Unlocking Success in Healthcare Bundled Payments
The healthcare industry is undergoing a significant transformation, with a growing emphasis on value-based care. One of the most promising models in this shift is the bundled payment system, which aims to improve patient outcomes while controlling costs. This article delves into the intricacies of bundled payments, exploring their structure, benefits, challenges, and strategies for successful implementation. By understanding these elements, healthcare providers can unlock the potential of bundled payments to enhance care delivery and financial performance.
Understanding Bundled Payments
Bundled payments represent a payment model that consolidates multiple services related to a specific treatment or condition into a single payment. This approach contrasts with traditional fee-for-service models, where providers are reimbursed for each individual service rendered. Bundled payments incentivize providers to deliver high-quality care efficiently, as they must manage costs within the fixed payment amount.
Typically, bundled payments cover a defined episode of care, which may include:
- Pre-operative assessments
- Inpatient hospital stays
- Post-acute care
- Follow-up visits
For example, a bundled payment for hip replacement surgery might encompass all services from the initial consultation through rehabilitation. This model encourages collaboration among healthcare providers, as they must work together to ensure that patients receive comprehensive care while staying within budget.
The Benefits of Bundled Payments
Bundled payments offer numerous advantages for healthcare providers, patients, and payers alike. Understanding these benefits is crucial for stakeholders considering the adoption of this payment model.
1. Cost Control and Predictability
One of the primary benefits of bundled payments is the potential for cost control. By consolidating payments for an entire episode of care, providers can better predict expenses and manage resources more effectively. This predictability can lead to improved financial planning and reduced administrative burdens associated with billing multiple services.
2. Enhanced Care Coordination
Bundled payments promote collaboration among healthcare providers, fostering a team-based approach to patient care. This coordination can lead to improved patient outcomes, as providers work together to ensure that all aspects of a patient’s treatment are addressed. For instance, a study published in the Journal of the American Medical Association found that hospitals participating in bundled payment programs for joint replacement surgeries experienced a 20% reduction in readmission rates.
3. Improved Patient Experience
Patients benefit from bundled payments through a more streamlined and cohesive care experience. With a single payment covering all services, patients are less likely to encounter unexpected costs or billing confusion. Additionally, the focus on value-based care encourages providers to prioritize patient satisfaction and engagement, leading to better overall experiences.
4. Incentives for Quality Improvement
Bundled payments incentivize providers to focus on quality rather than quantity. Since reimbursement is tied to patient outcomes, providers are motivated to implement best practices and evidence-based care protocols. This shift can lead to improved clinical outcomes and reduced complications, ultimately benefiting both patients and providers.
5. Alignment with Value-Based Care Initiatives
As the healthcare landscape continues to evolve towards value-based care, bundled payments align with broader industry trends. By adopting this model, providers can position themselves as leaders in quality care delivery, enhancing their reputation and competitiveness in the market.
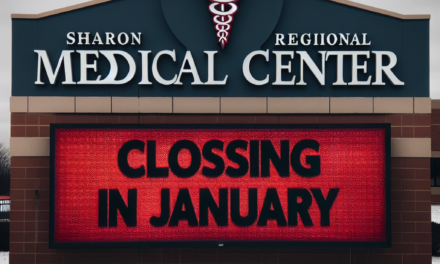
Challenges in Implementing Bundled Payments
While bundled payments offer significant advantages, they also present challenges that healthcare organizations must navigate to achieve success. Understanding these obstacles is essential for effective implementation.
1. Data Management and Analytics
Successful bundled payment programs rely on robust data management and analytics capabilities. Providers must track a wide range of metrics, including costs, patient outcomes, and satisfaction levels. This requires investment in technology and skilled personnel to analyze data effectively. Many organizations struggle with data silos and lack the necessary infrastructure to support comprehensive analytics.
2. Provider Engagement and Buy-In
Engaging providers in the transition to bundled payments can be challenging. Some clinicians may be resistant to change, particularly if they perceive bundled payments as a threat to their income or autonomy. To overcome this resistance, organizations must communicate the benefits of bundled payments clearly and involve providers in the design and implementation process.
3. Risk Management
Bundled payments shift financial risk from payers to providers, which can be daunting for some organizations. Providers must be prepared to manage this risk effectively, which may involve investing in care management programs and developing strategies to address potential complications. Organizations must also consider how to handle patients with complex needs who may require additional resources.
4. Regulatory and Compliance Issues
The regulatory landscape surrounding bundled payments can be complex and ever-changing. Providers must stay informed about relevant regulations and ensure compliance with federal and state guidelines. This may require ongoing education and training for staff, as well as collaboration with legal and compliance experts.
5. Financial Incentives and Payment Models
Designing effective financial incentives within bundled payment models can be challenging. Organizations must strike a balance between incentivizing cost savings and ensuring that quality of care is not compromised. Additionally, determining the appropriate payment amount for each episode of care requires careful analysis and consideration of various factors, including historical costs and patient demographics.
Strategies for Successful Implementation
To unlock the full potential of bundled payments, healthcare organizations must adopt strategic approaches to implementation. Here are several key strategies that can facilitate success:
1. Establish a Multidisciplinary Team
Creating a multidisciplinary team that includes representatives from various departments—such as finance, clinical operations, and quality improvement—can enhance collaboration and ensure that all perspectives are considered during the implementation process. This team can work together to develop protocols, monitor performance, and address challenges as they arise.
2. Invest in Technology and Data Analytics
Investing in technology that supports data collection and analysis is crucial for the success of bundled payment programs. Organizations should consider implementing electronic health records (EHR) systems that facilitate data sharing and interoperability. Additionally, advanced analytics tools can help providers track performance metrics and identify areas for improvement.
3. Engage Providers Early and Often
Engaging providers from the outset is essential for fostering buy-in and ensuring successful implementation. Organizations should involve clinicians in the design of bundled payment programs and provide ongoing education about the benefits and mechanics of the model. Regular communication and feedback loops can help address concerns and build trust among providers.
4. Develop Care Pathways and Protocols
Establishing standardized care pathways and protocols can help ensure consistency in care delivery and improve patient outcomes. Organizations should leverage evidence-based guidelines to develop these pathways, which can serve as a roadmap for providers throughout the episode of care. Regularly reviewing and updating these protocols based on performance data can further enhance their effectiveness.
5. Monitor Performance and Adjust Strategies
Continuous monitoring of performance metrics is essential for identifying areas for improvement and ensuring that bundled payment programs are achieving their intended goals. Organizations should establish key performance indicators (KPIs) related to cost, quality, and patient satisfaction, and regularly review these metrics to inform decision-making. If certain strategies are not yielding the desired results, organizations should be prepared to adjust their approach accordingly.
Case Studies: Successful Bundled Payment Programs
Examining real-world examples of successful bundled payment programs can provide valuable insights into best practices and strategies for implementation. Here are a few notable case studies:
1. The Comprehensive Care for Joint Replacement (CJR) Model
Launched by the Centers for Medicare & Medicaid Services (CMS) in 2016, the CJR model aims to improve care for Medicare beneficiaries undergoing hip and knee replacement surgeries. Under this program, hospitals receive a bundled payment for all services related to the procedure, incentivizing them to coordinate care and reduce costs.
Early results from the CJR model have been promising, with participating hospitals reporting a 20% reduction in Medicare spending for joint replacement surgeries. Additionally, patient satisfaction scores have improved, indicating that the focus on value-based care is resonating with patients.
2. The Bundled Payments for Care Improvement (BPCI) Initiative
The BPCI initiative, also launched by CMS, allows providers to participate in bundled payment arrangements for various clinical episodes. This program has seen widespread adoption across the country, with thousands of providers participating in different clinical areas.
One notable success story comes from a hospital system in Michigan that implemented BPCI for cardiac care. By focusing on care coordination and patient education, the hospital was able to reduce readmission rates by 15% and achieve significant cost savings while maintaining high-quality care.
3. Geisinger Health System’s ProvenCare Program
Geisinger Health System in Pennsylvania has been a pioneer in bundled payments through its ProvenCare program. This initiative offers a fixed price for specific procedures, such as coronary artery bypass grafting, which includes all pre-operative, operative, and post-operative care.
Geisinger’s approach emphasizes evidence-based protocols and patient engagement, resulting in improved outcomes and reduced costs. The program has demonstrated a 20% reduction in complications and a 10% decrease in overall costs compared to traditional fee-for-service models.
4. The Cleveland Clinic’s Bundled Payment Program
The Cleveland Clinic has successfully implemented bundled payment arrangements for various surgical procedures, including orthopedic and cardiovascular surgeries. By focusing on care coordination and patient education, the clinic has achieved significant improvements in patient outcomes and cost savings.
For instance, the Cleveland Clinic reported a 30% reduction in readmission rates for hip replacement surgeries under its bundled payment program. This success can be attributed to the clinic’s emphasis on multidisciplinary care teams and standardized care pathways.
5. The University of Virginia Health System’s Bundled Payment Initiative
The University of Virginia Health System has embraced bundled payments for several clinical episodes, including hip and knee replacements. By implementing a comprehensive care management program, the health system has successfully reduced costs while improving patient satisfaction.
Through its bundled payment initiative, the University of Virginia Health System achieved a 25% reduction in overall costs for joint replacement surgeries, along with improved patient outcomes and satisfaction scores. This success highlights the importance of care coordination and patient engagement in bundled payment models.
Conclusion
Bundled payments represent a transformative approach to healthcare reimbursement, aligning financial incentives with the delivery of high-quality, coordinated care. By understanding the structure, benefits, challenges, and strategies for successful implementation, healthcare organizations can unlock the potential of bundled payments to enhance patient outcomes and financial performance.
As the healthcare landscape continues to evolve towards value-based care, embracing bundled payments will be essential for providers seeking to thrive in this new environment. By fostering collaboration, investing in technology, and prioritizing patient engagement, organizations can navigate the complexities of bundled payments and ultimately improve the quality of care they deliver.
In summary, the journey towards successful bundled payments requires a commitment to continuous improvement, data-driven decision-making, and a focus on patient-centered care. By leveraging the insights and strategies outlined in this article, healthcare organizations can position themselves for success in the era of value-based care.