Boosting Emergency Response Through Mobile Health Units
In an era where rapid response to health emergencies is crucial, mobile health units (MHUs) have emerged as a transformative solution. These units are designed to deliver healthcare services directly to communities, especially in times of crisis. This article explores the multifaceted role of mobile health units in enhancing emergency response, examining their operational frameworks, benefits, challenges, and real-world applications.
1. Understanding Mobile Health Units
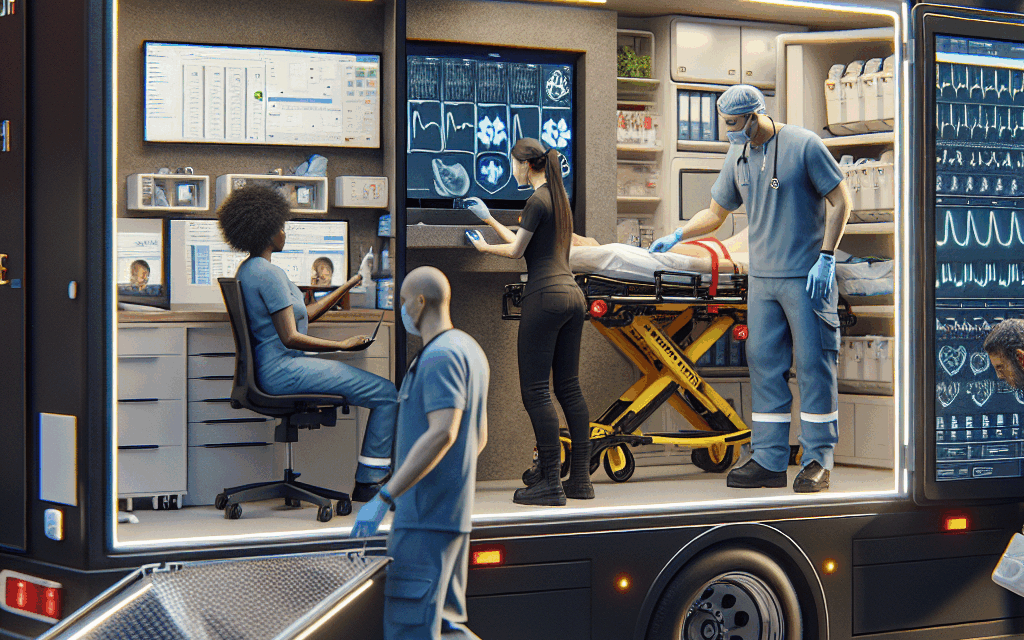
Mobile health units are portable healthcare facilities equipped to provide a range of medical services. They can be deployed in various settings, including urban areas, rural communities, and disaster-stricken regions. The flexibility and adaptability of MHUs make them invaluable in emergency situations.
Typically, these units are outfitted with essential medical equipment, supplies, and personnel capable of delivering immediate care. They can serve multiple functions, including:
- Providing primary care services
- Administering vaccinations
- Conducting health screenings
- Offering mental health support
- Facilitating health education and outreach
MHUs can be operated by various entities, including government health departments, non-profit organizations, and private healthcare providers. Their deployment is often strategic, targeting areas with limited access to healthcare or those affected by emergencies such as natural disasters, pandemics, or civil unrest.
2. The Role of Mobile Health Units in Emergency Situations
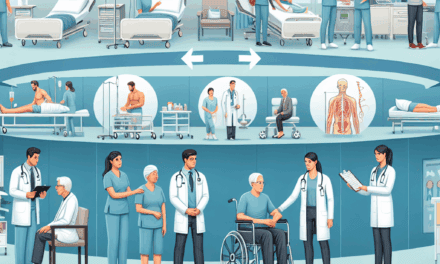
Mobile health units play a critical role in emergency response by bridging the gap between healthcare providers and communities in need. Their ability to reach underserved populations quickly can significantly impact health outcomes during crises.
During natural disasters, for instance, MHUs can be deployed to provide immediate medical care to affected individuals. They can set up in strategic locations, such as shelters or community centers, ensuring that healthcare services are accessible to those who need them most. A notable example is the response to Hurricane Katrina in 2005, where mobile clinics provided essential services to displaced populations.
In addition to disaster response, MHUs are instrumental during public health emergencies, such as the COVID-19 pandemic. They have been utilized for:
- Testing and screening for COVID-19
- Administering vaccines
- Providing education on preventive measures
For example, in the United States, various health departments deployed mobile units to administer COVID-19 vaccines in underserved communities, significantly increasing vaccination rates in areas that traditionally faced barriers to healthcare access.
3. Benefits of Mobile Health Units
The advantages of mobile health units are numerous, making them a vital component of emergency response strategies. Some of the key benefits include:
- Accessibility: MHUs can reach remote or underserved areas where traditional healthcare facilities may be lacking.
- Flexibility: They can be quickly deployed and adapted to meet the specific needs of a community during an emergency.
- Cost-effectiveness: Operating mobile units can be more economical than establishing permanent healthcare facilities in certain situations.
- Community engagement: MHUs often involve local healthcare workers, fostering trust and improving health literacy within communities.
- Rapid response: The ability to mobilize quickly can save lives during critical situations.
For instance, during the Ebola outbreak in West Africa, mobile health units were crucial in providing care and education to affected communities. They helped to contain the spread of the virus by offering testing, treatment, and preventive education directly where it was needed.
4. Challenges Facing Mobile Health Units
Despite their many benefits, mobile health units face several challenges that can hinder their effectiveness. Understanding these challenges is essential for improving their deployment and operation.
- Funding and resources: Securing adequate funding for mobile health units can be a significant barrier. Many units rely on grants and donations, which can be unpredictable.
- Logistical issues: Transporting equipment and personnel to remote locations can be complicated, especially in disaster scenarios where infrastructure may be damaged.
- Regulatory hurdles: Navigating the regulatory landscape can be challenging, particularly when operating across state or national borders.
- Staffing shortages: Recruiting and retaining qualified healthcare professionals for mobile units can be difficult, especially during high-demand periods.
- Community acceptance: Gaining the trust of local populations is crucial. If communities are skeptical of mobile health units, their effectiveness can be severely limited.
Addressing these challenges requires collaboration among various stakeholders, including government agencies, non-profits, and community organizations. For example, partnerships can help secure funding and resources while also fostering community trust through local engagement.
5. Case Studies: Successful Implementation of Mobile Health Units
Examining successful case studies can provide valuable insights into the effective implementation of mobile health units. These examples highlight best practices and innovative approaches that can be replicated in other contexts.
One notable case is the use of mobile health units in the aftermath of the 2010 earthquake in Haiti. The earthquake devastated the country’s healthcare infrastructure, leaving many without access to essential services. In response, various organizations deployed mobile clinics to provide immediate care, including:
- Emergency medical treatment
- Maternal and child health services
- Vaccination campaigns
These mobile units played a crucial role in reducing morbidity and mortality rates in the affected population. They also helped to rebuild trust in the healthcare system by involving local healthcare workers and community leaders in their operations.
Another successful example is the use of mobile health units in rural India. The government, in collaboration with NGOs, launched a program to deploy mobile clinics to underserved villages. These units provided a range of services, including:
- Primary healthcare
- Preventive care and health education
- Referral services for more complex cases
The program significantly improved health outcomes in these communities, demonstrating the effectiveness of mobile health units in addressing healthcare disparities.
Conclusion
Mobile health units represent a powerful tool for enhancing emergency response and improving healthcare access in underserved communities. Their ability to provide immediate care, engage with local populations, and adapt to various situations makes them invaluable in times of crisis.
While challenges remain, the benefits of mobile health units are clear. By learning from successful case studies and addressing logistical and regulatory hurdles, stakeholders can optimize the deployment of these units to ensure that healthcare reaches those who need it most.
As we continue to face global health challenges, investing in mobile health units will be essential for building resilient healthcare systems capable of responding effectively to emergencies. The future of emergency response lies in our ability to innovate and adapt, and mobile health units are at the forefront of this transformation.