Understanding Gut Health’s Impact on Diabetes Management
Diabetes is a chronic condition that affects millions of people worldwide, characterized by high blood sugar levels due to the body’s inability to produce or effectively use insulin. Recent research has highlighted the significant role of gut health in managing diabetes, suggesting that the gut microbiome—the community of microorganisms residing in the digestive tract—can influence insulin sensitivity, inflammation, and overall metabolic health. This article delves into the intricate relationship between gut health and diabetes management, exploring five key subtopics: the gut microbiome and its role in diabetes, the impact of diet on gut health, the connection between inflammation and diabetes, the potential of probiotics and prebiotics, and future directions in gut health research for diabetes management.
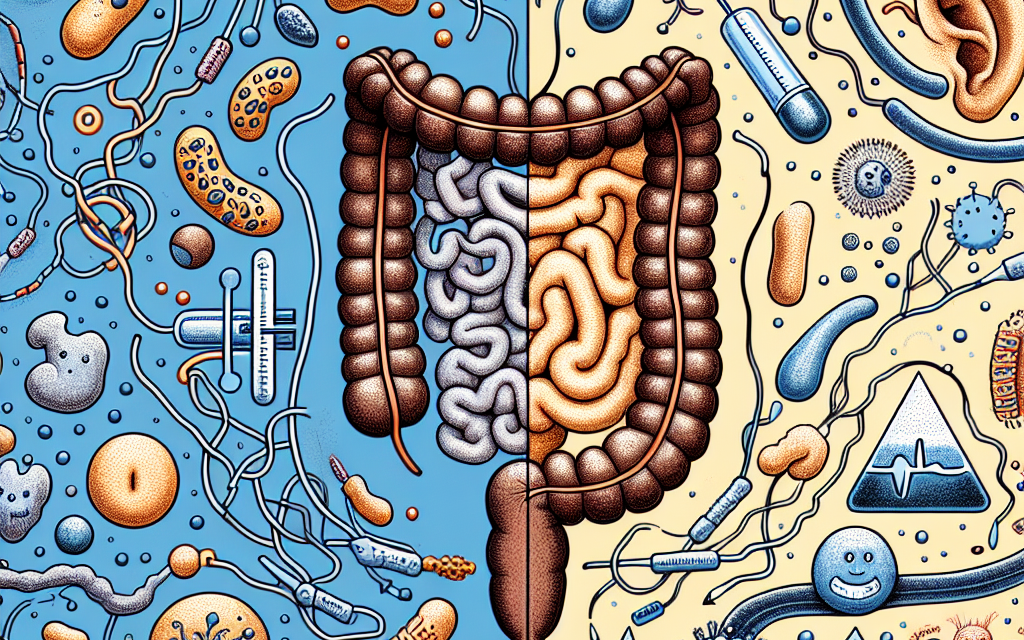
The Gut Microbiome and Its Role in Diabetes
The gut microbiome consists of trillions of bacteria, viruses, fungi, and other microorganisms that play a crucial role in digestion, metabolism, and immune function. Recent studies have shown that the composition and diversity of the gut microbiome can significantly impact glucose metabolism and insulin sensitivity, which are critical factors in diabetes management.
Research indicates that individuals with type 2 diabetes often have a less diverse gut microbiome compared to healthy individuals. A study published in the journal Nature found that specific bacterial species, such as Prevotella and Faecalibacterium, are more abundant in healthy individuals, while those with diabetes tend to have higher levels of Escherichia coli and other harmful bacteria. This imbalance, known as dysbiosis, can lead to increased inflammation and insulin resistance.
Moreover, the gut microbiome influences the production of short-chain fatty acids (SCFAs), which are metabolites produced when gut bacteria ferment dietary fibers. SCFAs, such as butyrate, have been shown to improve insulin sensitivity and reduce inflammation. A study published in Diabetes Care demonstrated that higher levels of SCFAs in the gut were associated with better glycemic control in individuals with type 2 diabetes.
In addition to SCFAs, the gut microbiome also plays a role in the regulation of hormones involved in glucose metabolism, such as glucagon-like peptide-1 (GLP-1). GLP-1 is an incretin hormone that enhances insulin secretion in response to meals and promotes satiety. Research has shown that certain gut bacteria can stimulate the production of GLP-1, thereby improving blood sugar control.
Overall, maintaining a healthy gut microbiome is essential for effective diabetes management. Strategies to promote gut health include dietary modifications, such as increasing fiber intake, consuming fermented foods, and avoiding excessive use of antibiotics, which can disrupt the delicate balance of gut bacteria.
The Impact of Diet on Gut Health
Diet plays a pivotal role in shaping the gut microbiome and, consequently, in managing diabetes. A diet rich in fiber, whole grains, fruits, vegetables, and fermented foods can promote a diverse and healthy gut microbiome, while a diet high in processed foods, sugars, and unhealthy fats can lead to dysbiosis.
Fiber is particularly important for gut health, as it serves as a food source for beneficial gut bacteria. Soluble fiber, found in foods like oats, beans, and fruits, can help regulate blood sugar levels by slowing down the absorption of glucose. A study published in the American Journal of Clinical Nutrition found that individuals with type 2 diabetes who consumed a high-fiber diet experienced significant improvements in glycemic control and insulin sensitivity.
Fermented foods, such as yogurt, kefir, sauerkraut, and kimchi, are also beneficial for gut health. These foods contain live probiotics, which can help restore the balance of gut bacteria. A systematic review in the journal Nutrition Reviews concluded that regular consumption of fermented foods is associated with improved metabolic health and reduced risk of type 2 diabetes.
On the other hand, diets high in added sugars and unhealthy fats can negatively impact gut health. Processed foods often lack the nutrients and fiber necessary for maintaining a healthy microbiome. A study published in Cell Metabolism found that a diet high in sugar and fat led to an increase in harmful bacteria and a decrease in beneficial bacteria, contributing to insulin resistance and inflammation.
To optimize gut health and support diabetes management, individuals should focus on the following dietary strategies:
- Increase fiber intake by incorporating whole grains, legumes, fruits, and vegetables into meals.
- Include fermented foods in the diet to promote the growth of beneficial gut bacteria.
- Avoid excessive consumption of processed foods, added sugars, and unhealthy fats.
- Stay hydrated, as water is essential for digestion and overall gut health.
- Consider a Mediterranean-style diet, which emphasizes whole foods, healthy fats, and lean proteins.
The Connection Between Inflammation and Diabetes
Chronic inflammation is a key factor in the development and progression of type 2 diabetes. The gut microbiome plays a significant role in regulating inflammation, and an imbalance in gut bacteria can lead to increased levels of inflammatory markers in the body.
When the gut microbiome is disrupted, it can result in a condition known as “leaky gut,” where the intestinal barrier becomes permeable, allowing harmful substances to enter the bloodstream. This triggers an immune response, leading to chronic inflammation. Research has shown that individuals with type 2 diabetes often have elevated levels of inflammatory markers, such as C-reactive protein (CRP) and interleukin-6 (IL-6).
Inflammation can impair insulin signaling, leading to insulin resistance—a hallmark of type 2 diabetes. A study published in Diabetes found that higher levels of inflammatory markers were associated with a greater risk of developing insulin resistance and type 2 diabetes.
Moreover, the gut microbiome influences the production of pro-inflammatory cytokines, which can further exacerbate insulin resistance. Certain bacterial species, such as Escherichia coli, have been linked to increased inflammation, while others, like Faecalibacterium prausnitzii, are known for their anti-inflammatory properties.
To mitigate inflammation and support diabetes management, individuals can adopt the following strategies:
- Incorporate anti-inflammatory foods into the diet, such as fatty fish, nuts, seeds, fruits, and vegetables.
- Engage in regular physical activity, which has been shown to reduce inflammation and improve insulin sensitivity.
- Manage stress through mindfulness practices, yoga, or meditation, as chronic stress can contribute to inflammation.
- Prioritize sleep, as poor sleep quality is associated with increased inflammation and insulin resistance.
- Consider supplements, such as omega-3 fatty acids or curcumin, which have anti-inflammatory properties.
The Potential of Probiotics and Prebiotics
Probiotics and prebiotics are two components that can significantly influence gut health and, consequently, diabetes management. Probiotics are live microorganisms that confer health benefits when consumed in adequate amounts, while prebiotics are non-digestible food components that promote the growth of beneficial gut bacteria.
Research has shown that probiotics can improve glycemic control and insulin sensitivity in individuals with type 2 diabetes. A meta-analysis published in Diabetes Care found that probiotic supplementation led to significant reductions in fasting blood glucose and HbA1c levels. Specific strains, such as Lactobacillus and Bifidobacterium, have been particularly effective in improving metabolic health.
Prebiotics, on the other hand, serve as food for beneficial gut bacteria, promoting their growth and activity. Foods rich in prebiotics include garlic, onions, leeks, asparagus, bananas, and whole grains. A study published in the journal Nutrition found that prebiotic supplementation improved insulin sensitivity and reduced body weight in individuals with type 2 diabetes.
Combining probiotics and prebiotics—known as synbiotics—may offer even greater benefits for gut health and diabetes management. A study published in Frontiers in Nutrition demonstrated that synbiotic supplementation improved glycemic control and reduced inflammation in individuals with type 2 diabetes.
To incorporate probiotics and prebiotics into the diet, individuals can:
- Consume fermented foods regularly, such as yogurt, kefir, sauerkraut, and kimchi.
- Include prebiotic-rich foods in meals, such as garlic, onions, and whole grains.
- Consider probiotic supplements, particularly those containing specific strains known to benefit metabolic health.
- Experiment with synbiotic products that combine both probiotics and prebiotics for enhanced effects.
Future Directions in Gut Health Research for Diabetes Management
The field of gut health research is rapidly evolving, with new studies continually uncovering the complex relationship between the gut microbiome and diabetes management. Future research directions may include:
- Personalized Nutrition: As our understanding of the gut microbiome deepens, personalized dietary recommendations based on an individual’s microbiome composition may become a reality. This approach could optimize diabetes management by tailoring interventions to promote a healthy gut microbiome.
- Microbiome Modulation: Researchers are exploring various methods to modulate the gut microbiome, including fecal microbiota transplantation (FMT) and targeted probiotics. These interventions may hold promise for improving metabolic health in individuals with diabetes.
- Longitudinal Studies: Long-term studies examining the effects of dietary interventions on gut health and diabetes outcomes will provide valuable insights into the causal relationships between gut microbiome composition, inflammation, and insulin sensitivity.
- Gut-Brain Axis: The connection between the gut microbiome and the brain—known as the gut-brain axis—may also play a role in diabetes management. Future research may explore how gut health influences appetite regulation, stress response, and overall metabolic health.
- Integration of Technology: Advances in technology, such as microbiome sequencing and wearable devices, may facilitate real-time monitoring of gut health and metabolic parameters, allowing for more effective diabetes management strategies.
Conclusion
Understanding the impact of gut health on diabetes management is crucial for developing effective strategies to control blood sugar levels and improve overall metabolic health. The gut microbiome plays a significant role in regulating insulin sensitivity, inflammation, and hormone production, all of which are critical factors in diabetes management.
By adopting a diet rich in fiber, fermented foods, and prebiotics, individuals can promote a healthy gut microbiome and enhance their diabetes management efforts. Additionally, incorporating probiotics and addressing inflammation through lifestyle changes can further support metabolic health.
As research continues to uncover the intricate relationship between gut health and diabetes, personalized approaches to nutrition and microbiome modulation may offer new avenues for improving outcomes for individuals living with diabetes. Ultimately, prioritizing gut health is not just a trend; it is a vital component of effective diabetes management that can lead to better health outcomes and improved quality of life.