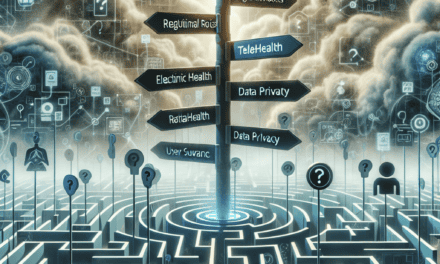
ATA Raises Concerns Over DEA’s Proposed Telehealth Registration Changes
The American Telemedicine Association (ATA) has recently voiced significant concerns regarding the Drug Enforcement Administration’s (DEA) proposed changes to telehealth registration requirements. As telehealth continues to evolve, especially in the wake of the COVID-19 pandemic, the DEA’s regulations play a crucial role in shaping how healthcare providers can prescribe controlled substances remotely. This article delves into the implications of these proposed changes, the concerns raised by the ATA, and the broader context of telehealth in the United States.
Understanding the DEA’s Proposed Changes
The DEA’s proposed changes to telehealth registration are primarily aimed at regulating how healthcare providers can prescribe controlled substances via telemedicine. These changes are part of a broader effort to ensure that prescriptions are issued responsibly and that patients receive safe and effective care. However, the specifics of these proposals have raised eyebrows among healthcare professionals and organizations like the ATA.
One of the key aspects of the proposed changes is the requirement for healthcare providers to undergo a more rigorous registration process before they can prescribe controlled substances through telehealth. This includes:
- In-person evaluations: Providers may be required to conduct in-person evaluations before prescribing controlled substances, which could undermine the convenience and accessibility that telehealth offers.
- Increased documentation: The proposed changes may necessitate more extensive documentation and record-keeping, placing additional burdens on healthcare providers.
- Limitations on prescribing: The DEA may impose stricter limits on the types of medications that can be prescribed via telehealth, particularly for new patients.
These changes are intended to combat the opioid crisis and prevent misuse of controlled substances. However, the ATA argues that they could have unintended consequences that may hinder patient access to necessary medications and disrupt the telehealth landscape.
The ATA’s Concerns: Access to Care
One of the primary concerns raised by the ATA is that the proposed changes could significantly limit patient access to care, particularly for those in rural or underserved areas. Telehealth has been a game-changer for many patients, allowing them to receive care without the need for travel, which can be a barrier for those with limited mobility or transportation options.
Access to care is a critical issue in the United States, where millions of people live in areas designated as Health Professional Shortage Areas (HPSAs). The ATA emphasizes that the proposed in-person evaluation requirement could exacerbate existing disparities in healthcare access. For example:
- Patients in rural areas may have to travel long distances to see a provider in person, which could delay treatment and exacerbate health issues.
- Individuals with disabilities or chronic illnesses may find it challenging to attend in-person appointments, leading to missed opportunities for care.
- Low-income patients may face financial barriers to travel, further limiting their access to necessary medications.
Moreover, the ATA points out that telehealth has been instrumental in providing timely care during the pandemic. Many patients have relied on telehealth services to manage chronic conditions, receive mental health support, and access medications. The proposed changes could disrupt this progress and lead to negative health outcomes for vulnerable populations.
Impact on Mental Health Services
The proposed changes also raise significant concerns regarding mental health services, particularly in the context of prescribing controlled substances such as antidepressants and anti-anxiety medications. The pandemic has led to a surge in mental health issues, with many individuals seeking help through telehealth platforms.
Telehealth has proven to be an effective means of delivering mental health services, allowing patients to connect with providers from the comfort of their homes. However, the requirement for in-person evaluations could hinder access to these essential services. Consider the following points:
- Many individuals seeking mental health support may be reluctant to attend in-person appointments due to stigma or anxiety, making telehealth a more appealing option.
- In-person evaluations may not be feasible for patients who live far from mental health providers, leading to delays in treatment.
- Telehealth has been particularly beneficial for patients with mobility issues or those who require flexible scheduling, which could be compromised by the proposed changes.
Furthermore, the ATA highlights that mental health conditions often require ongoing treatment and medication management. The proposed changes could disrupt continuity of care, forcing patients to navigate complex systems to obtain necessary prescriptions. This could lead to increased rates of medication non-adherence and worsening mental health outcomes.
Administrative Burdens on Healthcare Providers
Another significant concern raised by the ATA is the potential administrative burden that the proposed changes could impose on healthcare providers. The requirement for increased documentation and record-keeping could divert valuable time and resources away from patient care.
Healthcare providers are already facing numerous challenges, including high patient loads, administrative tasks, and the need to stay updated on evolving regulations. The proposed changes could exacerbate these challenges in several ways:
- Providers may need to invest additional time in training and compliance efforts to meet the new registration requirements.
- Increased documentation could lead to longer appointment times, reducing the number of patients providers can see in a day.
- Providers may face financial penalties or legal repercussions if they fail to comply with the new regulations, adding further stress to their practice.
The ATA argues that these administrative burdens could lead to burnout among healthcare providers, ultimately impacting the quality of care that patients receive. In a time when the healthcare system is already strained, adding more layers of bureaucracy could have detrimental effects on both providers and patients.
Potential Solutions and Recommendations
In light of the concerns raised by the ATA, it is essential to explore potential solutions and recommendations that could address the issues associated with the DEA’s proposed changes. The goal should be to strike a balance between ensuring patient safety and maintaining access to care through telehealth.
Some potential solutions include:
- Implementing a hybrid model: Allowing for a combination of in-person and telehealth evaluations could provide flexibility for both patients and providers while ensuring that safety protocols are followed.
- Streamlining documentation requirements: Simplifying the documentation process could reduce administrative burdens on healthcare providers, allowing them to focus more on patient care.
- Enhancing training and resources: Providing healthcare providers with training and resources on telehealth best practices could help them navigate the evolving landscape while ensuring compliance with regulations.
- Engaging stakeholders: Involving healthcare providers, patients, and telehealth organizations in the regulatory process could lead to more informed decisions that consider the needs of all parties involved.
By adopting these solutions, the DEA can work towards creating a regulatory framework that prioritizes patient safety while also promoting access to care through telehealth. Collaboration between regulatory agencies and healthcare stakeholders will be crucial in achieving this balance.
Conclusion: The Future of Telehealth and Regulatory Challenges
The concerns raised by the ATA regarding the DEA’s proposed telehealth registration changes highlight the complex interplay between regulation, patient access, and healthcare delivery. As telehealth continues to play a vital role in the healthcare landscape, it is essential for regulatory agencies to consider the potential impact of their decisions on patients and providers alike.
While the DEA’s intentions to combat substance misuse and ensure patient safety are commendable, the proposed changes could inadvertently create barriers to care for vulnerable populations. The ATA’s advocacy for a more balanced approach underscores the importance of maintaining access to telehealth services, particularly in a post-pandemic world where many patients have come to rely on these services for their healthcare needs.
As stakeholders continue to engage in discussions about the future of telehealth, it is crucial to prioritize solutions that enhance patient access while ensuring safety and compliance. By fostering collaboration and understanding between regulatory agencies and healthcare providers, we can work towards a telehealth landscape that benefits all patients and supports the evolving needs of the healthcare system.