Decline in Private Practice Physicians: Insights from the AMA
The landscape of healthcare in the United States has undergone significant changes over the past few decades, particularly concerning the role of private practice physicians. The American Medical Association (AMA) has been at the forefront of analyzing these trends, providing insights into the factors contributing to the decline of private practice. This article delves into the multifaceted reasons behind this trend, exploring the implications for healthcare delivery, physician satisfaction, and patient care.
Understanding the Decline of Private Practice
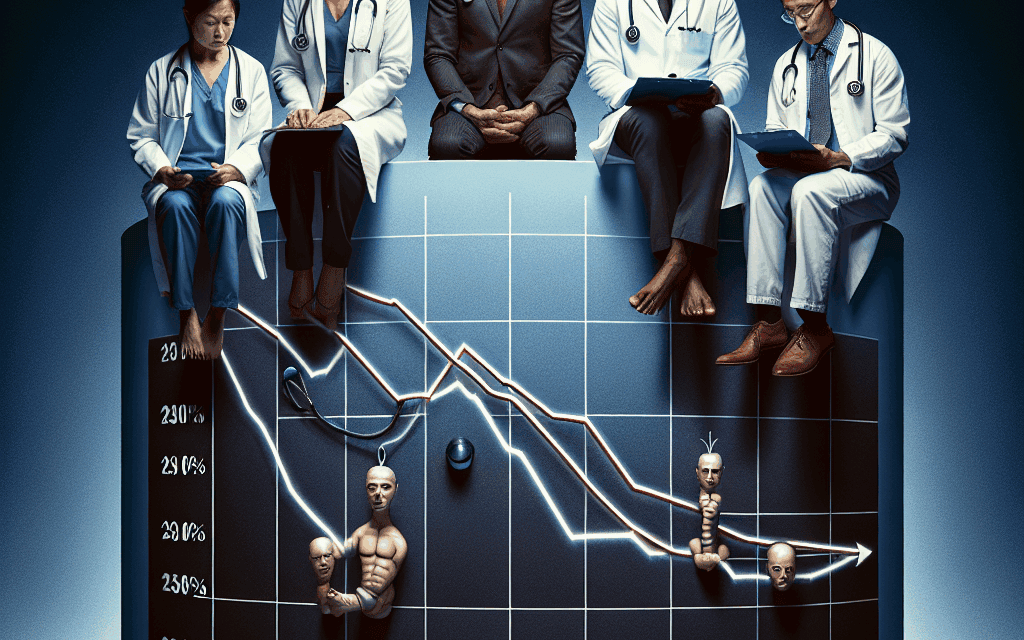
The decline of private practice physicians is a complex issue influenced by various factors, including economic pressures, regulatory changes, and shifts in patient expectations. According to the AMA, the percentage of physicians in private practice has decreased significantly over the years, with many opting for employment in hospitals or larger healthcare systems. This section will explore the key reasons behind this trend.
Economic Pressures and Financial Viability
One of the most significant factors contributing to the decline of private practice is the economic pressures faced by physicians. The rising costs of running a private practice, coupled with decreasing reimbursements from insurance companies, have made it increasingly difficult for physicians to maintain their independence.
- High Overhead Costs: Private practices often face high overhead costs, including rent, utilities, staff salaries, and malpractice insurance. According to a 2021 AMA report, the average overhead for a private practice can range from 60% to 70% of revenue, leaving physicians with limited income.
- Decreasing Reimbursements: The shift towards value-based care has led to changes in reimbursement models. Many private practices struggle to adapt to these new models, which often favor larger healthcare systems that can absorb the financial risks associated with patient care.
- Patient Volume Challenges: With the rise of urgent care centers and telemedicine, private practices face increased competition for patients. This competition can lead to reduced patient volumes, further straining the financial viability of private practices.
As a result of these economic pressures, many physicians find it more appealing to join larger healthcare organizations that can provide financial stability and administrative support. This shift not only impacts the physicians but also alters the dynamics of patient care, as larger systems often prioritize efficiency over personalized care.
Regulatory Challenges and Administrative Burdens
The regulatory environment surrounding healthcare has become increasingly complex, placing additional burdens on private practice physicians. The administrative tasks required to comply with regulations can be overwhelming, detracting from the time physicians can spend with patients.
- Complex Billing and Coding Requirements: The transition to electronic health records (EHR) and the implementation of the Affordable Care Act (ACA) have introduced complex billing and coding requirements. Many private practices lack the resources to manage these complexities effectively.
- Quality Reporting Mandates: Physicians are now required to participate in various quality reporting programs, which can be time-consuming and require additional staff to manage. This can be particularly challenging for small practices with limited resources.
- Compliance with HIPAA and Other Regulations: Ensuring compliance with the Health Insurance Portability and Accountability Act (HIPAA) and other regulations requires significant administrative effort. For many private practices, this translates into hiring additional staff or outsourcing these tasks, further increasing overhead costs.
These regulatory challenges can lead to burnout among physicians, who may feel overwhelmed by the administrative demands of running a practice. Consequently, many choose to leave private practice in favor of employment in larger healthcare systems that can handle these burdens more effectively.
Shifts in Patient Expectations and Healthcare Delivery
As healthcare evolves, so do patient expectations. Today’s patients are more informed and have higher expectations regarding their healthcare experiences. This shift has implications for private practice physicians, who may struggle to meet these demands.
- Demand for Convenience: Patients increasingly seek convenience in their healthcare experiences, favoring options like telemedicine and urgent care centers that offer quick access to care. Private practices may find it challenging to compete with these models, which often prioritize speed and accessibility.
- Desire for Comprehensive Care: Patients are also looking for comprehensive care that addresses their physical, mental, and emotional health. Larger healthcare systems can offer integrated services that private practices may struggle to provide.
- Increased Use of Technology: The rise of health technology, including mobile health apps and wearable devices, has changed how patients engage with their healthcare. Private practices may need to invest in technology to meet patient expectations, which can be financially burdensome.
These shifts in patient expectations can create a disconnect between what private practice physicians can offer and what patients desire. As a result, many physicians may feel compelled to leave private practice to work in environments that can better meet these evolving needs.
Impact of COVID-19 on Private Practice
The COVID-19 pandemic has had a profound impact on the healthcare landscape, exacerbating existing challenges for private practice physicians. The pandemic has led to significant changes in patient behavior and healthcare delivery, further contributing to the decline of private practice.
- Financial Strain: Many private practices experienced a sharp decline in patient visits during the pandemic, leading to significant financial strain. According to a survey by the AMA, nearly 60% of physicians reported a decrease in revenue during the early months of the pandemic.
- Shift to Telehealth: The rapid adoption of telehealth during the pandemic has changed how patients access care. While telehealth has provided opportunities for some private practices, those that were not prepared to offer these services faced challenges in retaining patients.
- Increased Burnout: The pandemic has taken a toll on physician mental health, with many experiencing increased levels of burnout. The stress of managing COVID-19 cases, coupled with the challenges of running a practice during a crisis, has led some physicians to reconsider their career paths.
The long-term effects of the pandemic on private practice are still unfolding, but it is clear that the challenges faced during this time have accelerated trends that were already in motion. Many physicians are now seeking employment in larger healthcare systems that can provide more stability and support.
Future of Private Practice: Opportunities and Challenges
Despite the challenges facing private practice physicians, there are still opportunities for those who wish to maintain their independence. Understanding the evolving healthcare landscape and adapting to new realities will be crucial for the future of private practice.
- Embracing Technology: Private practices that leverage technology effectively can enhance patient engagement and streamline operations. Investing in telehealth capabilities and EHR systems can help practices remain competitive.
- Focus on Niche Markets: Some private practices are finding success by focusing on niche markets or specialized services that cater to specific patient populations. This can help differentiate them from larger healthcare systems.
- Collaboration and Networking: Building networks with other private practices and healthcare providers can create opportunities for collaboration and resource sharing. This can help practices navigate challenges more effectively.
While the decline of private practice poses significant challenges, it also presents opportunities for innovation and adaptation. Physicians who are willing to embrace change and explore new models of care may find ways to thrive in this evolving landscape.
Conclusion
The decline in private practice physicians is a multifaceted issue influenced by economic pressures, regulatory challenges, shifts in patient expectations, and the impact of the COVID-19 pandemic. As the healthcare landscape continues to evolve, private practice physicians must navigate these challenges while seeking opportunities for growth and innovation.
Understanding the factors contributing to this decline is essential for stakeholders in the healthcare system, including policymakers, healthcare organizations, and physicians themselves. By addressing the challenges faced by private practices and exploring new models of care, it may be possible to revitalize this important aspect of the healthcare system.
Ultimately, the future of private practice will depend on the ability of physicians to adapt to changing circumstances while maintaining their commitment to providing high-quality, patient-centered care. The insights from the AMA serve as a valuable resource for understanding these trends and guiding the future of private practice in the United States.