Elevance Takes Legal Action Against Georgia Providers Over No Surprises Arbitration Allegations
The healthcare landscape in the United States is undergoing significant changes, particularly with the implementation of the No Surprises Act, which aims to protect patients from unexpected medical bills. In a recent development, Elevance Health, a major player in the health insurance industry, has initiated legal action against several healthcare providers in Georgia. This article delves into the intricacies of this legal battle, exploring the implications of the No Surprises Act, the allegations made by Elevance, and the broader context of healthcare arbitration in the U.S.
Understanding the No Surprises Act
The No Surprises Act, enacted as part of the Consolidated Appropriations Act of 2021, was designed to address the issue of surprise medical billing. Surprise billing occurs when patients receive care from out-of-network providers without their knowledge, leading to unexpectedly high medical bills. The Act aims to protect patients by prohibiting balance billing in certain situations and establishing a framework for resolving payment disputes between insurers and providers.
Key provisions of the No Surprises Act include:
- Prohibition of Balance Billing: Patients cannot be billed for out-of-network services without their consent in emergency situations or when they receive care from out-of-network providers at in-network facilities.
- Arbitration Process: The Act establishes an arbitration process for resolving payment disputes between insurers and providers, allowing both parties to negotiate fair compensation for services rendered.
- Transparency Requirements: Providers must inform patients about their network status and potential out-of-pocket costs before delivering services.
The No Surprises Act represents a significant shift in how healthcare billing is managed, aiming to create a more transparent and equitable system for patients. However, its implementation has not been without controversy, particularly regarding the arbitration process and how it affects the financial dynamics between insurers and providers.
The Allegations Against Georgia Providers
Elevance Health’s legal action against Georgia providers centers around allegations of improper practices related to the arbitration process established by the No Surprises Act. The company claims that certain providers have engaged in tactics that undermine the intent of the legislation, leading to inflated costs for patients and insurers alike.
Specific allegations include:
- Manipulation of Billing Codes: Elevance alleges that some providers have been using incorrect or inflated billing codes to maximize their reimbursement during arbitration, which contradicts the spirit of fair negotiation.
- Refusal to Engage in Good Faith Negotiations: The company claims that certain providers have not been negotiating in good faith, leading to prolonged arbitration processes and increased costs for patients.
- Excessive Charges for Services: Elevance argues that some providers are charging excessively for services that should be covered under the No Surprises Act, placing an undue financial burden on patients.
These allegations highlight the complexities of implementing the No Surprises Act and the challenges faced by insurers in ensuring compliance among healthcare providers. Elevance’s legal action aims to address these issues and hold providers accountable for their billing practices.
The Impact of Legal Action on Healthcare Providers
The legal action taken by Elevance against Georgia providers has significant implications for the healthcare landscape in the state and beyond. As the No Surprises Act continues to be implemented, the outcomes of this case could set important precedents for how similar disputes are handled in the future.
Potential impacts include:
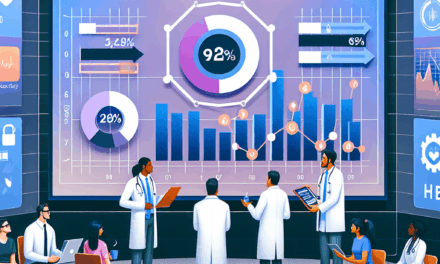
- Increased Scrutiny of Billing Practices: Providers may face heightened scrutiny regarding their billing practices, leading to a reevaluation of how services are priced and billed.
- Changes in Negotiation Strategies: The legal action may prompt providers to adopt more transparent and fair negotiation strategies to avoid similar disputes in the future.
- Financial Consequences: If Elevance’s allegations are upheld, providers may face financial penalties or be required to adjust their billing practices, impacting their revenue streams.
Moreover, the case could influence how other insurers approach arbitration and billing disputes, potentially leading to a more standardized approach across the industry. As the healthcare system grapples with the implications of the No Surprises Act, the outcomes of this legal battle will be closely watched by stakeholders on all sides.
Case Studies: Similar Legal Actions in Other States
Elevance’s legal action is not an isolated incident; similar cases have emerged in other states as insurers and providers navigate the complexities of the No Surprises Act. Examining these case studies can provide valuable insights into the broader implications of such legal actions.
One notable case occurred in California, where a major insurer filed a lawsuit against several hospitals for alleged violations of the No Surprises Act. The insurer claimed that the hospitals were engaging in unfair billing practices, leading to inflated costs for patients. The case resulted in a settlement that required the hospitals to revise their billing practices and implement more transparent pricing structures.
Another example can be found in Texas, where a group of providers challenged the arbitration process established by the No Surprises Act. The providers argued that the process favored insurers and did not adequately account for the costs of delivering care. This case highlighted the ongoing tensions between insurers and providers and underscored the need for a balanced approach to arbitration.
These case studies illustrate the challenges faced by both insurers and providers in adapting to the No Surprises Act. They also highlight the potential for legal action to drive changes in billing practices and negotiation strategies, ultimately benefiting patients by promoting transparency and fairness in healthcare costs.
The Future of Healthcare Arbitration
The legal action taken by Elevance against Georgia providers raises important questions about the future of healthcare arbitration in the United States. As the No Surprises Act continues to evolve, stakeholders must consider how to create a fair and effective arbitration process that protects patients while ensuring that providers are adequately compensated for their services.
Key considerations for the future of healthcare arbitration include:
- Standardization of Billing Practices: Establishing standardized billing practices across the industry could help reduce confusion and disputes related to arbitration, promoting a more equitable system for all parties involved.
- Enhanced Transparency: Increasing transparency in billing and negotiation processes can empower patients to make informed decisions about their healthcare and reduce the likelihood of surprise bills.
- Collaboration Between Insurers and Providers: Encouraging collaboration between insurers and providers can lead to more effective negotiation strategies and a better understanding of each party’s needs and concerns.
As the healthcare landscape continues to evolve, it is crucial for stakeholders to work together to address the challenges posed by surprise billing and arbitration. The outcomes of Elevance’s legal action may serve as a catalyst for change, prompting a reevaluation of how healthcare costs are managed and negotiated in the United States.
Conclusion
The legal action taken by Elevance Health against Georgia providers over No Surprises arbitration allegations underscores the complexities of implementing the No Surprises Act and the ongoing challenges faced by insurers and providers in the healthcare landscape. As the case unfolds, it has the potential to set important precedents for how similar disputes are handled in the future.
Key takeaways from this article include:
- The No Surprises Act aims to protect patients from unexpected medical bills, but its implementation has led to disputes between insurers and providers.
- Elevance’s allegations against Georgia providers highlight concerns about billing practices and the arbitration process established by the Act.
- The legal action could have significant implications for healthcare providers, potentially leading to changes in billing practices and negotiation strategies.
- Similar legal actions in other states demonstrate that this issue is not isolated and may drive broader changes in the healthcare industry.
- The future of healthcare arbitration will depend on collaboration between insurers and providers, enhanced transparency, and standardized billing practices.
As stakeholders continue to navigate the complexities of healthcare billing and arbitration, it is essential to prioritize patient protection and promote a fair and equitable system for all parties involved. The outcomes of Elevance’s legal action will be closely monitored, as they may shape the future of healthcare arbitration in the United States.