-
Table of Contents
- Healthcare Accessibility: Bridging the Gap with Technology
- Telemedicine: Revolutionizing Remote Healthcare
- The Rise of Telemedicine
- Benefits of Telemedicine
- Challenges and Limitations
- Future Prospects
- Mobile Health Applications: Empowering Patients
- The Proliferation of mHealth Apps
- Benefits of mHealth Apps
- Challenges and Limitations
- Future Trends
- Electronic Health Records: Streamlining Healthcare Delivery
- The Adoption of EHRs
- Benefits of EHRs
Healthcare Accessibility: Bridging the Gap with Technology
In the 21st century, healthcare accessibility remains a significant challenge worldwide. Despite advancements in medical science, millions of people still struggle to access basic healthcare services. However, technology is emerging as a powerful tool to bridge this gap, offering innovative solutions to make healthcare more accessible, efficient, and equitable. This article explores how technology is transforming healthcare accessibility, examining various aspects such as telemedicine, mobile health applications, electronic health records, artificial intelligence, and wearable technology.
Telemedicine: Revolutionizing Remote Healthcare
Telemedicine has emerged as a game-changer in the healthcare industry, especially in remote and underserved areas. By leveraging telecommunications technology, telemedicine allows patients to consult healthcare professionals without the need for physical travel. This section delves into the impact of telemedicine on healthcare accessibility, its benefits, challenges, and future prospects.
The Rise of Telemedicine
Telemedicine has gained significant traction in recent years, driven by advancements in communication technology and the increasing demand for remote healthcare services. The COVID-19 pandemic further accelerated its adoption, as healthcare systems worldwide sought to minimize in-person interactions to curb the spread of the virus.
According to a report by McKinsey & Company, telehealth usage increased 38 times from the pre-COVID-19 baseline. This surge highlights the potential of telemedicine to transform healthcare delivery, making it more accessible to people in rural and underserved areas.
Benefits of Telemedicine
Telemedicine offers numerous benefits that contribute to improved healthcare accessibility:
- Convenience: Patients can access healthcare services from the comfort of their homes, eliminating the need for long commutes and reducing wait times.
- Cost-Effectiveness: Telemedicine reduces the cost of healthcare delivery by minimizing overhead expenses associated with physical facilities.
- Increased Reach: Healthcare providers can extend their services to remote and rural areas, where access to medical facilities is limited.
- Continuity of Care: Telemedicine enables continuous monitoring and follow-up care, improving patient outcomes and reducing hospital readmissions.
Challenges and Limitations
Despite its advantages, telemedicine faces several challenges that need to be addressed to maximize its potential:
- Technological Barriers: Limited access to high-speed internet and digital devices in rural areas can hinder the adoption of telemedicine.
- Regulatory Hurdles: Varying regulations across regions can complicate the implementation of telemedicine services.
- Privacy Concerns: Ensuring the security and confidentiality of patient data is crucial to maintaining trust in telemedicine.
Future Prospects
The future of telemedicine looks promising, with ongoing advancements in technology and increasing acceptance among patients and healthcare providers. Innovations such as virtual reality consultations and remote patient monitoring are expected to further enhance the capabilities of telemedicine, making it an integral part of the healthcare ecosystem.
Mobile Health Applications: Empowering Patients
Mobile health applications, or mHealth apps, are transforming the way individuals manage their health. These apps provide users with tools to monitor their health, access medical information, and connect with healthcare providers. This section explores the role of mHealth apps in improving healthcare accessibility, their benefits, challenges, and future trends.
The Proliferation of mHealth Apps
The proliferation of smartphones and mobile internet has paved the way for the rapid growth of mHealth apps. According to a report by Statista, there were over 350,000 mHealth apps available on major app stores as of 2021. These apps cater to a wide range of health needs, from fitness tracking to chronic disease management.
Benefits of mHealth Apps
mHealth apps offer several benefits that enhance healthcare accessibility:
- Self-Management: Users can track their health metrics, set goals, and receive personalized recommendations, empowering them to take charge of their health.
- Access to Information: mHealth apps provide users with access to reliable medical information, helping them make informed decisions about their health.
- Improved Communication: These apps facilitate communication between patients and healthcare providers, enabling timely consultations and follow-ups.
- Behavioral Change: mHealth apps use gamification and reminders to encourage healthy behaviors and adherence to treatment plans.
Challenges and Limitations
Despite their potential, mHealth apps face several challenges:
- Data Privacy: Ensuring the security of user data is a major concern, as mHealth apps often collect sensitive health information.
- User Engagement: Maintaining user engagement over time can be challenging, as users may lose interest or motivation.
- Regulatory Compliance: mHealth apps must comply with healthcare regulations, which can vary across regions and impact their development and deployment.
Future Trends
The future of mHealth apps is promising, with advancements in artificial intelligence and machine learning expected to enhance their capabilities. Personalized health recommendations, predictive analytics, and integration with wearable devices are some of the trends that will shape the future of mHealth apps, making them an essential tool for improving healthcare accessibility.
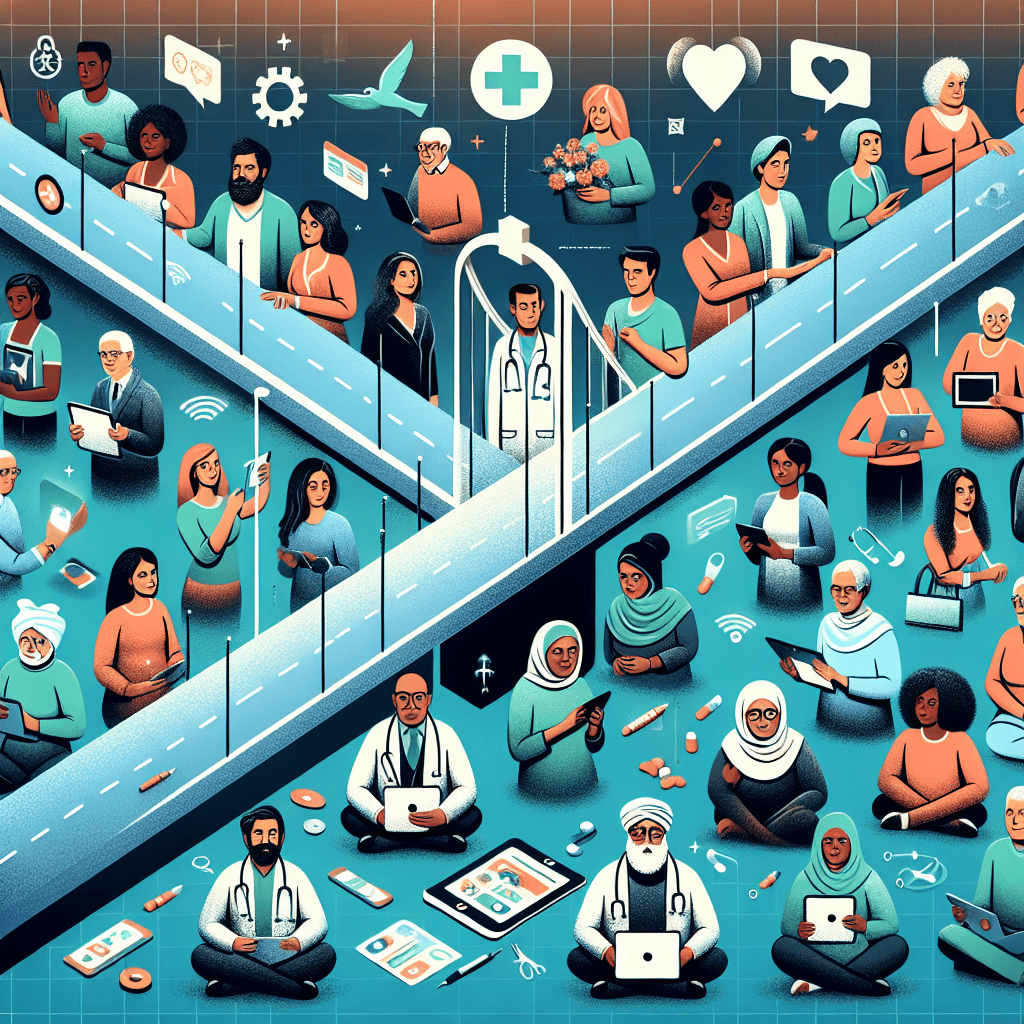
Electronic Health Records: Streamlining Healthcare Delivery
Electronic Health Records (EHRs) are digital versions of patients’ medical histories, providing a comprehensive view of their health information. EHRs play a crucial role in streamlining healthcare delivery, improving patient outcomes, and enhancing accessibility. This section examines the impact of EHRs on healthcare accessibility, their benefits, challenges, and future developments.
The Adoption of EHRs
The adoption of EHRs has been driven by the need for efficient healthcare delivery and improved patient care. According to the Office of the National Coordinator for Health Information Technology, nearly 86% of office-based physicians in the United States used EHRs as of 2017. This widespread adoption highlights the importance of EHRs in modern healthcare systems.
Benefits of EHRs
EHRs offer several benefits that contribute to improved healthcare accessibility:
- Comprehensive Patient Information: EHRs provide healthcare providers with a complete view of a patient’s medical history, enabling informed decision-making and personalized care.
- Improved Coordination: EHRs facilitate seamless communication and coordination among healthcare providers, reducing duplication of tests and