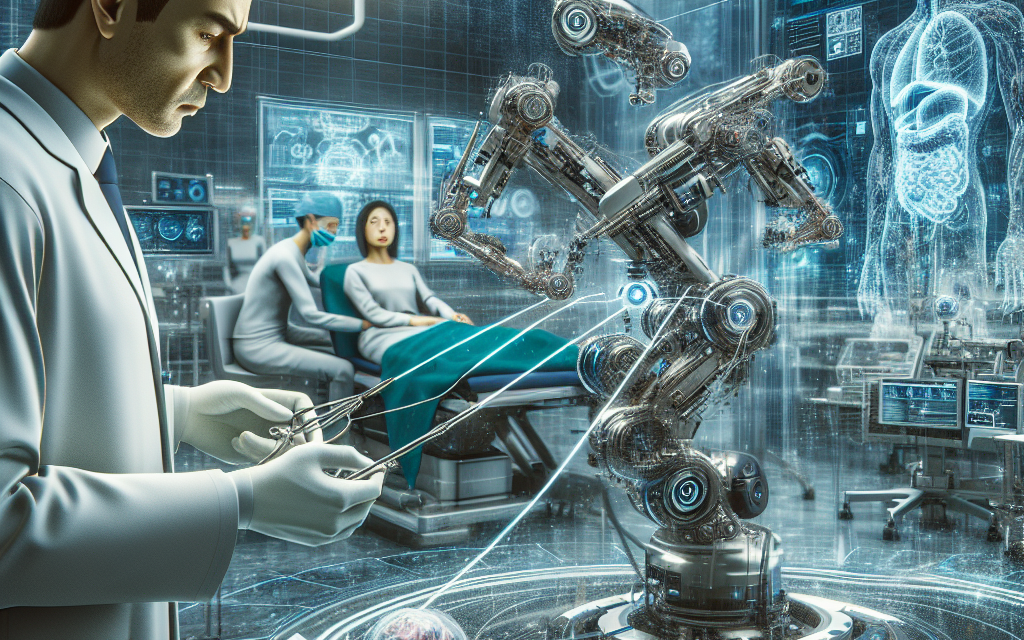
Advancements in Robotic Telesurgery: What’s Next?
Robotic telesurgery represents a significant leap forward in the field of medicine, combining the precision of robotic systems with the flexibility of remote operations. As technology continues to evolve, the potential for robotic telesurgery to transform surgical practices is immense. This article explores the latest advancements in robotic telesurgery, the challenges faced, and what the future may hold for this innovative field.
1. The Evolution of Robotic Telesurgery
Robotic telesurgery has its roots in the early developments of robotic systems in the 1980s. The first significant milestone was the introduction of the da Vinci Surgical System in 2000, which allowed surgeons to perform minimally invasive surgeries with enhanced precision. This system set the stage for further advancements in robotic telesurgery.
Over the years, several key developments have shaped the landscape of robotic telesurgery:
- Enhanced Visualization: Modern robotic systems are equipped with high-definition cameras and 3D visualization capabilities, allowing surgeons to see the surgical site in greater detail.
- Improved Dexterity: Robotic arms can mimic the movements of a surgeon’s hands with greater precision, enabling complex maneuvers that would be difficult or impossible with traditional methods.
- Telecommunication Advances: The rise of high-speed internet and low-latency communication has made it feasible for surgeons to operate remotely, even from thousands of miles away.
- AI Integration: Artificial intelligence is increasingly being integrated into robotic systems, providing real-time data analysis and decision support during surgeries.
- Training and Simulation: Advanced simulation technologies are being developed to train surgeons in robotic telesurgery, enhancing their skills and confidence before performing actual procedures.
These advancements have not only improved surgical outcomes but have also expanded the possibilities for remote surgeries, particularly in underserved areas where access to specialized surgical care is limited.
2. Current Applications of Robotic Telesurgery
Robotic telesurgery is currently being utilized in various medical fields, demonstrating its versatility and effectiveness. Some of the most notable applications include:
- Urology: Robotic telesurgery is widely used in urological procedures, such as prostatectomies. The da Vinci system has become a standard tool for these surgeries, allowing for precise removal of the prostate with minimal damage to surrounding tissues.
- Gynecology: In gynecological surgeries, robotic systems facilitate procedures like hysterectomies and myomectomies. The precision of robotic arms helps reduce recovery times and complications.
- Cardiac Surgery: Robotic telesurgery is making inroads into cardiac procedures, including valve repairs and coronary artery bypass surgeries. Surgeons can perform these complex operations with enhanced control and visualization.
- Orthopedics: In orthopedic surgery, robotic systems assist in joint replacements and other procedures, improving alignment and reducing recovery times.
- Telemedicine Integration: The integration of robotic telesurgery with telemedicine platforms allows for remote consultations and pre-operative assessments, streamlining the surgical process.
These applications highlight the growing acceptance of robotic telesurgery in various specialties, showcasing its potential to improve patient outcomes and expand access to surgical care.
3. Challenges and Limitations of Robotic Telesurgery
Despite its many advantages, robotic telesurgery faces several challenges and limitations that must be addressed for its widespread adoption:
- High Costs: The initial investment in robotic surgical systems is substantial, often exceeding millions of dollars. This can be a barrier for many hospitals, particularly in developing regions.
- Technical Limitations: While robotic systems have advanced significantly, they still face limitations in terms of haptic feedback, which can affect a surgeon’s ability to gauge tissue resistance during procedures.
- Training Requirements: Surgeons require extensive training to operate robotic systems effectively. This training can be time-consuming and costly, limiting the number of qualified practitioners.
- Regulatory Hurdles: The regulatory landscape for robotic telesurgery is complex, with varying requirements across different countries. This can slow down the adoption of new technologies.
- Patient Acceptance: Some patients may be hesitant to undergo robotic telesurgery due to concerns about the technology or the lack of a physical presence of the surgeon during the procedure.
Addressing these challenges will be crucial for the future of robotic telesurgery. Innovations in cost-effective technologies, improved training programs, and enhanced regulatory frameworks will play a significant role in overcoming these barriers.
4. Future Trends in Robotic Telesurgery
The future of robotic telesurgery is promising, with several trends expected to shape its development in the coming years:
- AI and Machine Learning: The integration of AI and machine learning will enhance robotic systems’ capabilities, allowing for better decision-making and predictive analytics during surgeries.
- Miniaturization: Advances in technology may lead to the development of smaller, more portable robotic systems that can be used in a wider range of settings, including remote and rural areas.
- Telepresence Surgery: The concept of telepresence surgery, where surgeons can operate remotely while feeling as if they are physically present, is gaining traction. This could revolutionize how surgeries are performed across the globe.
- Collaborative Robotics: Future robotic systems may incorporate collaborative features, allowing multiple surgeons to work together on a single procedure, regardless of their physical location.
- Patient-Centric Designs: As patient experience becomes a priority, future robotic systems may be designed with a focus on enhancing patient comfort and outcomes, incorporating feedback from patients and healthcare providers.
These trends indicate a shift towards more sophisticated, accessible, and patient-friendly robotic telesurgery solutions, paving the way for a new era in surgical care.
5. Case Studies and Success Stories
Several case studies illustrate the successful implementation of robotic telesurgery and its impact on patient care:
- The First Remote Surgery: In 2001, a team of surgeons in New York performed the first remote surgery using the da Vinci system on a patient in France. This groundbreaking procedure demonstrated the feasibility of robotic telesurgery across long distances.
- Urology Success: A study published in the Journal of Urology highlighted the outcomes of robotic-assisted prostatectomies performed remotely. The results showed reduced blood loss and shorter hospital stays compared to traditional methods.
- Gynecological Innovations: A hospital in India implemented robotic telesurgery for hysterectomies, resulting in a 30% reduction in recovery time and a significant decrease in post-operative complications.
- Cardiac Surgery Breakthroughs: A leading cardiac center in the United States successfully performed remote valve repairs using robotic telesurgery, showcasing the potential for complex cardiac procedures to be conducted from afar.
- Global Outreach Programs: Various organizations are using robotic telesurgery to provide surgical care in underserved regions. For example, a program in Africa has successfully utilized robotic systems to perform life-saving surgeries that would otherwise be unavailable.
These case studies highlight the transformative potential of robotic telesurgery, demonstrating its ability to improve surgical outcomes and expand access to care in diverse settings.
Conclusion
Robotic telesurgery is at the forefront of medical innovation, offering unprecedented opportunities to enhance surgical precision, improve patient outcomes, and expand access to care. While challenges remain, the advancements in technology, training, and integration with telemedicine are paving the way for a future where robotic telesurgery becomes a standard practice in hospitals worldwide.
As we look ahead, the potential for AI integration, miniaturization of robotic systems, and collaborative surgical approaches will further revolutionize the field. By addressing the current limitations and embracing these trends, the medical community can harness the full potential of robotic telesurgery, ultimately transforming the landscape of surgical care for patients around the globe.