-
Table of Contents
- Challenges and Opportunities in Rural Healthcare Delivery
- 1. Infrastructure and Accessibility
- 1.1 Transportation Barriers
- 1.2 Facility Shortages
- 1.3 Technological Limitations
- 2. Workforce Challenges
- 2.1 Recruitment and Retention
- 2.2 Training and Education
- 2.3 Scope of Practice
- 3. Financial Constraints
- 3.1 Funding Shortages
- 3.2 Insurance Coverage
- 3.3 Cost of Care
- 4. Health Disparities
- 4.1 Chronic Disease Prevalence
- 4.2 Mental Health Services
- 4.3 Health Literacy
- 5. Opportunities for Innovation
Challenges and Opportunities in Rural Healthcare Delivery
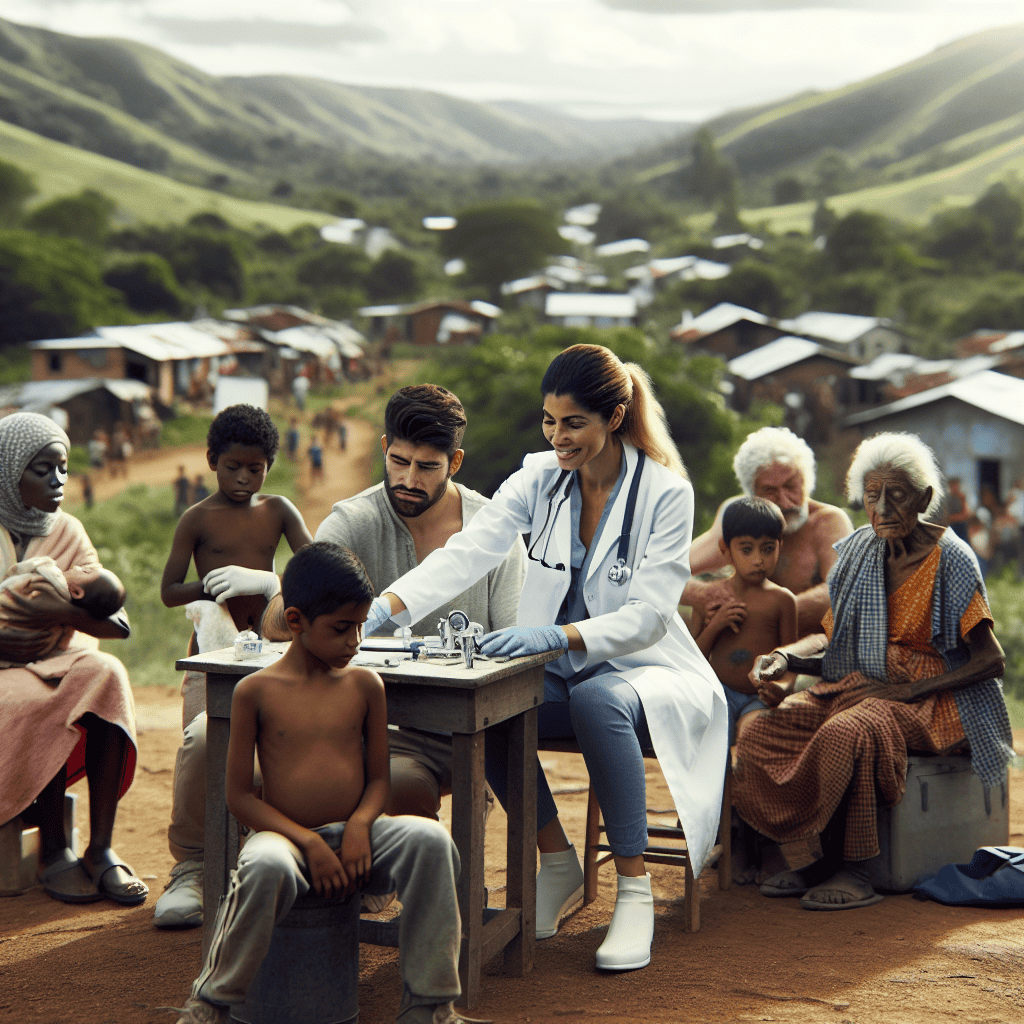
Rural healthcare delivery is a critical component of the global health system, yet it faces unique challenges that can hinder the provision of quality care. At the same time, these challenges present opportunities for innovation and improvement. This article explores the multifaceted landscape of rural healthcare, examining the obstacles and potential solutions that can enhance healthcare delivery in these areas.
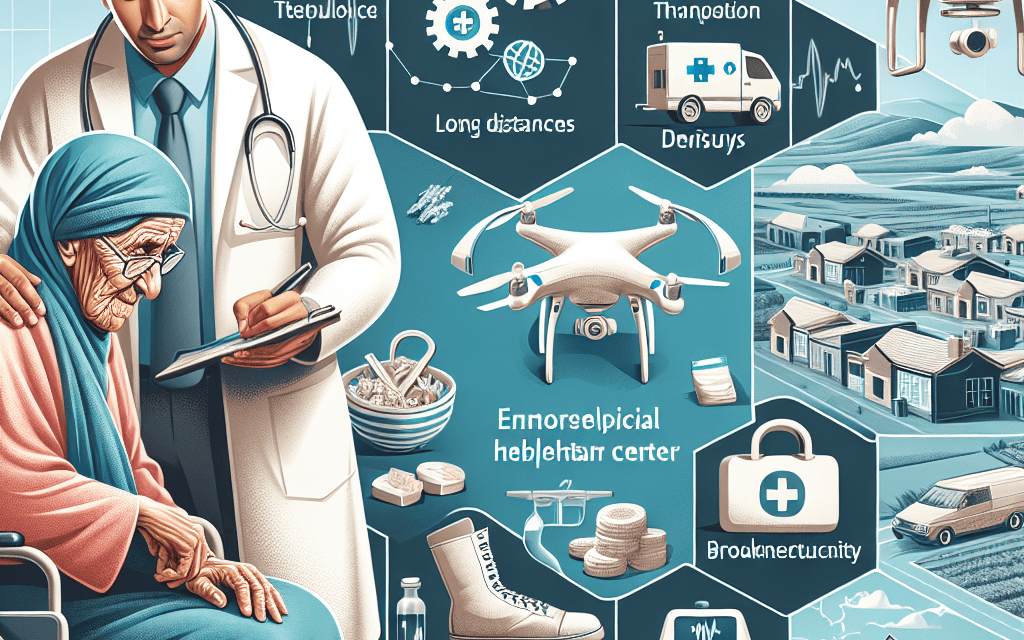
1. Infrastructure and Accessibility
Infrastructure and accessibility are foundational elements of effective healthcare delivery. In rural areas, these elements often present significant challenges that can impede access to necessary medical services.
1.1 Transportation Barriers
One of the most pressing issues in rural healthcare is the lack of reliable transportation. Many rural areas are characterized by vast distances between communities and healthcare facilities, making it difficult for residents to access care. This is particularly problematic for individuals with chronic conditions who require regular medical attention.
For example, a study conducted in rural Appalachia found that transportation was a major barrier to healthcare access, with many residents lacking personal vehicles or public transportation options. This issue is compounded by poor road conditions and inclement weather, which can further hinder travel.
- Limited public transportation options
- Long distances to healthcare facilities
- Poor road conditions
- Weather-related travel disruptions
1.2 Facility Shortages
Rural areas often suffer from a shortage of healthcare facilities, including hospitals, clinics, and specialized care centers. This scarcity can lead to overcrowding and long wait times, reducing the quality of care that patients receive.
In many cases, rural hospitals are small and underfunded, lacking the resources to provide comprehensive services. This can force patients to travel long distances to urban centers for specialized care, further exacerbating accessibility issues.
1.3 Technological Limitations
The digital divide is another significant barrier to healthcare access in rural areas. Many rural communities lack high-speed internet access, which limits the availability of telemedicine services that could otherwise bridge the gap in healthcare delivery.
Telemedicine has the potential to revolutionize rural healthcare by providing remote consultations and monitoring, but without reliable internet infrastructure, its benefits remain out of reach for many rural residents.
2. Workforce Challenges
The healthcare workforce is a critical component of any healthcare system, and rural areas face unique challenges in attracting and retaining qualified professionals.
2.1 Recruitment and Retention
Recruiting healthcare professionals to rural areas is a persistent challenge. Many healthcare workers prefer to work in urban settings where they have access to more resources, professional development opportunities, and personal amenities.
Retention is equally challenging, as rural healthcare workers often face professional isolation, limited career advancement opportunities, and lower salaries compared to their urban counterparts. These factors contribute to high turnover rates and staffing shortages in rural healthcare facilities.
2.2 Training and Education
Access to training and education is another barrier for rural healthcare workers. Continuing education and professional development are essential for maintaining high standards of care, but rural professionals often have limited access to these opportunities.
Programs that offer remote learning and on-site training can help bridge this gap, but they require investment and support from both government and private sectors.
2.3 Scope of Practice
In rural areas, healthcare professionals often need to work outside their traditional scope of practice to meet the needs of their communities. This can lead to increased stress and burnout, as well as potential legal and ethical challenges.
Expanding the scope of practice for certain healthcare roles, such as nurse practitioners and physician assistants, can help alleviate some of these pressures, but it requires careful regulation and oversight.
3. Financial Constraints
Financial constraints are a significant barrier to effective healthcare delivery in rural areas. Limited funding and resources can impact the quality and availability of care.
3.1 Funding Shortages
Rural healthcare facilities often operate on tight budgets, with limited funding from government and private sources. This can lead to understaffing, outdated equipment, and inadequate facilities.
Efforts to increase funding for rural healthcare are essential, but they must be accompanied by strategic planning to ensure that resources are used effectively and efficiently.
3.2 Insurance Coverage
Insurance coverage is another financial challenge for rural residents. Many individuals in rural areas are uninsured or underinsured, which can limit their access to necessary medical services.
Expanding insurance coverage and providing subsidies for low-income individuals can help address this issue, but it requires policy changes and collaboration between government and private insurers.
3.3 Cost of Care
The cost of healthcare can be prohibitive for many rural residents, particularly those with low incomes. High out-of-pocket expenses can deter individuals from seeking care, leading to worse health outcomes.
Efforts to reduce the cost of care, such as implementing sliding scale fees and offering financial assistance programs, can help make healthcare more accessible to rural populations.
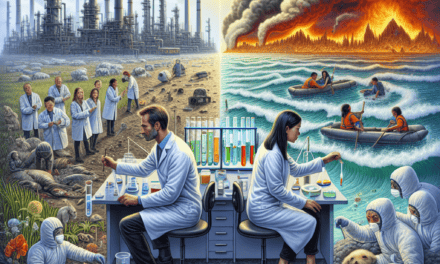
4. Health Disparities
Health disparities are a significant concern in rural areas, where residents often experience worse health outcomes compared to their urban counterparts.
4.1 Chronic Disease Prevalence
Chronic diseases, such as diabetes, heart disease, and obesity, are more prevalent in rural areas. This is due in part to limited access to preventive care and health education, as well as socioeconomic factors that contribute to unhealthy lifestyles.
Addressing chronic disease prevalence requires a multifaceted approach that includes improving access to care, promoting healthy behaviors, and addressing social determinants of health.
4.2 Mental Health Services
Mental health is another area where rural residents face significant disparities. Access to mental health services is often limited, with few providers available to meet the needs of the community.
Expanding mental health services in rural areas, including telepsychiatry and community-based programs, can help address this gap and improve mental health outcomes.
4.3 Health Literacy
Health literacy is a critical factor in healthcare delivery, and rural residents often have lower levels of health literacy compared to urban populations. This can impact their ability to understand and manage their health conditions.
Efforts to improve health literacy, such as community education programs and patient-centered communication strategies, can empower rural residents to take an active role in their healthcare.
5. Opportunities for Innovation
Despite the challenges, rural healthcare delivery presents numerous opportunities for innovation and improvement. By leveraging technology and community resources, rural areas can enhance healthcare access and quality.