ASTP Completes Only Partial HTI-2, Leaving Health IT Developers Disappointed
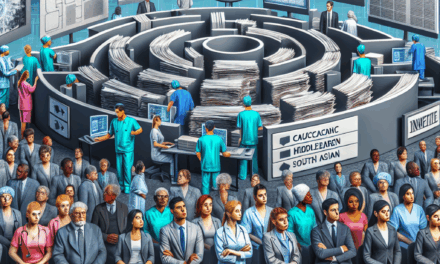
The landscape of health information technology (Health IT) is constantly evolving, driven by the need for improved patient care, data interoperability, and regulatory compliance. One of the most significant initiatives in this domain is the Health IT Certification Program, which aims to ensure that health IT products meet specific standards for functionality and interoperability. Recently, the American Society for Testing and Prevention (ASTP) announced the completion of only a partial Health IT Interoperability Test Initiative (HTI-2), leaving many health IT developers feeling disheartened. This article delves into the implications of this partial completion, the challenges faced by developers, and the broader impact on the healthcare ecosystem.
Understanding HTI-2: Objectives and Importance
The Health IT Interoperability Test Initiative (HTI-2) is a critical component of the certification process for health IT products. Its primary objective is to ensure that various health IT systems can communicate effectively with one another, thereby facilitating seamless data exchange across different platforms. This interoperability is essential for improving patient outcomes, reducing administrative burdens, and enhancing the overall efficiency of healthcare delivery.
HTI-2 was designed to address several key areas:
- Data Exchange Standards: Establishing common standards for data exchange to ensure that different systems can interpret and utilize shared information effectively.
- Interoperability Testing: Conducting rigorous testing of health IT products to verify their ability to exchange data with other systems.
- Regulatory Compliance: Ensuring that health IT products meet federal and state regulations regarding data privacy and security.
- Stakeholder Engagement: Involving various stakeholders, including healthcare providers, patients, and technology developers, in the testing process to gather diverse perspectives.
- Continuous Improvement: Creating a framework for ongoing evaluation and enhancement of health IT systems to keep pace with technological advancements.
The importance of HTI-2 cannot be overstated. As healthcare increasingly relies on digital solutions, the ability to share information across different platforms is vital for coordinated care. For instance, a patient visiting multiple specialists needs their medical history, lab results, and treatment plans to be accessible to all providers involved in their care. Without effective interoperability, critical information may be lost or delayed, leading to suboptimal patient outcomes.
The Disappointment of Partial Completion
The recent announcement by ASTP regarding the partial completion of HTI-2 has left many health IT developers disappointed. This partial completion means that not all aspects of the testing initiative were fully realized, raising concerns about the effectiveness of the certification process and the future of health IT interoperability.
Several factors contributed to this situation:
- Resource Constraints: Many health IT developers operate with limited resources, making it challenging to meet the rigorous demands of the HTI-2 testing process.
- Complexity of Interoperability: Achieving true interoperability is a complex task that requires collaboration among various stakeholders, including software vendors, healthcare providers, and regulatory bodies.
- Regulatory Changes: Frequent changes in regulations can create uncertainty for developers, making it difficult to align their products with the latest requirements.
- Technological Challenges: The rapid pace of technological advancement can outstrip the ability of health IT systems to adapt, leading to gaps in interoperability.
- Stakeholder Engagement: Insufficient engagement with key stakeholders during the testing process can result in a lack of buy-in and support for the initiative.
The disappointment among health IT developers is palpable. Many invested significant time and resources into preparing for the HTI-2 testing, only to find that the initiative did not yield the comprehensive results they had hoped for. This situation raises questions about the future of health IT certification and the commitment of regulatory bodies to support developers in achieving interoperability.
Impact on Health IT Developers
The partial completion of HTI-2 has far-reaching implications for health IT developers. Many are grappling with the consequences of this situation, which can affect their business operations, product development, and relationships with healthcare providers.
One of the most immediate impacts is the potential for lost revenue. Health IT developers rely on certification to market their products to healthcare organizations. Without full certification, developers may struggle to attract clients, leading to decreased sales and revenue. This situation is particularly concerning for smaller developers who may not have the financial cushion to weather such setbacks.
Additionally, the partial completion of HTI-2 may hinder innovation in the health IT space. Developers may be less inclined to invest in new features or enhancements if they perceive that the certification process is fraught with challenges. This stagnation could ultimately limit the availability of cutting-edge solutions that could improve patient care and streamline healthcare operations.
Moreover, the relationship between health IT developers and healthcare providers may be strained as a result of the partial completion. Providers often look to certified products to ensure compliance with regulatory requirements and to facilitate interoperability. If developers cannot provide fully certified solutions, providers may seek alternatives, further complicating the landscape for health IT vendors.
In response to these challenges, many health IT developers are advocating for greater transparency and support from regulatory bodies. They are calling for clearer guidelines on the certification process, as well as increased collaboration between developers and regulators to address the complexities of interoperability.
Case Studies: The Real-World Impact of HTI-2
To better understand the implications of the partial completion of HTI-2, it is essential to examine real-world case studies that highlight the challenges faced by health IT developers and the impact on healthcare delivery.
One notable case is that of a mid-sized health IT company that specializes in electronic health record (EHR) systems. This company invested heavily in preparing for the HTI-2 testing, believing that successful certification would open doors to new clients and partnerships. However, after the announcement of partial completion, the company faced significant backlash from potential clients who were hesitant to adopt a product that lacked full certification. As a result, the company experienced a sharp decline in sales and was forced to lay off several employees.
Another case involves a large healthcare organization that had been working closely with a health IT vendor to implement a new data exchange platform. The organization had high hopes for the project, as it aimed to improve care coordination among its various departments. However, when the vendor’s product received only partial certification, the organization had to reconsider its investment. The lack of full certification raised concerns about the platform’s ability to integrate with other systems, leading the organization to explore alternative solutions.
These case studies illustrate the tangible consequences of the partial completion of HTI-2. They highlight the challenges faced by health IT developers in navigating the certification process and the impact on healthcare organizations that rely on certified products to enhance patient care.
The Path Forward: Recommendations for Health IT Developers
In light of the challenges posed by the partial completion of HTI-2, health IT developers must adopt proactive strategies to navigate the evolving landscape of health information technology. Here are several recommendations for developers seeking to enhance their chances of success in the certification process:
- Invest in Interoperability: Developers should prioritize interoperability in their product design and development processes. By building systems that are inherently interoperable, they can better position themselves for successful certification.
- Engage with Regulatory Bodies: Establishing open lines of communication with regulatory bodies can help developers stay informed about changes in certification requirements and best practices for achieving compliance.
- Collaborate with Stakeholders: Engaging with healthcare providers, patients, and other stakeholders can provide valuable insights into the needs and expectations of end-users, ultimately leading to more effective solutions.
- Focus on Continuous Improvement: Developers should adopt a mindset of continuous improvement, regularly evaluating their products and processes to identify areas for enhancement and innovation.
- Advocate for Clear Guidelines: Developers should work collectively to advocate for clearer guidelines and support from regulatory bodies, ensuring that the certification process is transparent and achievable.
By implementing these strategies, health IT developers can better navigate the complexities of the certification process and position themselves for success in an increasingly competitive market.
Conclusion: Navigating the Future of Health IT
The partial completion of HTI-2 by ASTP has left many health IT developers disappointed and concerned about the future of interoperability in healthcare. The challenges faced by developers, coupled with the real-world implications of this situation, underscore the need for a collaborative approach to achieving true interoperability.
As the healthcare landscape continues to evolve, it is essential for health IT developers to prioritize interoperability, engage with stakeholders, and advocate for clearer guidelines from regulatory bodies. By doing so, they can enhance their chances of success in the certification process and contribute to a more connected and efficient healthcare ecosystem.
Ultimately, the journey toward achieving full interoperability is a collective effort that requires collaboration among developers, healthcare providers, and regulatory bodies. By working together, stakeholders can overcome the challenges posed by partial completions and pave the way for a future where health IT systems seamlessly communicate, ultimately improving patient care and outcomes.