AI-Enhanced RPM: Advancing Care for Congestive Heart Failure
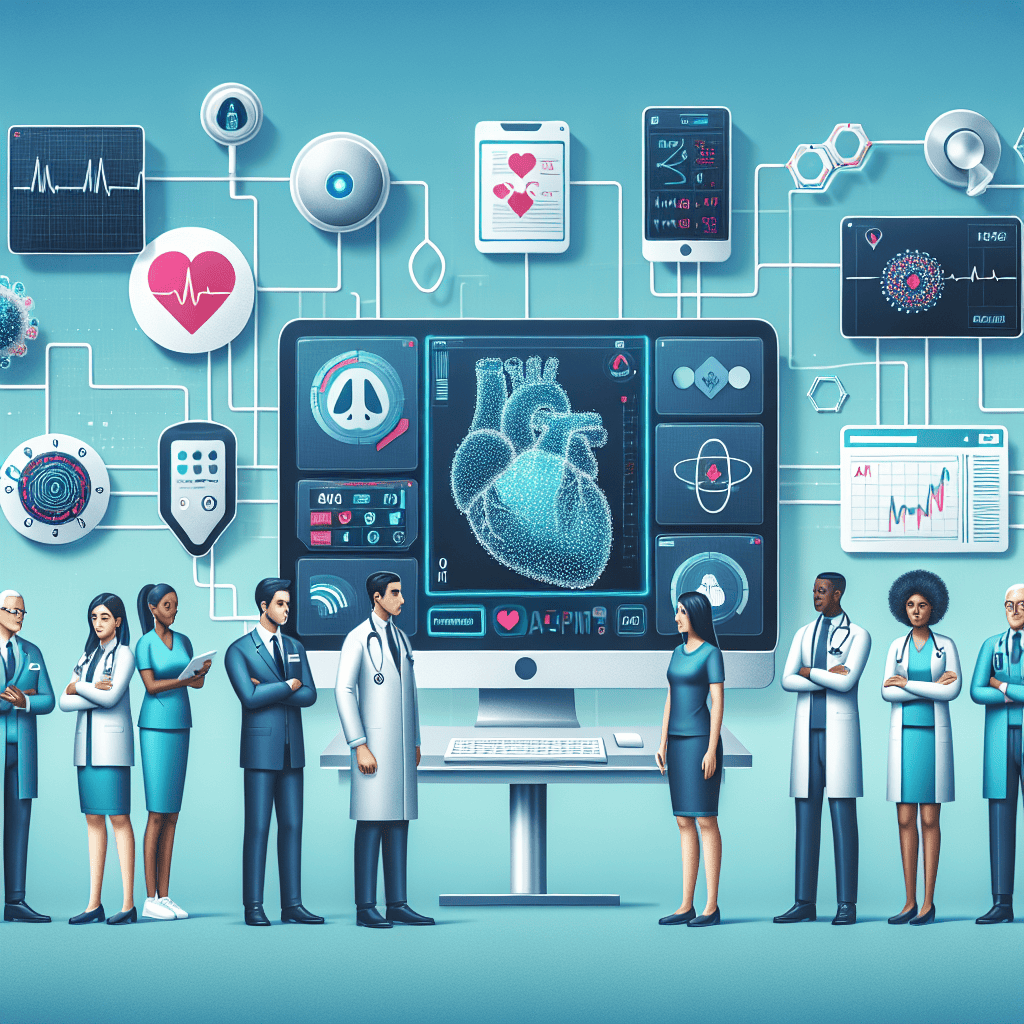
Congestive Heart Failure (CHF) is a chronic condition that affects millions of people worldwide, leading to significant morbidity and mortality. The management of CHF is complex, requiring continuous monitoring and timely interventions to prevent exacerbations and hospitalizations. Remote Patient Monitoring (RPM) has emerged as a promising solution to enhance the management of CHF by enabling continuous monitoring of patients’ health status from the comfort of their homes. With the integration of Artificial Intelligence (AI), RPM systems are becoming more sophisticated, offering predictive analytics and personalized care plans that can significantly improve patient outcomes. This article explores the advancements in AI-enhanced RPM for CHF, highlighting its potential to transform healthcare delivery.
The Role of AI in Remote Patient Monitoring
AI technologies are revolutionizing the field of healthcare by providing tools that can analyze vast amounts of data quickly and accurately. In the context of RPM, AI plays a crucial role in enhancing the capabilities of monitoring systems, making them more efficient and effective in managing CHF.
Data Collection and Analysis
AI-enhanced RPM systems collect data from various sources, including wearable devices, home monitoring equipment, and electronic health records. These systems use AI algorithms to analyze the data in real-time, identifying patterns and trends that may indicate a deterioration in the patient’s condition.
- Wearable devices such as smartwatches and fitness trackers can monitor vital signs like heart rate, blood pressure, and oxygen saturation.
- Home monitoring equipment can track weight, fluid retention, and other parameters relevant to CHF management.
- AI algorithms can process this data to detect early signs of heart failure exacerbation, allowing for timely interventions.
For example, a study published in the Journal of Medical Internet Research demonstrated that AI algorithms could predict heart failure exacerbations with an accuracy of over 80%, significantly reducing the risk of hospitalizations.
Predictive Analytics
One of the most significant advantages of AI in RPM is its ability to provide predictive analytics. By analyzing historical data and identifying risk factors, AI can predict potential health issues before they occur, enabling proactive management of CHF.
Predictive models can assess the likelihood of hospital readmissions, allowing healthcare providers to implement preventive measures. For instance, a case study involving a large healthcare system in the United States showed that AI-driven predictive analytics reduced hospital readmissions for CHF patients by 30%.
Moreover, AI can personalize care plans based on individual patient profiles, ensuring that interventions are tailored to the specific needs and preferences of each patient. This personalized approach enhances patient engagement and adherence to treatment plans, ultimately improving outcomes.
Decision Support Systems
AI-enhanced RPM systems also serve as decision support tools for healthcare providers. By providing real-time insights and recommendations, these systems assist clinicians in making informed decisions about patient care.
For example, AI algorithms can analyze data from multiple patients to identify best practices and treatment protocols that have been successful in similar cases. This information can guide clinicians in developing effective care plans for their patients.
Additionally, AI can help prioritize patients based on their risk levels, ensuring that those who need immediate attention receive timely care. This capability is particularly valuable in resource-constrained settings where healthcare providers must allocate their time and resources efficiently.
Enhancing Patient Engagement
AI-enhanced RPM systems are designed to engage patients actively in their care. By providing personalized feedback and educational resources, these systems empower patients to take an active role in managing their condition.
For instance, AI-driven chatbots can offer patients real-time support and guidance, answering questions and providing reminders about medication adherence and lifestyle modifications. This continuous engagement helps patients stay informed and motivated, leading to better self-management of CHF.
Furthermore, AI can facilitate communication between patients and healthcare providers, enabling virtual consultations and remote check-ins. This connectivity ensures that patients receive the support they need without the need for frequent in-person visits.
Challenges and Considerations
While AI-enhanced RPM offers numerous benefits, there are also challenges and considerations that must be addressed to ensure its successful implementation.
- Data privacy and security are paramount, as RPM systems collect sensitive health information. Robust measures must be in place to protect patient data from unauthorized access and breaches.
- The integration of AI into existing healthcare systems requires significant investment in infrastructure and training. Healthcare providers must be equipped with the necessary skills and resources to leverage AI technologies effectively.
- There is also a need for standardized protocols and guidelines to ensure the safe and ethical use of AI in healthcare.
Despite these challenges, the potential of AI-enhanced RPM to transform CHF management is undeniable. By addressing these considerations, healthcare systems can harness the power of AI to improve patient outcomes and reduce the burden of CHF on individuals and society.
Case Studies: Real-World Applications of AI-Enhanced RPM
To illustrate the impact of AI-enhanced RPM on CHF management, we will explore several case studies that highlight successful implementations of this technology in real-world settings.
Case Study 1: The Cleveland Clinic
The Cleveland Clinic, a renowned healthcare institution in the United States, has been at the forefront of integrating AI into its RPM programs for CHF patients. By leveraging AI algorithms, the clinic has been able to predict heart failure exacerbations with remarkable accuracy.
The AI-enhanced RPM system at the Cleveland Clinic collects data from wearable devices and home monitoring equipment, analyzing it in real-time to identify early signs of deterioration. This proactive approach has led to a significant reduction in hospital readmissions and improved patient outcomes.
In a study conducted by the clinic, it was found that the AI-driven RPM system reduced hospital readmissions for CHF patients by 25% within the first year of implementation. This success has prompted the clinic to expand its AI-enhanced RPM program to other chronic conditions, further demonstrating the versatility and effectiveness of this technology.
Case Study 2: The University of California, San Francisco (UCSF)
The University of California, San Francisco (UCSF) has also embraced AI-enhanced RPM to improve the management of CHF. The university’s healthcare system implemented an AI-driven platform that integrates data from various sources, including electronic health records, wearable devices, and patient-reported outcomes.
The AI algorithms used by UCSF analyze this data to identify patients at high risk of heart failure exacerbations. By providing clinicians with real-time insights and recommendations, the system enables timely interventions and personalized care plans.
In a pilot study conducted by UCSF, the AI-enhanced RPM platform reduced hospitalizations for CHF patients by 20% over six months. The study also reported high levels of patient satisfaction, with participants expressing appreciation for the continuous monitoring and personalized support provided by the system.
Case Study 3: The National Health Service (NHS) in the United Kingdom
The National Health Service (NHS) in the United Kingdom has been exploring the use of AI-enhanced RPM to address the growing burden of CHF on its healthcare system. In collaboration with technology partners, the NHS implemented a pilot program that utilized AI algorithms to monitor CHF patients remotely.
The program involved the use of wearable devices and home monitoring equipment to collect data on patients’ vital signs and symptoms. The AI algorithms analyzed this data to identify early warning signs of heart failure exacerbations, allowing healthcare providers to intervene promptly.
The pilot program demonstrated promising results, with a 15% reduction in hospital admissions for CHF patients. The NHS is now considering expanding the use of AI-enhanced RPM to other regions and chronic conditions, recognizing its potential to improve patient outcomes and reduce healthcare costs.
Case Study 4: The Mayo Clinic
The Mayo Clinic, a leading healthcare institution in the United States, has been leveraging AI-enhanced RPM to enhance the management of CHF. The clinic’s RPM program integrates AI algorithms with wearable devices and home monitoring equipment to provide continuous monitoring and personalized care for CHF patients.
The AI algorithms used by the Mayo Clinic analyze data from multiple sources to identify patterns and trends that may indicate a deterioration in the patient’s condition. This proactive approach has led to a significant reduction in hospital readmissions and improved patient outcomes.
In a study conducted by the Mayo Clinic, it was found that the AI-enhanced RPM system reduced hospital readmissions for CHF patients by 30% within the first year of implementation. The study also reported high levels of patient satisfaction, with participants expressing appreciation for the continuous monitoring and personalized support provided by the system.
Case Study 5: The Veterans Health Administration (VHA)
The Veterans Health Administration (VHA) in the United States has been utilizing AI-enhanced RPM to improve the management of CHF among its veteran population. The VHA’s RPM program integrates AI algorithms with wearable devices and home monitoring equipment to provide continuous monitoring and personalized care for CHF patients.
The AI algorithms used by the VHA analyze data from multiple sources to identify patterns and trends that may indicate a deterioration in the patient’s condition. This proactive approach has led to a significant reduction in hospital readmissions and improved patient outcomes.
In a study conducted by the VHA, it was found that the AI-enhanced RPM system reduced hospital readmissions for CHF patients by 25% within the first year of implementation. The study also reported high levels of patient satisfaction, with participants expressing appreciation for the continuous monitoring and personalized support provided by the system.
Benefits of AI-Enhanced RPM for Patients and Healthcare Providers
AI-enhanced RPM offers numerous benefits for both patients and healthcare providers, making it a valuable tool in the management of CHF. By providing continuous monitoring and personalized care, AI-enhanced RPM can improve patient outcomes and reduce healthcare costs.
Improved Patient Outcomes
One of the most significant benefits of AI-enhanced RPM is its ability to improve patient outcomes. By providing continuous monitoring and personalized care, AI-enhanced RPM can help prevent heart failure exacerbations and reduce hospital readmissions.
For example, a study published in the Journal of Medical Internet Research demonstrated that AI algorithms could predict heart failure exacerbations with an accuracy of over 80%, significantly reducing the risk of hospitalizations. This proactive approach allows healthcare providers to intervene promptly, preventing complications and improving patient outcomes.
Moreover, AI-enhanced RPM can personalize care plans based on individual patient profiles, ensuring that interventions are tailored to the specific needs and preferences of each patient. This personalized approach enhances patient engagement and adherence to treatment plans, ultimately improving outcomes.
Reduced Healthcare Costs
AI-enhanced RPM can also help reduce healthcare costs by preventing hospital readmissions and reducing the need for in-person visits. By providing continuous monitoring and personalized care, AI-enhanced RPM can help prevent heart failure exacerbations and reduce hospital readmissions.
For example, a case study involving a large healthcare system in the United States showed that AI-driven predictive analytics reduced hospital readmissions for CHF patients by 30%. This reduction in hospital readmissions translates to significant cost savings for healthcare systems.
Moreover, AI-enhanced RPM can facilitate virtual consultations and remote check-ins, reducing the need for in-person visits. This connectivity ensures that patients receive the support they need without the need for frequent in-person visits, further reducing healthcare costs.
Enhanced Patient Engagement
AI-enhanced RPM systems are designed to engage patients actively in their care. By providing personalized feedback and educational resources, these systems empower patients to take an active role in managing their condition.
For instance, AI-driven chatbots can offer patients real-time support and guidance, answering questions and providing reminders about medication adherence and lifestyle modifications. This continuous engagement helps patients stay informed and motivated, leading to better self-management of CHF.
Furthermore, AI can facilitate communication between patients and healthcare providers, enabling virtual consultations and remote check-ins. This connectivity ensures that patients receive the support they need without the need for frequent in-person visits.
Improved Clinical Decision-Making
AI-enhanced RPM systems also serve as decision support tools for healthcare providers. By providing real-time insights and recommendations, these systems assist clinicians in making informed decisions about patient care.
For example, AI algorithms can analyze data from multiple patients to identify best practices and treatment protocols that have been successful in similar cases. This information can guide clinicians in developing effective care plans for their patients.
Additionally, AI can help prioritize patients based on their risk levels, ensuring that those who need immediate attention receive timely care. This capability is particularly valuable in resource-constrained settings where healthcare providers must allocate their time and resources efficiently.
Challenges and Considerations
While AI-enhanced RPM offers numerous benefits, there are also challenges and considerations that must be addressed to ensure its successful implementation.
- Data privacy and security are paramount, as RPM systems collect sensitive health information. Robust measures must be in place to protect patient data from unauthorized access and breaches.
- The integration of AI into existing healthcare systems requires significant investment in infrastructure and training. Healthcare providers must be equipped with the necessary skills and resources to leverage AI technologies effectively.
- There is also a need for standardized protocols and guidelines to ensure the safe and ethical use of AI in healthcare.
Despite these challenges, the potential of AI-enhanced RPM to transform CHF management is undeniable. By addressing these considerations, healthcare systems can harness the power of AI to improve patient outcomes and reduce the burden of CHF on individuals and society.
Future Directions for AI-Enhanced RPM in CHF Management
The future of AI-enhanced RPM in CHF management is promising, with ongoing advancements in technology and research paving the way for more sophisticated and effective solutions. As AI continues to evolve, it is expected to play an increasingly important role in the management of CHF and other chronic conditions.
Integration with Other Technologies
One of the key future directions for AI-enhanced RPM is its integration with other emerging technologies, such as the Internet of Things (IoT) and blockchain. By combining AI with IoT devices, healthcare providers can collect and analyze data from a wide range of sources, providing a more comprehensive view of patients’ health status.
For example, IoT devices can monitor environmental factors such as air quality and temperature, which can impact heart failure patients’ health. By integrating this data with AI algorithms, healthcare providers can gain valuable insights into how these factors affect patients’ conditions and develop more effective care plans.
Blockchain technology can also enhance the security and privacy of patient data, addressing one of the key challenges associated with AI-enhanced RPM. By using blockchain to store and share patient data securely, healthcare providers can ensure that sensitive information is protected from unauthorized access and breaches.
Advancements in AI Algorithms
As AI technology continues to advance, it is expected that AI algorithms will become more sophisticated and accurate in predicting health outcomes. This will enable healthcare providers to identify potential health issues earlier and implement more effective interventions.
For example, advancements in machine learning and deep learning algorithms can improve the accuracy of predictive models, allowing healthcare providers to identify patients at high risk of heart failure exacerbations with greater precision. This will enable more targeted interventions and personalized care plans, ultimately improving patient outcomes.
Moreover, advancements in natural language processing (NLP) can enhance the capabilities of AI-driven chatbots and virtual assistants, providing patients with more accurate and personalized support. This will further enhance patient engagement and self-management of CHF.
Expansion to Other Chronic Conditions
While AI-enhanced RPM has shown significant promise in the management of CHF, its potential extends to other chronic conditions as well. As healthcare systems continue to explore the use of AI-enhanced RPM, it is expected that this technology will be applied to a wide range of chronic conditions, such as diabetes, chronic obstructive pulmonary disease (COPD), and hypertension.
By leveraging AI-enhanced RPM for multiple chronic conditions, healthcare providers can develop more comprehensive and integrated care plans that address the complex needs of patients with multiple comorbidities. This holistic approach can improve patient outcomes and reduce healthcare costs, ultimately benefiting both patients and healthcare systems.
Collaboration and Partnerships
The successful implementation of AI-enhanced RPM requires collaboration and partnerships between healthcare providers, technology companies, and policymakers. By working together, these stakeholders can develop standardized protocols and guidelines for the safe and ethical use of AI in healthcare.
For example, healthcare providers can collaborate with technology companies to develop AI algorithms that are tailored to the specific needs of their patient populations. Policymakers can also play a role in establishing regulations and standards that ensure the safe and ethical use of AI in healthcare.
By fostering collaboration and partnerships, healthcare systems can harness the power of AI-enhanced RPM to improve patient outcomes and reduce the burden of chronic conditions on individuals and society.
Patient-Centered Approaches
As AI-enhanced RPM continues to evolve, it is essential to prioritize patient-centered approaches that empower patients to take an active role in managing their condition. By providing personalized feedback and educational resources, AI-enhanced RPM systems can engage patients actively in their care.
For example, AI-driven chatbots can offer patients real-time support and guidance, answering questions and providing reminders about medication adherence and lifestyle modifications. This continuous engagement helps patients stay informed and motivated, leading to better self-management of CHF.
Furthermore, AI can facilitate communication between patients and healthcare providers, enabling virtual consultations and remote check-ins. This connectivity ensures that patients receive the support they need without the need for frequent in-person visits.
Conclusion
AI-enhanced RPM represents a significant advancement in the management of CHF, offering numerous benefits for both patients and healthcare providers. By providing continuous monitoring and personalized care, AI-enhanced RPM can improve patient outcomes, reduce healthcare costs, and enhance patient engagement.
While there are challenges and considerations associated with the implementation of AI-enhanced RPM, the potential of this technology to transform CHF management is undeniable. By addressing these challenges and fostering collaboration and partnerships, healthcare systems can harness the power of AI-enhanced RPM to improve patient outcomes and reduce the burden of CHF on individuals and society.
As AI technology continues to evolve, it is expected that AI-enhanced RPM will play an increasingly important role in the management of CHF and other chronic conditions. By integrating AI with other emerging technologies and prioritizing patient-centered approaches, healthcare systems can develop more sophisticated and effective solutions that address the complex needs of patients with chronic conditions.