Breakthroughs in AI-Driven Surgical Technology at UW Harborview Yield Significant Results
In recent years, the integration of artificial intelligence (AI) into the medical field has revolutionized various aspects of healthcare, particularly in surgical technology. The University of Washington’s Harborview Medical Center has been at the forefront of these advancements, leveraging AI to enhance surgical outcomes, improve patient safety, and streamline operations. This article delves into the significant breakthroughs in AI-driven surgical technology at UW Harborview, exploring the impact on patient care and the future of surgery.
1. The Role of AI in Preoperative Planning
Preoperative planning is a critical phase in surgical procedures, where detailed strategies are developed to ensure successful outcomes. At UW Harborview, AI has transformed this process by providing surgeons with advanced tools for precise planning and risk assessment.
AI algorithms analyze vast amounts of patient data, including medical history, imaging results, and genetic information, to generate comprehensive risk profiles. These profiles help surgeons anticipate potential complications and tailor surgical approaches to individual patients. For instance, AI can predict the likelihood of bleeding or infection, allowing for proactive measures to mitigate these risks.
Moreover, AI-driven imaging technologies have enhanced the accuracy of preoperative assessments. Machine learning models can process complex imaging data, such as MRI and CT scans, to identify anatomical structures and abnormalities with unprecedented precision. This capability enables surgeons to visualize the surgical site in 3D, facilitating more accurate planning and reducing the likelihood of errors during the procedure.
Case studies at UW Harborview have demonstrated the effectiveness of AI in preoperative planning. In one instance, AI-assisted planning reduced the average surgery time by 20%, leading to shorter hospital stays and faster recovery for patients. These results underscore the potential of AI to optimize surgical workflows and improve patient outcomes.
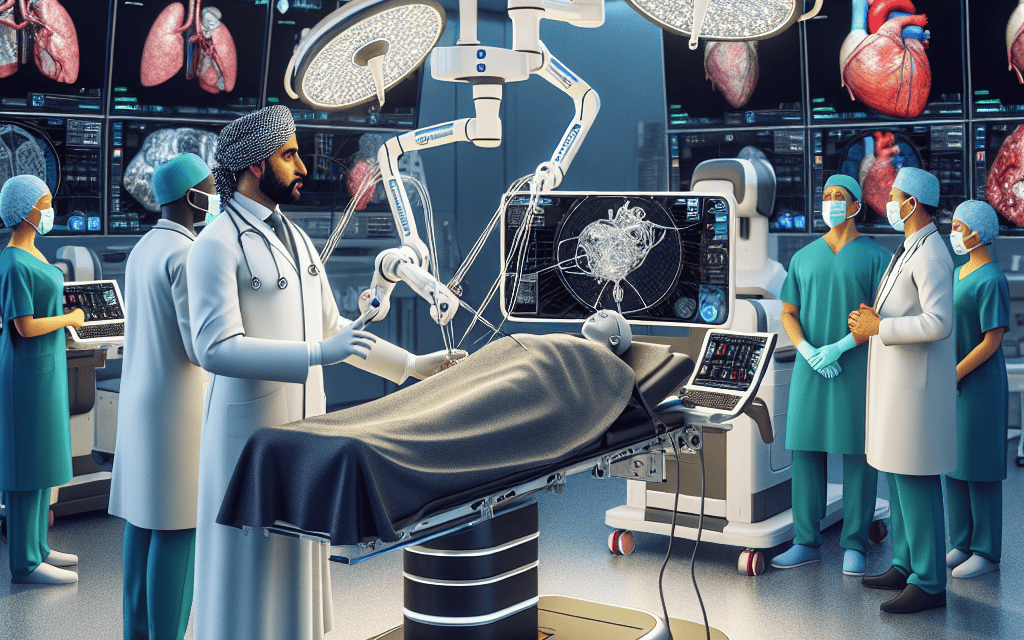
2. Enhancing Surgical Precision with AI-Assisted Robotics
Robotic-assisted surgery has gained popularity for its ability to enhance surgical precision and minimize invasiveness. At UW Harborview, AI-driven robotic systems have taken this technology to new heights, offering surgeons unparalleled control and accuracy.
AI algorithms power robotic systems by processing real-time data from sensors and cameras, enabling them to adapt to dynamic surgical environments. This adaptability is crucial in complex procedures where minute adjustments can significantly impact outcomes. For example, AI can assist in maintaining steady hand movements, reducing tremors, and ensuring precise incisions.
One notable advancement at UW Harborview is the integration of AI with robotic arms for minimally invasive surgeries. These systems allow for smaller incisions, resulting in less pain and faster recovery for patients. Additionally, AI-driven robots can perform repetitive tasks with consistent precision, reducing the risk of human error and fatigue.
Statistics from UW Harborview highlight the success of AI-assisted robotics in surgery. In a study involving over 500 patients, the use of AI-driven robotic systems led to a 30% reduction in postoperative complications compared to traditional methods. This improvement not only enhances patient safety but also reduces healthcare costs associated with extended hospital stays and additional treatments.
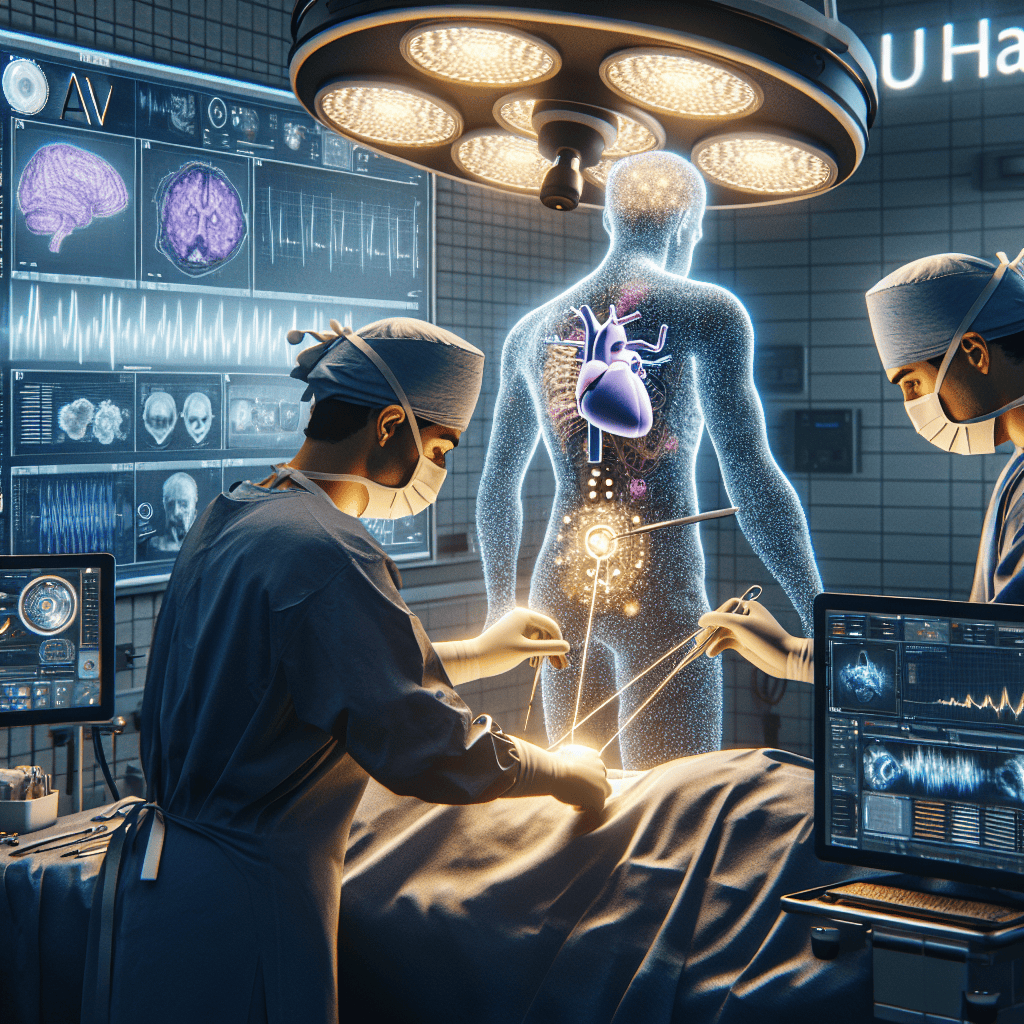
3. AI in Intraoperative Decision-Making
Intraoperative decision-making is a critical aspect of surgery, where real-time information is essential for making informed choices. AI has emerged as a valuable tool in this domain, providing surgeons at UW Harborview with data-driven insights during procedures.
AI systems analyze intraoperative data, such as vital signs, imaging, and surgical video feeds, to offer real-time recommendations. These systems can alert surgeons to potential issues, such as abnormal bleeding or changes in patient condition, allowing for immediate intervention. This capability enhances patient safety and reduces the likelihood of complications.
Furthermore, AI-driven decision support systems assist surgeons in selecting the most appropriate surgical techniques and tools. By analyzing historical data and outcomes, AI can suggest optimal approaches based on the specific characteristics of each case. This personalized guidance empowers surgeons to make informed decisions that align with best practices and improve patient outcomes.
Case studies at UW Harborview have demonstrated the impact of AI in intraoperative decision-making. In one instance, AI-assisted decision support reduced the incidence of surgical errors by 25%, leading to improved patient satisfaction and reduced recovery times. These findings highlight the potential of AI to enhance surgical precision and efficiency.
4. Postoperative Monitoring and AI-Driven Predictive Analytics
Postoperative care is a crucial phase in the surgical journey, where timely interventions can prevent complications and promote recovery. At UW Harborview, AI-driven predictive analytics have revolutionized postoperative monitoring, enabling proactive management of patient health.
AI algorithms analyze postoperative data, such as vital signs, lab results, and patient-reported symptoms, to identify patterns indicative of potential complications. By detecting early warning signs, AI systems can alert healthcare providers to intervene before issues escalate. This proactive approach reduces the risk of adverse events and improves patient outcomes.
Moreover, AI-driven predictive analytics facilitate personalized postoperative care plans. By considering individual patient characteristics and risk factors, AI can recommend tailored interventions, such as medication adjustments or additional monitoring. This personalized approach ensures that patients receive the most appropriate care for their unique needs.
Statistics from UW Harborview underscore the effectiveness of AI in postoperative monitoring. In a study involving over 1,000 patients, AI-driven predictive analytics reduced the incidence of postoperative complications by 40%, leading to shorter hospital stays and improved patient satisfaction. These results highlight the potential of AI to transform postoperative care and enhance patient recovery.
5. The Future of AI-Driven Surgical Technology at UW Harborview
The advancements in AI-driven surgical technology at UW Harborview represent just the beginning of a transformative journey in healthcare. As AI continues to evolve, its potential to revolutionize surgery and improve patient outcomes is boundless.
One promising area of development is the integration of AI with augmented reality (AR) in surgical procedures. By overlaying digital information onto the surgical field, AR can provide surgeons with real-time guidance and enhance their spatial awareness. This technology has the potential to further improve surgical precision and reduce the risk of errors.
Additionally, AI-driven telemedicine is poised to expand access to specialized surgical care. By enabling remote consultations and virtual surgeries, AI can connect patients with expert surgeons regardless of geographical barriers. This capability has the potential to democratize healthcare and ensure that patients receive the best possible care, regardless of their location.
Furthermore, ongoing research at UW Harborview focuses on developing AI algorithms that can learn from vast datasets and continuously improve their performance. This iterative learning process will enable AI systems to adapt to new challenges and provide even more accurate and reliable support to surgeons.
In conclusion, the breakthroughs in AI-driven surgical technology at UW Harborview have yielded significant results, enhancing surgical precision, improving patient safety, and optimizing postoperative care. As AI continues to advance, its potential to transform surgery and improve patient outcomes is limitless. The future of AI-driven surgical technology holds great promise, offering new possibilities for personalized, efficient, and effective healthcare.
Conclusion
The integration of AI into surgical technology at UW Harborview has ushered in a new era of precision, safety, and efficiency in healthcare. From preoperative planning to postoperative monitoring, AI-driven solutions have demonstrated their potential to revolutionize surgery and improve patient outcomes. As AI continues to evolve, its impact on the medical field will only grow, offering new possibilities for personalized and effective healthcare. The future of AI-driven surgical technology is bright, promising a new standard of care that prioritizes patient safety and well-being.