AHA Raises Concerns Over HTI-2 Deadlines and Challenging Requirements
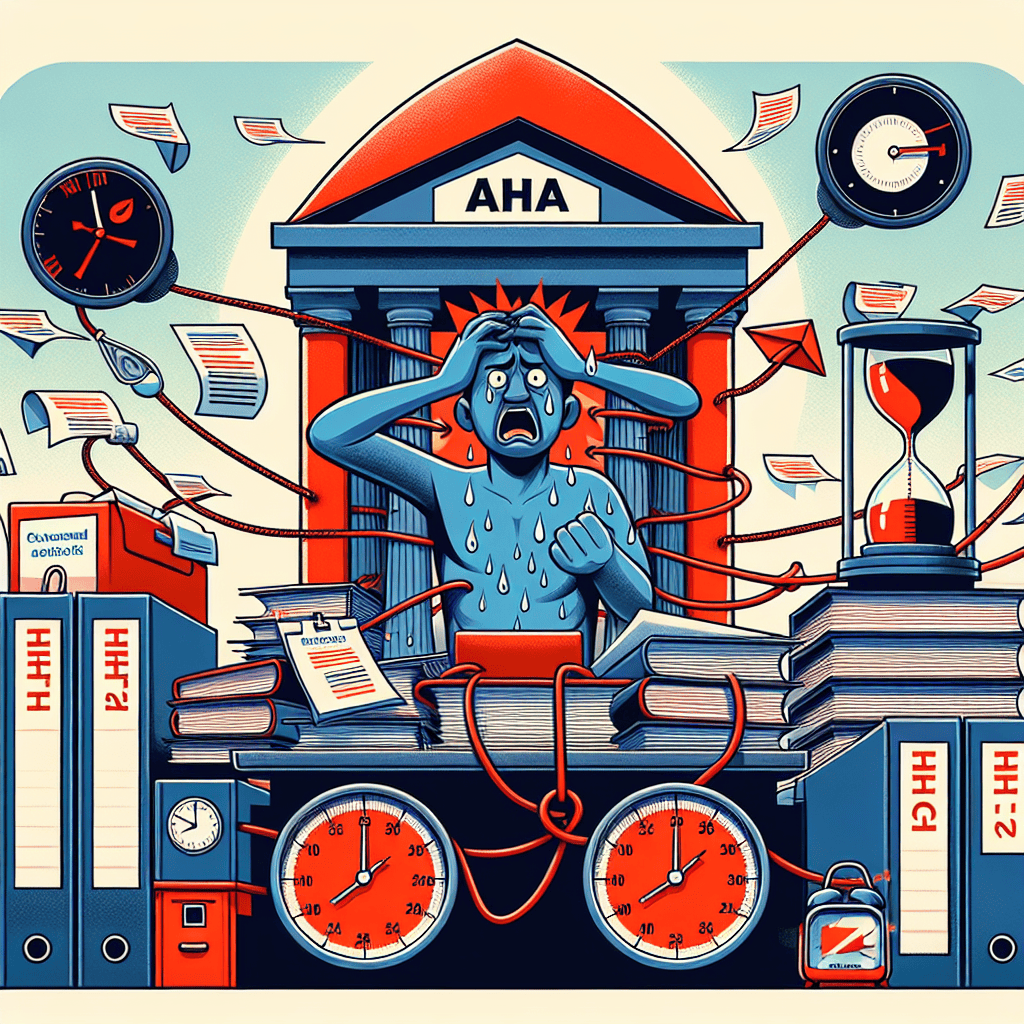
The American Hospital Association (AHA) has recently voiced significant concerns regarding the Health Information Technology for Economic and Clinical Health Act (HITECH) Stage 2, commonly referred to as HTI-2. The AHA’s apprehensions primarily revolve around the stringent deadlines and challenging requirements imposed by HTI-2, which they argue could potentially hinder healthcare providers’ ability to deliver quality care. This article delves into the various aspects of these concerns, exploring the implications for healthcare providers, the potential impact on patient care, and the broader healthcare landscape.
Understanding HTI-2: An Overview
To fully grasp the AHA’s concerns, it’s essential to first understand what HTI-2 entails. The Health Information Technology for Economic and Clinical Health Act (HITECH) was enacted as part of the American Recovery and Reinvestment Act of 2009, with the aim of promoting the adoption and meaningful use of health information technology. HTI-2 represents the second stage of this initiative, focusing on the advanced use of electronic health records (EHRs) to improve patient care.
HTI-2 introduces a set of criteria that healthcare providers must meet to demonstrate meaningful use of EHRs. These criteria are designed to ensure that EHRs are used effectively to enhance patient care, improve clinical outcomes, and facilitate better coordination among healthcare providers. However, the AHA argues that the deadlines and requirements associated with HTI-2 are overly ambitious and may pose significant challenges for healthcare providers.
The Ambitious Deadlines of HTI-2
One of the primary concerns raised by the AHA is the ambitious deadlines set by HTI-2. Healthcare providers are required to meet specific criteria within a limited timeframe to qualify for incentive payments and avoid penalties. The AHA argues that these deadlines do not take into account the complexities involved in implementing and optimizing EHR systems, particularly for smaller healthcare facilities with limited resources.
For instance, many healthcare providers face challenges in upgrading their existing EHR systems to meet HTI-2 requirements. This process often involves significant financial investments, staff training, and workflow adjustments, all of which require time and careful planning. The AHA contends that the current deadlines do not provide sufficient time for healthcare providers to make these necessary adjustments without compromising patient care.
Moreover, the AHA highlights the potential for increased administrative burden on healthcare providers as they strive to meet HTI-2 deadlines. This burden can divert valuable resources away from direct patient care, potentially impacting the quality of care provided to patients. The AHA calls for a more flexible approach to HTI-2 deadlines, allowing healthcare providers to implement changes at a pace that aligns with their unique circumstances and capabilities.
Challenging Requirements: A Barrier to Meaningful Use
In addition to the ambitious deadlines, the AHA has expressed concerns about the challenging requirements imposed by HTI-2. These requirements are designed to ensure that healthcare providers use EHRs in a way that meaningfully improves patient care. However, the AHA argues that some of these requirements may be overly prescriptive and difficult to achieve, particularly for smaller healthcare facilities.
For example, HTI-2 requires healthcare providers to demonstrate the ability to exchange health information with other providers and patients in a secure and efficient manner. While this goal is laudable, the AHA points out that many healthcare providers face significant technical and logistical challenges in achieving this level of interoperability. These challenges can be particularly pronounced for rural and underserved healthcare facilities, which may lack the necessary infrastructure and resources to meet HTI-2 requirements.
Furthermore, the AHA argues that the focus on meeting specific criteria may inadvertently lead to a checkbox mentality, where healthcare providers prioritize compliance over genuine improvements in patient care. This approach can undermine the overall goals of HTI-2, as healthcare providers may focus on meeting requirements rather than leveraging EHRs to enhance patient outcomes and care coordination.
The Impact on Patient Care
The AHA’s concerns about HTI-2 deadlines and requirements are not solely focused on the challenges faced by healthcare providers. The organization also highlights the potential impact on patient care, arguing that the current approach to HTI-2 may inadvertently compromise the quality of care provided to patients.
One of the key concerns is the potential for increased administrative burden on healthcare providers as they strive to meet HTI-2 requirements. This burden can divert valuable resources away from direct patient care, potentially impacting the quality of care provided to patients. The AHA argues that a more flexible approach to HTI-2 deadlines and requirements could help alleviate this burden, allowing healthcare providers to focus on delivering high-quality care to their patients.
Additionally, the AHA points out that the focus on meeting specific criteria may lead to a one-size-fits-all approach to patient care. This approach can overlook the unique needs and circumstances of individual patients, potentially compromising the quality of care provided. The AHA calls for a more patient-centered approach to HTI-2, where healthcare providers are encouraged to use EHRs in a way that aligns with the specific needs and preferences of their patients.
Case Studies: Real-World Challenges and Solutions
To illustrate the challenges faced by healthcare providers in meeting HTI-2 requirements, the AHA has highlighted several case studies from across the country. These case studies provide valuable insights into the real-world challenges and potential solutions for healthcare providers striving to achieve meaningful use of EHRs.
One such case study involves a small rural hospital in the Midwest, which faced significant challenges in upgrading its EHR system to meet HTI-2 requirements. The hospital lacked the necessary financial resources and technical expertise to implement the required changes, leading to delays and increased administrative burden. However, by partnering with a larger healthcare system, the hospital was able to access the necessary resources and support to successfully meet HTI-2 requirements.
Another case study involves a large urban hospital that struggled to achieve interoperability with other healthcare providers in its region. The hospital faced significant technical challenges in exchanging health information with other providers, leading to delays in patient care and increased administrative burden. By investing in advanced interoperability solutions and collaborating with other healthcare providers, the hospital was able to overcome these challenges and achieve meaningful use of EHRs.
These case studies highlight the importance of collaboration and resource-sharing in overcoming the challenges associated with HTI-2. The AHA argues that a more flexible approach to HTI-2 deadlines and requirements could facilitate greater collaboration among healthcare providers, ultimately leading to improved patient care and outcomes.
Recommendations for a More Flexible Approach
In light of the challenges and concerns associated with HTI-2, the AHA has put forward several recommendations for a more flexible approach to the initiative. These recommendations are designed to address the unique needs and circumstances of healthcare providers, while still achieving the overall goals of HTI-2.
One of the key recommendations is to extend the deadlines for meeting HTI-2 requirements, allowing healthcare providers more time to implement necessary changes and optimize their EHR systems. The AHA argues that this extension would help alleviate the administrative burden on healthcare providers, allowing them to focus on delivering high-quality care to their patients.
Additionally, the AHA recommends a more flexible approach to HTI-2 requirements, allowing healthcare providers to tailor their use of EHRs to the specific needs and circumstances of their patients. This approach would encourage healthcare providers to prioritize genuine improvements in patient care over mere compliance with specific criteria.
Finally, the AHA calls for increased support and resources for healthcare providers, particularly those in rural and underserved areas. This support could include financial assistance, technical expertise, and access to advanced interoperability solutions, helping healthcare providers overcome the challenges associated with HTI-2 and achieve meaningful use of EHRs.
Conclusion: Balancing Ambition with Practicality
The AHA’s concerns over HTI-2 deadlines and challenging requirements highlight the need for a more balanced approach to health information technology initiatives. While the goals of HTI-2 are laudable, the current approach may inadvertently hinder healthcare providers’ ability to deliver quality care. By adopting a more flexible approach to deadlines and requirements, and providing increased support and resources for healthcare providers, the AHA believes that the goals of HTI-2 can be achieved without compromising patient care.
Ultimately, the success of HTI-2 will depend on the ability of healthcare providers to effectively leverage EHRs to enhance patient care and outcomes. By addressing the challenges and concerns raised by the AHA, policymakers can help ensure that HTI-2 achieves its intended goals, while also supporting healthcare providers in their mission to deliver high-quality care to their patients.