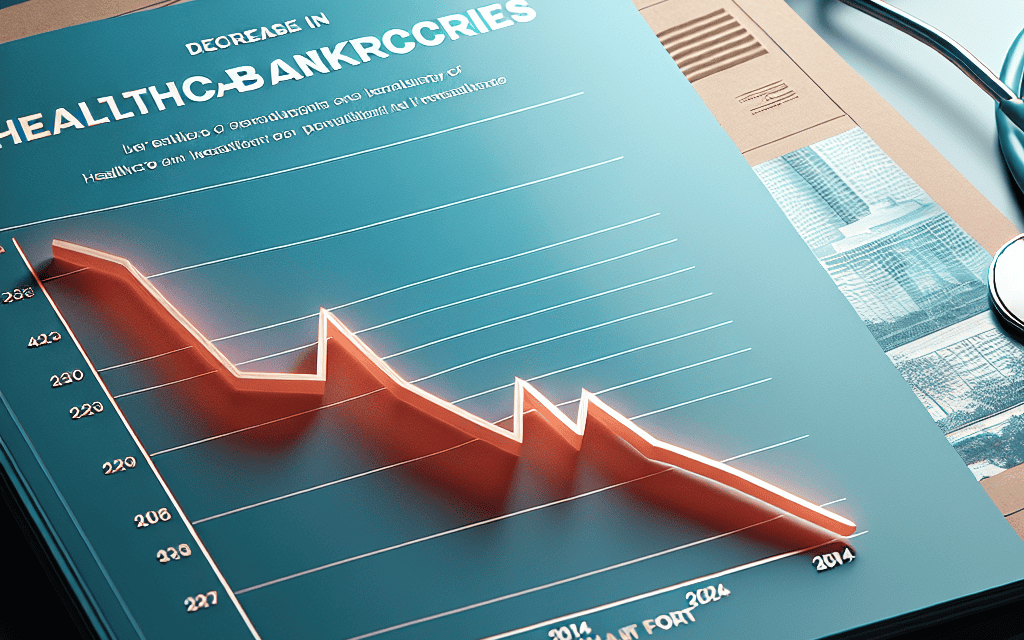
Healthcare Bankruptcies Decrease in 2024, According to Report
The healthcare industry has long been a cornerstone of the American economy, providing essential services to millions. However, it has also faced significant financial challenges, leading to a wave of bankruptcies in previous years. A recent report indicates a notable decrease in healthcare bankruptcies in 2024, suggesting a shift in the financial landscape of the sector. This article delves into the factors contributing to this decline, the implications for the healthcare system, and what the future may hold.
Understanding the Decline in Healthcare Bankruptcies
The decrease in healthcare bankruptcies in 2024 can be attributed to several interrelated factors. Understanding these factors is crucial for stakeholders in the healthcare industry, including providers, policymakers, and patients.
1. Economic Recovery Post-Pandemic
The COVID-19 pandemic had a profound impact on the healthcare sector, leading to unprecedented financial strain. However, as the economy has begun to recover, many healthcare providers have seen improvements in their financial health.
- Increased Patient Volume: As restrictions have eased and vaccination rates have increased, patient volumes have rebounded. Hospitals and clinics that faced financial difficulties during the pandemic are now experiencing a surge in demand for services.
- Government Support: Federal and state governments have provided substantial financial assistance to healthcare providers during the pandemic. Programs such as the Provider Relief Fund have helped stabilize many organizations, allowing them to avoid bankruptcy.
- Telehealth Expansion: The rapid adoption of telehealth services has opened new revenue streams for healthcare providers. This shift has allowed them to reach more patients and maintain continuity of care, contributing to financial stability.
As a result of these factors, many healthcare organizations that were on the brink of bankruptcy have managed to recover, leading to a decrease in overall bankruptcies in the sector.
2. Changes in Healthcare Policy
Healthcare policy changes at both the federal and state levels have played a significant role in shaping the financial landscape of the industry. These changes have aimed to improve access to care and reduce costs, ultimately benefiting healthcare providers.
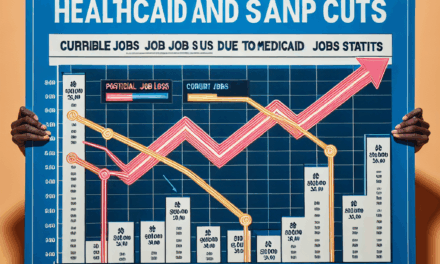
- Medicaid Expansion: Many states have expanded Medicaid under the Affordable Care Act, providing coverage to millions of low-income individuals. This expansion has increased revenue for hospitals and clinics that serve these populations, reducing the likelihood of bankruptcy.
- Value-Based Care Models: The shift towards value-based care has incentivized healthcare providers to focus on patient outcomes rather than the volume of services provided. This approach can lead to more efficient operations and improved financial performance.
- Regulatory Reforms: Streamlined regulations and reduced administrative burdens have allowed healthcare providers to operate more efficiently, reducing costs and improving profitability.
These policy changes have created a more favorable environment for healthcare providers, contributing to the decline in bankruptcies.
3. Financial Restructuring and Mergers
In response to financial challenges, many healthcare organizations have pursued restructuring strategies or mergers with other entities. These actions can provide the necessary capital and resources to stabilize operations.
- Bankruptcy Alternatives: Instead of filing for bankruptcy, some organizations have opted for financial restructuring, which allows them to renegotiate debts and improve their financial position without the stigma of bankruptcy.
- Mergers and Acquisitions: The trend of consolidation in the healthcare industry has continued, with many smaller providers merging with larger systems. This consolidation can lead to increased efficiencies and shared resources, reducing financial strain.
- Investment from Private Equity: Private equity firms have increasingly invested in healthcare organizations, providing the capital needed for growth and stability. This influx of investment can help prevent bankruptcies.
These strategies have allowed many healthcare providers to navigate financial challenges more effectively, contributing to the overall decrease in bankruptcies.
4. Technological Advancements
The integration of technology into healthcare has transformed the industry, leading to improved operational efficiencies and better patient outcomes. These advancements have also played a role in reducing bankruptcies.
- Electronic Health Records (EHR): The widespread adoption of EHR systems has streamlined administrative processes, reducing costs and improving billing accuracy. This efficiency can lead to increased revenue and decreased financial strain.
- Data Analytics: Healthcare organizations are increasingly using data analytics to identify trends, optimize operations, and improve patient care. This data-driven approach can enhance financial performance and reduce the risk of bankruptcy.
- Remote Monitoring Technologies: The rise of remote patient monitoring technologies has allowed providers to manage chronic conditions more effectively, reducing hospital readmissions and associated costs.
By leveraging technology, healthcare providers can enhance their financial stability and reduce the likelihood of bankruptcy.
5. Patient-Centric Care Models
The shift towards patient-centric care models has not only improved patient satisfaction but has also had positive financial implications for healthcare providers. This approach focuses on delivering high-quality care that meets the needs of patients.
- Improved Patient Engagement: Engaging patients in their care can lead to better health outcomes and increased loyalty. Satisfied patients are more likely to return for services, contributing to financial stability.
- Preventive Care Initiatives: Emphasizing preventive care can reduce the need for costly interventions down the line. By investing in preventive measures, healthcare providers can lower overall costs and improve their financial outlook.
- Community Partnerships: Collaborating with community organizations to address social determinants of health can improve population health and reduce healthcare costs, benefiting providers financially.
By prioritizing patient needs, healthcare organizations can enhance their financial performance and reduce the risk of bankruptcy.
The Implications of Decreased Bankruptcies
The decline in healthcare bankruptcies in 2024 has significant implications for various stakeholders in the healthcare system. Understanding these implications is essential for navigating the evolving landscape.
1. Improved Access to Care
As healthcare providers stabilize financially, patients can expect improved access to care. This improvement is crucial for ensuring that individuals receive timely and necessary medical services.
- Increased Service Offerings: Financially stable providers are more likely to expand their service offerings, including specialized care and preventive services.
- Geographic Accessibility: Providers that avoid bankruptcy can maintain or expand their facilities, ensuring that care is accessible to underserved populations.
- Continuity of Care: Patients benefit from continuity of care when providers remain financially viable, leading to better health outcomes.
Overall, decreased bankruptcies contribute to a more robust healthcare system that prioritizes patient access.
2. Economic Stability in Local Communities
Healthcare providers are often significant employers in their communities. The decline in bankruptcies can lead to greater economic stability in local areas.
- Job Retention: Financially stable healthcare organizations can retain jobs, providing employment opportunities for local residents.
- Economic Multiplier Effect: Healthcare providers contribute to the local economy through purchasing goods and services, creating a multiplier effect that benefits other businesses.
- Community Investment: Stable providers are more likely to invest in community health initiatives, further enhancing the economic well-being of the area.
The economic stability provided by a healthy healthcare sector is vital for the overall prosperity of communities.
3. Enhanced Quality of Care
With decreased financial pressures, healthcare providers can focus on improving the quality of care they deliver. This enhancement is essential for patient satisfaction and health outcomes.
- Investment in Staff Training: Financially stable organizations can invest in ongoing staff training and development, leading to improved patient care.
- Upgraded Facilities and Technology: Providers can allocate resources towards upgrading facilities and technology, enhancing the patient experience.
- Focus on Patient Safety: A stable financial environment allows providers to prioritize patient safety initiatives, reducing the risk of medical errors.
As a result, patients can expect higher quality care from providers that are not burdened by financial distress.
4. Strengthened Healthcare Systems
The decline in bankruptcies contributes to the overall strength of healthcare systems. A robust healthcare system is essential for addressing public health challenges and ensuring population health.
- Collaboration Among Providers: Financial stability encourages collaboration among healthcare providers, leading to integrated care models that improve patient outcomes.
- Resilience to Future Crises: A financially stable healthcare system is better equipped to respond to future public health crises, ensuring that care remains accessible during emergencies.
- Investment in Research and Innovation: Stable providers can invest in research and innovation, leading to advancements in medical treatments and technologies.
A strong healthcare system is essential for addressing the complex health needs of the population.
5. Future Challenges and Considerations
While the decrease in healthcare bankruptcies is a positive development, it is essential to remain vigilant about potential challenges that could arise in the future.
- Rising Operational Costs: Healthcare providers may face increasing operational costs, including labor and supply chain expenses, which could threaten financial stability.
- Regulatory Changes: Future changes in healthcare policy and regulations could impact the financial landscape, necessitating adaptability from providers.
- Market Competition: Increased competition among healthcare providers could lead to financial pressures, particularly for smaller organizations.
Addressing these challenges will be crucial for maintaining the positive trend of decreased bankruptcies in the healthcare sector.
Conclusion
The decrease in healthcare bankruptcies in 2024 is a promising development for the industry, reflecting a combination of economic recovery, policy changes, financial restructuring, technological advancements, and a focus on patient-centric care. This trend has significant implications for access to care, economic stability in communities, quality of care, and the overall strength of healthcare systems.
However, it is essential to remain aware of potential challenges that could threaten this progress. By addressing these challenges proactively, stakeholders in the healthcare industry can work towards sustaining the positive momentum and ensuring a resilient healthcare system for the future.
In summary, the decline in healthcare bankruptcies is a multifaceted issue that highlights the importance of adaptability and innovation in the face of changing economic and regulatory landscapes. As the healthcare sector continues to evolve, ongoing collaboration among providers, policymakers, and communities will be essential for fostering a sustainable and effective healthcare system.