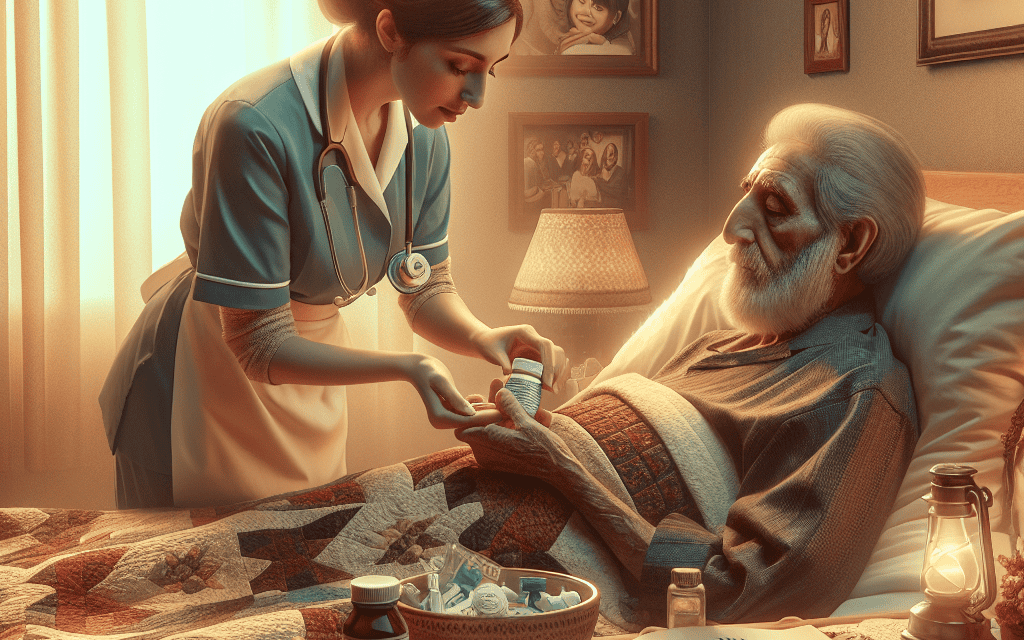
Hospice Home Care: A Vital Support in Terminal Illness Management
As the population ages and the prevalence of chronic illnesses increases, the need for compassionate and effective end-of-life care has never been more critical. Hospice home care has emerged as a vital support system for patients facing terminal illnesses, providing not only medical assistance but also emotional and spiritual support for both patients and their families. This article delves into the multifaceted aspects of hospice home care, exploring its significance, benefits, challenges, and the holistic approach it embodies in terminal illness management.
Understanding Hospice Home Care
Hospice home care is a specialized form of medical care designed for individuals with terminal illnesses who are no longer seeking curative treatment. Instead, the focus shifts to comfort, quality of life, and dignity in the final stages of life. This section will explore the fundamental principles of hospice care, its eligibility criteria, and the interdisciplinary team involved in providing this essential service.
Principles of Hospice Care
At its core, hospice care is grounded in several key principles:
- Patient-Centered Care: Hospice care prioritizes the needs and preferences of the patient, ensuring that care plans are tailored to individual circumstances.
- Holistic Approach: Care extends beyond physical symptoms to address emotional, spiritual, and social needs, recognizing the interconnectedness of these aspects in a patient’s experience.
- Family Involvement: Hospice recognizes the importance of family in the care process, providing support and education to help them cope with the challenges of terminal illness.
- Interdisciplinary Team: A diverse team of healthcare professionals collaborates to provide comprehensive care, including physicians, nurses, social workers, chaplains, and volunteers.
- Focus on Quality of Life: The primary goal is to enhance the quality of life for patients, managing pain and other distressing symptoms while allowing them to live as fully as possible.
Eligibility for Hospice Care
To qualify for hospice care, patients typically must meet specific criteria:
- Terminal Diagnosis: Patients must have a prognosis of six months or less to live, as determined by a physician.
- Decline in Health: There should be a noticeable decline in the patient’s health status, indicating that curative treatments are no longer effective.
- Patient and Family Choice: Patients must choose hospice care over curative treatment, emphasizing the importance of informed decision-making.
The Interdisciplinary Team
The interdisciplinary team in hospice care plays a crucial role in delivering comprehensive support. This team typically includes:
- Physicians: Oversee the medical aspects of care, manage symptoms, and coordinate with other team members.
- Nurses: Provide direct patient care, administer medications, and educate families on care techniques.
- Social Workers: Offer emotional support, assist with practical needs, and help families navigate healthcare systems.
- Chaplains: Address spiritual concerns and provide comfort to patients and families from various faith backgrounds.
- Volunteers: Offer companionship and respite for family caregivers, enhancing the overall support system.
The Benefits of Hospice Home Care
Hospice home care offers numerous benefits that significantly enhance the quality of life for patients and their families. This section will explore these advantages in detail, highlighting how hospice care can transform the end-of-life experience.
Enhanced Quality of Life
One of the most significant benefits of hospice home care is the enhancement of the patient’s quality of life. By focusing on comfort rather than curative measures, hospice care allows patients to:
- Manage Pain Effectively: Hospice teams employ various pain management strategies, including medications and alternative therapies, to alleviate discomfort.
- Maintain Independence: Patients can remain in their familiar surroundings, preserving a sense of autonomy and control over their environment.
- Engage in Meaningful Activities: With symptom management in place, patients can participate in activities they enjoy, fostering a sense of normalcy.
Emotional and Spiritual Support
Hospice care recognizes the emotional and spiritual dimensions of terminal illness. The support provided by the interdisciplinary team can help patients and families navigate complex feelings:
- Emotional Counseling: Social workers and counselors offer emotional support, helping patients and families process grief, fear, and anxiety.
- Spiritual Care: Chaplains provide spiritual guidance, helping patients find peace and meaning in their experiences.
- Family Support: Hospice teams educate families on coping strategies and provide respite care, allowing caregivers to recharge.
Cost-Effectiveness
Hospice home care can also be a cost-effective option for families facing terminal illness. Key financial benefits include:
- Reduced Hospitalization: By managing symptoms at home, patients often experience fewer hospital visits, leading to lower medical expenses.
- Comprehensive Care Packages: Hospice services typically include a range of support services bundled into one package, reducing out-of-pocket costs.
- Insurance Coverage: Many insurance plans, including Medicare, cover hospice care, making it accessible to a broader population.
Support for Family Caregivers
Family caregivers often face immense physical and emotional burdens when caring for a terminally ill loved one. Hospice home care provides essential support to alleviate these challenges:
- Respite Care: Hospice services can offer temporary relief for family caregivers, allowing them to take breaks and recharge.
- Education and Training: Caregivers receive training on how to manage symptoms and provide care, increasing their confidence and competence.
- Emotional Support: Hospice teams provide counseling and support groups for caregivers, helping them cope with the emotional toll of caregiving.
Personalized Care Plans
Hospice home care emphasizes personalized care plans tailored to the unique needs of each patient. This individualized approach ensures that:
- Patient Preferences are Respected: Care plans are developed in collaboration with patients and families, honoring their wishes and values.
- Dynamic Adjustments: Care plans can be adjusted as the patient’s condition changes, ensuring that care remains relevant and effective.
- Comprehensive Assessments: Regular assessments by the interdisciplinary team ensure that all aspects of the patient’s well-being are addressed.
Challenges in Hospice Home Care
While hospice home care offers numerous benefits, it is not without its challenges. This section will explore some of the common obstacles faced by patients, families, and healthcare providers in the hospice care landscape.
Access to Services
Accessing hospice home care can be a significant challenge for many patients and families. Factors influencing access include:
- Geographic Barriers: In rural areas, hospice services may be limited, making it difficult for patients to receive care at home.
- Awareness and Education: Many families are unaware of hospice options or may have misconceptions about what hospice care entails.
- Insurance Limitations: Some insurance plans may not cover hospice services, creating financial barriers for families seeking care.
Emotional Resistance
Patients and families may experience emotional resistance to hospice care, often stemming from cultural beliefs or fear of death. Common issues include:
- Stigma Surrounding Hospice: Some individuals view hospice as a last resort, associating it with giving up on life.
- Fear of Losing Control: Patients may fear that choosing hospice means relinquishing control over their care and treatment options.
- Cultural Beliefs: Cultural attitudes toward death and dying can influence decisions about hospice care, leading to reluctance in seeking services.
Coordination of Care
Effective coordination among healthcare providers is essential for successful hospice home care. Challenges in this area can include:
- Lack of Communication: Poor communication between primary care physicians and hospice teams can lead to fragmented care.
- Transitioning from Curative to Palliative Care: Patients may struggle with the transition from curative treatments to hospice care, leading to confusion and anxiety.
- Inconsistent Care Standards: Variability in hospice care standards can affect the quality of care received by patients.
Family Dynamics
Family dynamics can significantly impact the hospice care experience. Challenges may arise from:
- Conflicting Opinions: Family members may have differing views on the appropriateness of hospice care, leading to tension and conflict.
- Caregiver Burnout: Family caregivers may experience burnout, affecting their ability to provide care and support.
- Grief and Anticipatory Grief: Family members may struggle with anticipatory grief, complicating their emotional responses to the patient’s condition.
Regulatory and Policy Issues
The hospice care landscape is influenced by various regulatory and policy issues that can impact service delivery:
- Reimbursement Challenges: Changes in reimbursement policies can affect the financial viability of hospice providers, potentially limiting access to care.
- Quality Assurance Standards: Ensuring consistent quality of care across hospice providers is essential but can be challenging to regulate effectively.
- Advocacy for Policy Change: Ongoing advocacy is needed to address barriers to hospice care access and improve the overall system.
The Future of Hospice Home Care
The landscape of hospice home care is evolving, driven by advancements in technology, changing demographics, and shifting societal attitudes toward end-of-life care. This section will explore emerging trends and innovations that are shaping the future of hospice care.
Telehealth Integration
The integration of telehealth into hospice home care is revolutionizing how patients receive support. Key benefits include:
- Increased Access: Telehealth allows patients in remote areas to connect with hospice providers, improving access to care.
- Real-Time Monitoring: Healthcare providers can monitor patients’ conditions remotely, enabling timely interventions when needed.
- Enhanced Communication: Telehealth facilitates better communication between patients, families, and healthcare teams, fostering collaboration.
Personalized Medicine
Advancements in personalized medicine are influencing hospice care by allowing for more tailored treatment plans. This includes:
- Genetic Testing: Understanding a patient’s genetic makeup can inform pain management strategies and symptom control.
- Customized Care Plans: Personalized approaches to care can enhance the effectiveness of interventions and improve patient outcomes.
- Patient Engagement: Involving patients in their care decisions fosters a sense of ownership and empowerment.
Community-Based Approaches
Community-based hospice care models are gaining traction, emphasizing collaboration with local organizations and resources. Benefits include:
- Holistic Support: Community partnerships can provide additional resources, such as counseling services and support groups.
- Increased Awareness: Community engagement initiatives can raise awareness about hospice care options and reduce stigma.
- Tailored Services: Community-based models can adapt services to meet the unique needs of diverse populations.
Education and Advocacy
Ongoing education and advocacy efforts are essential for improving hospice care access and quality. Key initiatives include:
- Public Awareness Campaigns: Initiatives aimed at educating the public about hospice care can help dispel myths and encourage informed decision-making.
- Training for Healthcare Providers: Continued education for healthcare professionals can enhance their understanding of hospice care and improve referral practices.
- Policy Advocacy: Engaging in advocacy efforts to influence healthcare policies can lead to improved access and quality of hospice services.
Emphasis on Cultural Competence
As the population becomes increasingly diverse, cultural competence in hospice care is essential. This includes:
- Understanding Cultural Beliefs: Hospice providers must be aware of and respect the cultural beliefs and practices of patients and families.
- Tailoring Communication: Effective communication strategies should be adapted to meet the needs of diverse populations.
- Inclusive Care Models: Developing inclusive care models that address the unique needs of various cultural groups can enhance the hospice experience.
Conclusion
Hospice home care represents a compassionate and holistic approach to managing terminal illness, prioritizing the quality of life for patients and their families. By understanding the principles of hospice care, recognizing its benefits, addressing challenges, and embracing future trends, we can create a more supportive environment for those facing the end of life. As society continues to evolve, it is crucial to advocate for accessible, high-quality hospice services that honor the dignity and wishes of every individual. Ultimately, hospice home care is not just about managing illness; it is about celebrating life, fostering connections, and providing comfort during one of life’s most profound journeys.