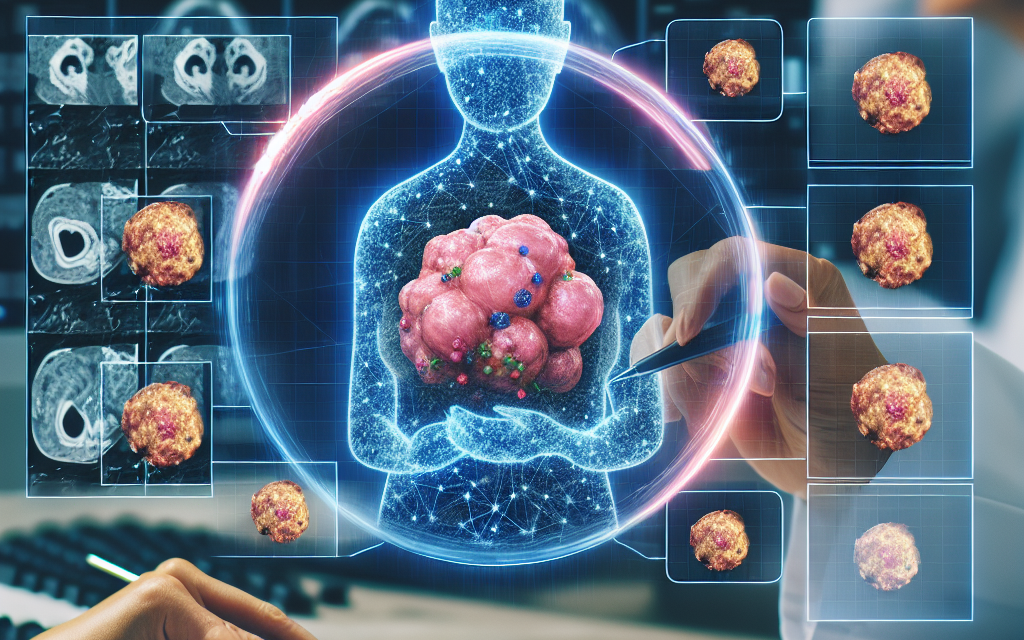
CHOP Unveils AI Model to Improve Tumor Analysis
The Children’s Hospital of Philadelphia (CHOP) has recently made headlines with the unveiling of a groundbreaking artificial intelligence (AI) model designed to enhance tumor analysis. This innovative approach aims to revolutionize the way tumors are diagnosed and treated, providing healthcare professionals with advanced tools to improve patient outcomes. In this article, we will explore the significance of this development, the technology behind it, its implications for pediatric oncology, and the future of AI in healthcare.
Understanding the Need for Advanced Tumor Analysis
Tumor analysis is a critical component of cancer diagnosis and treatment. Accurate identification of tumor types, stages, and genetic mutations can significantly influence treatment decisions and patient prognosis. However, traditional methods of tumor analysis often face limitations, including:
- Human Error: Pathologists may overlook subtle features in tumor samples, leading to misdiagnosis.
- Time Constraints: The increasing volume of cases can overwhelm pathologists, resulting in rushed analyses.
- Variability in Interpretation: Different pathologists may interpret the same sample differently, leading to inconsistencies in diagnosis.
These challenges underscore the need for more reliable and efficient methods of tumor analysis. The introduction of AI technology in this field promises to address these issues by providing tools that can analyze tumor samples with greater accuracy and speed.
The Technology Behind CHOP’s AI Model
The AI model developed by CHOP leverages advanced machine learning algorithms to analyze histopathological images of tumor samples. This technology is built on several key components:
- Deep Learning: The model utilizes deep learning techniques, particularly convolutional neural networks (CNNs), which are adept at recognizing patterns in visual data.
- Large Datasets: The AI was trained on extensive datasets comprising thousands of annotated tumor images, allowing it to learn from a diverse range of cases.
- Real-Time Analysis: The model is designed to provide real-time feedback, enabling pathologists to make quicker and more informed decisions.
One of the standout features of this AI model is its ability to identify not only the type of tumor but also its molecular characteristics. This capability is crucial for personalized medicine, where treatment plans are tailored to the specific genetic makeup of a patient’s tumor.
Implications for Pediatric Oncology
Pediatric oncology presents unique challenges, as tumors in children often differ from those in adults. The AI model developed by CHOP has significant implications for this field:
- Improved Diagnostic Accuracy: The AI model can help reduce misdiagnosis rates, which are particularly concerning in pediatric cases where treatment options may be limited.
- Personalized Treatment Plans: By analyzing the genetic profile of tumors, the AI can assist in developing targeted therapies that are more effective for young patients.
- Enhanced Research Opportunities: The data generated by the AI can contribute to ongoing research efforts, helping to identify new biomarkers and treatment strategies.
For instance, a case study involving a young patient with a rare type of brain tumor demonstrated how the AI model could accurately identify the tumor’s genetic mutations. This information allowed the medical team to select a targeted therapy that significantly improved the patient’s prognosis.
Challenges and Limitations of AI in Tumor Analysis
While the potential benefits of AI in tumor analysis are substantial, there are also challenges and limitations that must be addressed:
- Data Privacy Concerns: The use of patient data for training AI models raises ethical questions regarding privacy and consent.
- Integration with Existing Systems: Implementing AI technology in clinical settings requires seamless integration with existing pathology workflows.
- Need for Validation: AI models must undergo rigorous validation to ensure their accuracy and reliability before widespread adoption.
Moreover, there is a need for ongoing education and training for pathologists to effectively utilize AI tools. As these technologies evolve, healthcare professionals must stay informed about their capabilities and limitations.
The Future of AI in Healthcare
The unveiling of CHOP’s AI model marks a significant step forward in the integration of artificial intelligence in healthcare. The future of AI in this field holds immense promise:
- Broader Applications: Beyond tumor analysis, AI can be applied to various aspects of healthcare, including radiology, genomics, and patient monitoring.
- Collaboration with Clinicians: AI will increasingly serve as a collaborative tool for healthcare professionals, enhancing their decision-making capabilities.
- Continuous Learning: AI models can be designed to learn continuously from new data, improving their accuracy and effectiveness over time.
As we look ahead, it is essential to foster a collaborative environment between AI developers and healthcare professionals to ensure that these technologies are used ethically and effectively. The goal should be to enhance patient care while maintaining the human touch that is so vital in medicine.
Conclusion
The unveiling of CHOP’s AI model for tumor analysis represents a significant advancement in the field of pediatric oncology. By addressing the challenges of traditional tumor analysis methods, this innovative technology has the potential to improve diagnostic accuracy, personalize treatment plans, and enhance research opportunities. However, it is crucial to navigate the challenges associated with data privacy, integration, and validation to ensure the successful implementation of AI in clinical settings.
As we move forward, the collaboration between AI technology and healthcare professionals will be key to unlocking the full potential of these advancements. The future of AI in healthcare is bright, and with continued research and development, we can look forward to a new era of precision medicine that ultimately improves patient outcomes and transforms the landscape of cancer care.