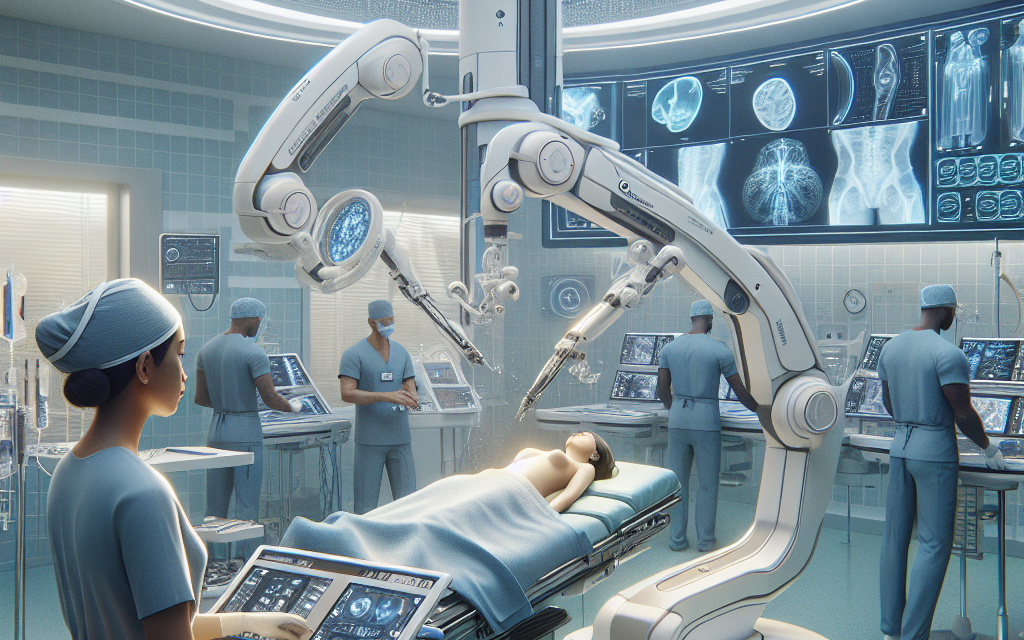
Technology has become an integral part of modern surgical support, enhancing precision, efficiency, and safety in the operating room. From robotic-assisted surgeries to advanced imaging systems, technology is reshaping how surgeries are performed and supported.
One of the most significant advancements is the introduction of robotic surgical systems. These systems allow surgeons to perform minimally invasive procedures with enhanced dexterity and control. For instance, the da Vinci Surgical System has revolutionized urological, gynecological, and general surgeries by providing surgeons with a 3D view of the surgical site and the ability to manipulate instruments with precision. According to a study published in the Journal of Robotic Surgery, robotic-assisted surgeries have been associated with reduced blood loss, shorter hospital stays, and quicker recovery times compared to traditional open surgeries.
In addition to robotic systems, imaging technologies such as augmented reality (AR) and virtual reality (VR) are becoming increasingly prevalent in surgical support. These technologies provide surgeons with real-time data and visualizations that enhance their understanding of complex anatomical structures. For example, AR can overlay critical information onto a surgeon’s field of view, allowing for more informed decision-making during procedures. A study conducted by the University of California, San Francisco, found that AR-assisted surgeries improved accuracy and reduced the time taken to complete complex procedures.
Moreover, artificial intelligence (AI) is playing a pivotal role in surgical support by analyzing vast amounts of data to assist in preoperative planning and intraoperative decision-making. AI algorithms can predict potential complications based on patient data, enabling surgical teams to prepare more effectively. A report from the American College of Surgeons highlighted that AI-driven predictive analytics could reduce surgical complications by up to 30%.
- Robotic surgical systems enhance precision and control.
- Augmented and virtual reality improve understanding of anatomy.
- Artificial intelligence aids in preoperative planning and decision-making.
- Data analytics can predict complications and improve outcomes.
- Integration of technology streamlines surgical workflows.
As technology continues to evolve, the integration of these tools into surgical support will lead to more effortless and relaxed surgical environments, ultimately benefiting both patients and healthcare providers.
The Importance of Team Dynamics
Effective surgical support is not solely reliant on technology; it also hinges on the dynamics of the surgical team. A well-coordinated team can significantly enhance the efficiency and safety of surgical procedures. The importance of communication, collaboration, and mutual respect among team members cannot be overstated.
Research has shown that effective communication is a cornerstone of successful surgical outcomes. A study published in the Journal of the American College of Surgeons found that surgical teams that engaged in structured communication practices, such as preoperative briefings and postoperative debriefings, experienced fewer complications and improved patient satisfaction. These practices foster an environment where team members feel comfortable voicing concerns and sharing insights, ultimately leading to better decision-making during surgeries.
Collaboration among team members is equally crucial. The surgical team typically consists of surgeons, anesthesiologists, nurses, and surgical technologists, each with distinct roles and responsibilities. A collaborative approach ensures that all team members are aligned in their goals and can support one another effectively. For instance, during a complex procedure, a surgical nurse may anticipate the surgeon’s needs by preparing instruments in advance, allowing the surgeon to focus on the task at hand without unnecessary interruptions.
Moreover, mutual respect among team members fosters a positive work environment, which can reduce stress and enhance performance. A study conducted by the Institute for Healthcare Improvement found that surgical teams that practiced mutual respect and support reported higher levels of job satisfaction and lower rates of burnout. This is particularly important in high-stress environments like the operating room, where the stakes are high, and the pressure is intense.
- Effective communication enhances surgical outcomes.
- Structured communication practices reduce complications.
- Collaboration among team members improves efficiency.
- Mutual respect fosters a positive work environment.
- Team dynamics influence job satisfaction and burnout rates.
As the next generation of surgical support evolves, prioritizing team dynamics will be essential in creating an effortless and relaxed atmosphere in the operating room, ultimately leading to better patient care.
Innovations in Surgical Instruments
The development of innovative surgical instruments is a critical component of the next generation of surgical support. These advancements not only enhance the precision and safety of surgical procedures but also contribute to a more relaxed environment for both surgeons and patients.
One notable innovation is the emergence of smart surgical instruments equipped with sensors and connectivity features. These instruments can provide real-time feedback to surgeons, allowing them to make informed decisions during procedures. For example, smart scalpels can measure tissue properties and provide data on blood flow, helping surgeons assess the best approach for incisions. A study published in the journal Surgical Endoscopy demonstrated that the use of smart instruments reduced the risk of complications by 25% in laparoscopic surgeries.
Another significant advancement is the development of single-use surgical instruments. Traditionally, reusable instruments required extensive cleaning and sterilization processes, which could lead to delays in surgical schedules. Single-use instruments eliminate this concern, allowing for quicker turnaround times between procedures. A report from the Association of periOperative Registered Nurses (AORN) indicated that the adoption of single-use instruments could reduce surgical delays by up to 40%, contributing to a more efficient operating room environment.
Furthermore, advancements in minimally invasive surgical techniques have led to the creation of specialized instruments designed for specific procedures. For instance, laparoscopic instruments have evolved to include articulating tips and advanced graspers that enhance maneuverability within the body. These innovations not only improve surgical outcomes but also reduce patient recovery times, leading to a more relaxed experience for patients post-surgery.
- Smart surgical instruments provide real-time feedback.
- Single-use instruments reduce delays in surgical schedules.
- Minimally invasive techniques enhance precision and recovery.
- Specialized instruments improve maneuverability during procedures.
- Innovations contribute to a safer and more efficient operating room.
As surgical instruments continue to evolve, their role in creating an effortless and relaxed surgical support environment will become increasingly significant, ultimately benefiting both healthcare providers and patients.
The Impact of Patient-Centered Design
In recent years, there has been a growing recognition of the importance of patient-centered design in healthcare settings, including surgical environments. Creating spaces that prioritize patient comfort and well-being can significantly enhance the overall surgical experience.
One key aspect of patient-centered design is the physical layout of the operating room and recovery areas. Research has shown that well-designed spaces can reduce patient anxiety and improve satisfaction. For instance, incorporating natural light, calming colors, and comfortable furnishings can create a more inviting atmosphere. A study published in the Journal of Environmental Psychology found that patients who underwent surgery in environments designed with patient comfort in mind reported lower levels of anxiety and pain compared to those in traditional settings.
Moreover, patient-centered design extends beyond the physical environment to include the surgical process itself. Engaging patients in their care and providing them with information about their procedures can alleviate anxiety and foster a sense of control. Preoperative education programs that explain what to expect during surgery and recovery have been shown to improve patient satisfaction and reduce postoperative complications. A systematic review published in the British Journal of Surgery found that patients who received preoperative education experienced shorter hospital stays and lower rates of anxiety.
Additionally, incorporating technology into patient-centered design can enhance the surgical experience. For example, virtual reality (VR) can be used to provide patients with immersive experiences that prepare them for surgery. A study conducted by the University of Washington found that patients who used VR before surgery reported lower levels of anxiety and pain during the procedure.
- Patient-centered design prioritizes comfort and well-being.
- Physical layout impacts patient anxiety and satisfaction.
- Preoperative education improves patient outcomes.
- Engaging patients fosters a sense of control.
- Technology enhances the surgical experience through immersive tools.
As healthcare continues to evolve, embracing patient-centered design will be essential in creating effortless and relaxed surgical support environments that prioritize the needs and experiences of patients.
The Future of Surgical Training and Education
The future of surgical training and education is poised for significant transformation as new technologies and methodologies emerge. Preparing the next generation of surgeons requires innovative approaches that emphasize hands-on experience, collaboration, and adaptability.
One of the most promising developments in surgical training is the use of simulation-based education. High-fidelity simulators allow trainees to practice surgical techniques in a risk-free environment, enabling them to develop their skills without jeopardizing patient safety. A study published in the Annals of Surgery found that surgical residents who trained on simulators demonstrated improved technical skills and reduced error rates during actual surgeries.
Moreover, the integration of virtual reality (VR) and augmented reality (AR) into surgical training is gaining traction. These technologies provide immersive experiences that allow trainees to visualize complex procedures and practice in a realistic setting. For instance, VR platforms can simulate various surgical scenarios, enabling trainees to refine their decision-making skills and enhance their understanding of anatomy. A study conducted by the University of Toronto found that medical students who trained using VR reported higher confidence levels and better retention of surgical techniques.
Collaboration and mentorship are also critical components of effective surgical training. Establishing mentorship programs that connect experienced surgeons with trainees can foster a culture of learning and support. A study published in the Journal of Surgical Education highlighted that mentorship programs improved trainee satisfaction and confidence, ultimately leading to better surgical outcomes.
- Simulation-based education enhances technical skills.
- Virtual and augmented reality provide immersive training experiences.
- Collaboration and mentorship foster a culture of learning.
- Innovative training methods improve confidence and retention.
- Adaptability is essential in preparing future surgeons.
As surgical training continues to evolve, embracing innovative methodologies will be crucial in preparing the next generation of surgeons for the challenges of modern healthcare, ultimately contributing to effortless and relaxed surgical support environments.
Conclusion
The next generation of surgical support is characterized by a focus on creating effortless and relaxed environments that enhance both surgical performance and patient experience. Through advancements in technology, the importance of team dynamics, innovations in surgical instruments, patient-centered design, and the evolution of surgical training, the landscape of surgical support is transforming.
As we move forward, it is essential for healthcare providers to embrace these changes and prioritize the integration of technology, effective communication, and patient-centered approaches. By doing so, we can create surgical environments that not only improve outcomes but also foster a sense of comfort and well-being for patients and surgical teams alike.
In summary, the future of surgical support holds great promise, with the potential to revolutionize how surgeries are performed and experienced. By focusing on effortless and relaxed environments, we can ensure that both patients and healthcare providers thrive in the evolving landscape of surgical care.