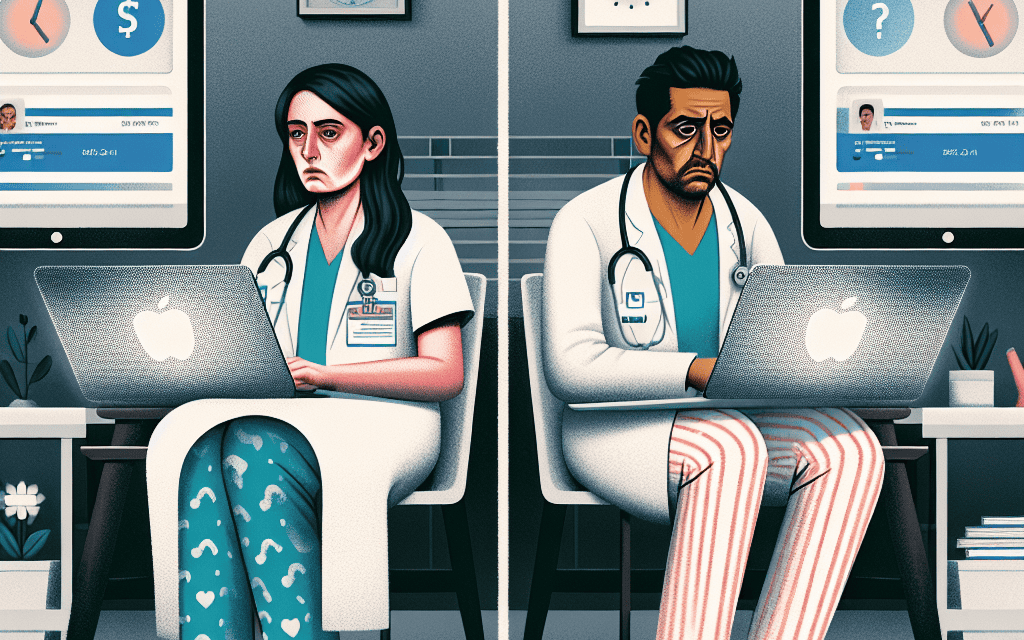
Study Reveals Patient Engagement Tools Fail to Reduce Clinician ‘Pajama Time’
The healthcare landscape is rapidly evolving, with technology playing a pivotal role in enhancing patient engagement and improving clinical outcomes. However, a recent study has shed light on a concerning trend: despite the proliferation of patient engagement tools, clinicians are still spending excessive amounts of time on administrative tasks, often referred to as “pajama time.” This article delves into the findings of the study, exploring the reasons behind this phenomenon, the implications for healthcare providers, and potential solutions to mitigate the issue.
Understanding ‘Pajama Time’
‘Pajama time’ is a colloquial term used to describe the hours healthcare providers spend outside of regular working hours—often late at night or during weekends—completing administrative tasks, such as charting, responding to emails, and managing patient records. This phenomenon has become increasingly prevalent as electronic health records (EHRs) and other digital tools have been integrated into clinical practice.
According to a survey conducted by the American Medical Association (AMA), nearly 50% of physicians reported spending more than 10 hours a week on administrative tasks outside of their regular working hours. This trend not only affects clinician well-being but also has significant implications for patient care and healthcare costs.
The Impact of Pajama Time on Clinicians
The consequences of pajama time extend beyond mere inconvenience. Clinicians who are forced to work late into the night often experience burnout, decreased job satisfaction, and a decline in the quality of patient care. The AMA survey found that 44% of physicians reported feeling burned out, with administrative burdens being a significant contributing factor.
- Burnout and Mental Health: The emotional toll of excessive pajama time can lead to mental health issues, including anxiety and depression. Clinicians may feel overwhelmed by the demands of their job, leading to a vicious cycle of stress and decreased productivity.
- Quality of Care: When clinicians are fatigued from long hours spent on administrative tasks, their ability to provide high-quality care diminishes. Studies have shown that clinician fatigue can lead to increased medical errors, negatively impacting patient safety.
- Work-Life Balance: The blurring of boundaries between work and personal life can strain relationships and lead to dissatisfaction in both professional and personal realms. Clinicians may find it challenging to disconnect from work, leading to a lack of fulfillment outside of their careers.
The Role of Patient Engagement Tools
Patient engagement tools, such as patient portals, telehealth platforms, and mobile health applications, were designed to enhance communication between patients and providers, streamline workflows, and ultimately improve patient outcomes. However, the recent study indicates that these tools have not significantly reduced the amount of pajama time clinicians experience.
Limitations of Current Patient Engagement Tools
While patient engagement tools have the potential to improve communication and efficiency, several limitations hinder their effectiveness in reducing clinician pajama time:
- Complexity and Usability: Many patient engagement tools are complex and not user-friendly. Clinicians often spend more time navigating these systems than they would have spent on traditional methods of communication.
- Integration Issues: A lack of interoperability between different systems can lead to fragmented workflows. Clinicians may find themselves switching between multiple platforms, increasing the time spent on administrative tasks.
- Patient Overload: With the rise of patient engagement tools, clinicians may experience an influx of patient messages and requests. This can lead to increased administrative burdens rather than alleviating them.
Case Studies: Real-World Implications
To better understand the impact of patient engagement tools on pajama time, it is essential to examine real-world case studies that illustrate the challenges faced by clinicians.
Case Study 1: A Primary Care Practice
A primary care practice in a suburban area implemented a new patient portal to enhance communication with patients. Initially, the practice anticipated that the portal would reduce the number of phone calls and emails from patients, thereby decreasing the administrative burden on clinicians. However, the opposite occurred.
After the portal’s implementation, clinicians reported an increase in patient messages, many of which required detailed responses. The time spent addressing these messages during pajama time increased significantly, leading to higher levels of burnout among staff. The practice ultimately had to hire additional administrative support to manage the influx of patient inquiries, negating the intended efficiency gains.
Case Study 2: A Telehealth Initiative
Another healthcare organization launched a telehealth initiative aimed at improving access to care for patients in rural areas. While the initiative was successful in increasing patient engagement, it also resulted in longer hours for clinicians. Many providers found themselves working late into the night to accommodate patient appointments and complete necessary documentation.
The organization conducted a survey among its clinicians and found that 60% reported an increase in pajama time since the telehealth initiative’s launch. The organization recognized the need to reevaluate its workflows and provide additional support to clinicians to prevent burnout and maintain quality care.
Strategies for Reducing Pajama Time
Given the challenges associated with pajama time, healthcare organizations must explore strategies to mitigate this issue while still leveraging the benefits of patient engagement tools.
1. Streamlining Workflows
One of the most effective ways to reduce pajama time is to streamline workflows. This can be achieved through:
- Standardizing Processes: Establishing standardized processes for common tasks can help reduce variability and improve efficiency. For example, creating templates for common patient communications can save time.
- Training and Support: Providing comprehensive training for clinicians on how to effectively use patient engagement tools can enhance usability and reduce frustration.
- Utilizing Automation: Implementing automation for routine tasks, such as appointment reminders and follow-up messages, can free up clinician time for more complex patient interactions.
2. Enhancing Interoperability
Improving interoperability between different healthcare systems can significantly reduce the administrative burden on clinicians. This can be achieved through:
- Adopting Open Standards: Encouraging the use of open standards for data exchange can facilitate seamless communication between different systems, reducing the need for clinicians to switch between platforms.
- Investing in Integrated Solutions: Healthcare organizations should consider investing in integrated solutions that combine various functionalities into a single platform, minimizing the time spent on administrative tasks.
- Collaboration with Vendors: Engaging with technology vendors to address interoperability challenges can lead to more effective solutions tailored to the needs of clinicians.
3. Fostering a Supportive Work Environment
Creating a supportive work environment is crucial for reducing pajama time and preventing burnout among clinicians. Strategies include:
- Encouraging Work-Life Balance: Healthcare organizations should promote policies that encourage work-life balance, such as flexible scheduling and designated time for administrative tasks during regular working hours.
- Providing Mental Health Resources: Offering mental health resources and support for clinicians can help address the emotional toll of excessive pajama time.
- Recognizing and Rewarding Efforts: Acknowledging the hard work of clinicians and providing incentives for efficient practices can foster a positive work culture.
Conclusion: A Call to Action
The findings of the recent study highlight a critical issue in the healthcare industry: despite the implementation of patient engagement tools, clinicians continue to experience excessive pajama time. This phenomenon not only affects clinician well-being but also has significant implications for patient care and healthcare costs.
To address this issue, healthcare organizations must take proactive steps to streamline workflows, enhance interoperability, and foster a supportive work environment. By doing so, they can reduce the administrative burden on clinicians, improve job satisfaction, and ultimately enhance the quality of care provided to patients.
As the healthcare landscape continues to evolve, it is essential for stakeholders to prioritize the well-being of clinicians and recognize the importance of balancing technology with human-centered care. Only then can we create a sustainable healthcare system that benefits both providers and patients alike.