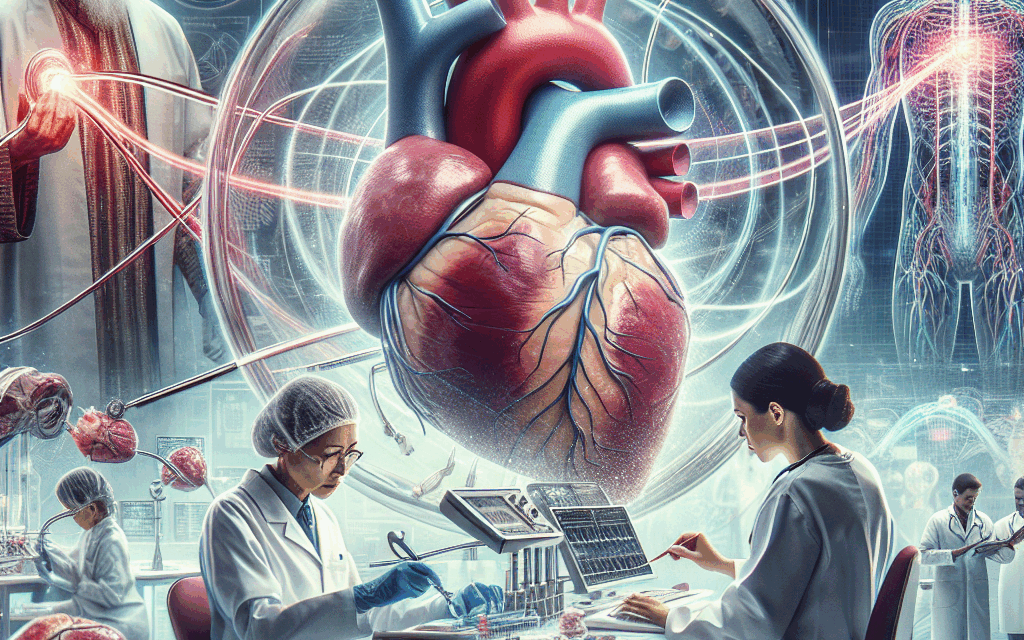
Advancements in Heart Failure Therapies
Heart failure (HF) is a complex clinical syndrome that arises when the heart is unable to pump sufficiently to maintain blood flow to meet the body’s needs. It affects millions of people worldwide and is a leading cause of morbidity and mortality. Over the past few decades, significant advancements in heart failure therapies have emerged, improving patient outcomes and quality of life. This article explores the latest developments in heart failure therapies, focusing on five key areas: pharmacological treatments, device-based therapies, lifestyle modifications, gene therapy, and future directions in heart failure management.
Pharmacological Treatments
Pharmacological therapy remains the cornerstone of heart failure management. The landscape of heart failure medications has evolved significantly, with new classes of drugs and novel mechanisms of action being introduced. The primary goal of these medications is to alleviate symptoms, improve functional capacity, and reduce mortality.
Traditionally, heart failure treatment has relied on a combination of diuretics, ACE inhibitors, beta-blockers, and aldosterone antagonists. However, recent advancements have introduced new agents that target specific pathways involved in heart failure.
- SGLT2 Inhibitors: Sodium-glucose cotransporter 2 (SGLT2) inhibitors, originally developed for diabetes management, have shown remarkable benefits in heart failure patients, particularly those with reduced ejection fraction (HFrEF). Clinical trials such as EMPEROR-Reduced and DAPA-HF have demonstrated that these agents significantly reduce the risk of hospitalization for heart failure and cardiovascular death.
- ARNI Therapy: Angiotensin receptor-neprilysin inhibitors (ARNIs), such as sacubitril/valsartan, have revolutionized heart failure treatment. The PARADIGM-HF trial established that ARNI therapy reduces the risk of cardiovascular death and hospitalization compared to traditional ACE inhibitors. This dual mechanism of action not only lowers blood pressure but also enhances natriuresis and reduces cardiac remodeling.
- New Beta-Blockers: While beta-blockers have been a staple in heart failure management, newer agents like carvedilol and bisoprolol have shown improved outcomes in specific populations. Ongoing research is exploring the role of beta-blockers in patients with preserved ejection fraction (HFpEF).
- Vasodilators: Novel vasodilators, such as vericiguat, have emerged as promising options for patients with worsening heart failure. The VICTORIA trial demonstrated that vericiguat significantly reduced the risk of cardiovascular death and heart failure hospitalization in patients with chronic heart failure.
- Combination Therapies: The future of heart failure pharmacotherapy may lie in combination therapies that target multiple pathways simultaneously. Ongoing studies are investigating the synergistic effects of combining SGLT2 inhibitors with ARNI therapy, which may further enhance patient outcomes.
In summary, advancements in pharmacological treatments for heart failure have led to improved outcomes for patients. The introduction of SGLT2 inhibitors and ARNI therapy has transformed the management of heart failure, providing new hope for patients with this chronic condition.
Device-Based Therapies
Device-based therapies have become an integral part of heart failure management, particularly for patients with advanced disease. These interventions aim to improve cardiac function, alleviate symptoms, and enhance the quality of life. The following are key advancements in device-based therapies for heart failure:
- Implantable Cardioverter-Defibrillators (ICDs): ICDs are essential for preventing sudden cardiac death in patients with heart failure and reduced ejection fraction. Recent studies have reinforced the importance of early ICD implantation in eligible patients, demonstrating a significant reduction in mortality rates.
- Cardiac Resynchronization Therapy (CRT): CRT has been shown to improve outcomes in patients with heart failure and ventricular dyssynchrony. The latest guidelines recommend CRT for patients with HFrEF who remain symptomatic despite optimal medical therapy. Ongoing research is exploring the use of CRT in patients with HFpEF.
- Left Ventricular Assist Devices (LVADs): LVADs have become a viable option for patients with end-stage heart failure who are not candidates for heart transplantation. Recent advancements in LVAD technology have led to smaller, more efficient devices that improve patient mobility and quality of life. The MOMENTUM 3 trial demonstrated that continuous-flow LVADs provide better outcomes compared to pulsatile devices.
- Wearable Devices: The rise of wearable technology has opened new avenues for heart failure management. Devices that monitor heart rate, rhythm, and physical activity can provide real-time data to healthcare providers, enabling timely interventions and personalized care. Studies have shown that remote monitoring can reduce hospitalizations and improve patient adherence to treatment.
- Bioelectronic Medicine: Emerging bioelectronic therapies aim to modulate neural pathways involved in heart failure. Devices that stimulate the vagus nerve have shown promise in preclinical studies, potentially offering a novel approach to managing heart failure symptoms.
Device-based therapies have significantly advanced the management of heart failure, providing patients with new options for improving their condition. As technology continues to evolve, the integration of these devices into routine care will likely enhance patient outcomes and quality of life.
Lifestyle Modifications
While pharmacological and device-based therapies are crucial for managing heart failure, lifestyle modifications play a vital role in improving patient outcomes. Adopting a heart-healthy lifestyle can help alleviate symptoms, enhance functional capacity, and reduce the risk of hospitalization. Key lifestyle modifications include:
- Dietary Changes: A heart-healthy diet is essential for managing heart failure. Patients are encouraged to follow a low-sodium diet to reduce fluid retention and blood pressure. The DASH (Dietary Approaches to Stop Hypertension) diet, rich in fruits, vegetables, whole grains, and lean proteins, has been shown to improve cardiovascular health.
- Physical Activity: Regular physical activity is crucial for heart failure patients. Exercise training programs tailored to individual capabilities can improve exercise tolerance, reduce symptoms, and enhance quality of life. The HF-ACTION trial demonstrated that exercise training significantly improves functional capacity and quality of life in patients with HFrEF.
- Weight Management: Maintaining a healthy weight is essential for heart failure management. Obesity can exacerbate heart failure symptoms and increase the risk of comorbidities. Weight loss through dietary changes and physical activity can lead to significant improvements in heart function and overall health.
- Smoking Cessation: Smoking is a major risk factor for cardiovascular disease and can worsen heart failure symptoms. Smoking cessation programs have been shown to improve outcomes in heart failure patients, reducing the risk of hospitalization and mortality.
- Stress Management: Chronic stress can negatively impact heart health. Techniques such as mindfulness, meditation, and cognitive-behavioral therapy can help patients manage stress and improve their overall well-being.
Incorporating lifestyle modifications into heart failure management can lead to significant improvements in patient outcomes. Healthcare providers should emphasize the importance of these changes and provide support to help patients adopt and maintain a heart-healthy lifestyle.
Gene Therapy
Gene therapy represents a groundbreaking approach to treating heart failure by targeting the underlying genetic and molecular mechanisms of the disease. While still in the experimental stages, advancements in gene therapy hold promise for transforming heart failure management. Key areas of research include:
- Gene Editing Technologies: Technologies such as CRISPR-Cas9 have revolutionized gene editing, allowing for precise modifications to the genome. Researchers are exploring the potential of gene editing to correct genetic mutations associated with inherited cardiomyopathies, which can lead to heart failure.
- Gene Delivery Systems: Effective delivery of therapeutic genes to cardiac tissues is crucial for successful gene therapy. Advances in viral and non-viral delivery systems are being developed to enhance the efficiency and safety of gene transfer to the heart.
- Myocardial Regeneration: Gene therapy has the potential to promote myocardial regeneration by delivering genes that stimulate cardiac cell proliferation and repair. Studies have shown that delivering growth factors or transcription factors can enhance cardiac function in animal models of heart failure.
- Targeting Inflammation: Inflammation plays a significant role in the progression of heart failure. Gene therapies that target inflammatory pathways may help mitigate cardiac damage and improve outcomes. Research is ongoing to identify specific genes that can modulate the inflammatory response in heart failure.
- Clinical Trials: Several clinical trials are underway to evaluate the safety and efficacy of gene therapies for heart failure. For example, the AAV1/SERCA2a gene therapy has shown promise in early-phase trials, demonstrating improvements in cardiac function and exercise capacity in patients with advanced heart failure.
While gene therapy for heart failure is still in its infancy, the potential for targeted, personalized treatments offers hope for patients with this challenging condition. Continued research and clinical trials will be essential to determine the feasibility and effectiveness of these innovative approaches.
Future Directions in Heart Failure Management
The future of heart failure management is poised for significant advancements, driven by ongoing research and technological innovations. Several key trends and areas of focus are shaping the future landscape of heart failure therapies:
- Personalized Medicine: The shift towards personalized medicine aims to tailor treatments based on individual patient characteristics, including genetic profiles, comorbidities, and response to therapy. Biomarkers and genetic testing will play a crucial role in guiding treatment decisions and optimizing outcomes.
- Telemedicine: The COVID-19 pandemic accelerated the adoption of telemedicine in healthcare. Remote monitoring and virtual consultations are becoming integral to heart failure management, allowing for timely interventions and improved patient engagement. Studies have shown that telehealth can reduce hospitalizations and enhance patient satisfaction.
- Artificial Intelligence (AI): AI and machine learning are being integrated into heart failure management to analyze large datasets and identify patterns that can inform treatment decisions. Predictive analytics can help identify patients at high risk for hospitalization, enabling proactive interventions.
- Regenerative Medicine: Advances in regenerative medicine, including stem cell therapy and tissue engineering, hold promise for repairing damaged cardiac tissue and restoring heart function. Ongoing research is exploring the potential of stem cells to regenerate myocardium in heart failure patients.
- Global Health Initiatives: Addressing heart failure as a global health challenge is essential for improving outcomes worldwide. Initiatives aimed at increasing awareness, access to care, and education about heart failure will be crucial in reducing the burden of this condition, particularly in low- and middle-income countries.
The future of heart failure management is bright, with ongoing advancements in therapies and technologies that promise to improve patient outcomes. As research continues to evolve, healthcare providers must stay informed about the latest developments to provide the best possible care for their patients.
Conclusion
Advancements in heart failure therapies have transformed the landscape of this complex condition, offering new hope for patients and healthcare providers alike. From innovative pharmacological treatments and device-based therapies to lifestyle modifications and emerging gene therapies, the future of heart failure management is promising. As we continue to explore new frontiers in research and technology, it is essential to prioritize patient-centered care and ensure that all individuals with heart failure have access to the latest advancements in treatment.
In summary, the key takeaways from this article include:
- The evolution of pharmacological treatments, including SGLT2 inhibitors and ARNI therapy, has significantly improved outcomes for heart failure patients.
- Device-based therapies, such as ICDs and LVADs, play a crucial role in managing advanced heart failure and preventing sudden cardiac death.
- Lifestyle modifications are essential for enhancing patient outcomes and should be emphasized in heart failure management.
- Gene therapy holds promise for targeting the underlying mechanisms of heart failure, with ongoing research exploring its potential.
- The future of heart failure management will be shaped by personalized medicine, telemedicine, AI, regenerative medicine, and global health initiatives.
As we move forward, continued research, collaboration, and innovation will be vital in improving the lives of those affected by heart failure.