Essential Diagnostic Tools for Managing Chronic Pain

Chronic pain is a pervasive issue affecting millions of individuals worldwide, significantly impacting their quality of life and daily functioning. Effective management of chronic pain requires a comprehensive approach, beginning with accurate diagnosis. This article explores the essential diagnostic tools used in managing chronic pain, providing insights into their applications, benefits, and limitations. By understanding these tools, healthcare professionals can better tailor treatment plans to individual needs, ultimately improving patient outcomes.
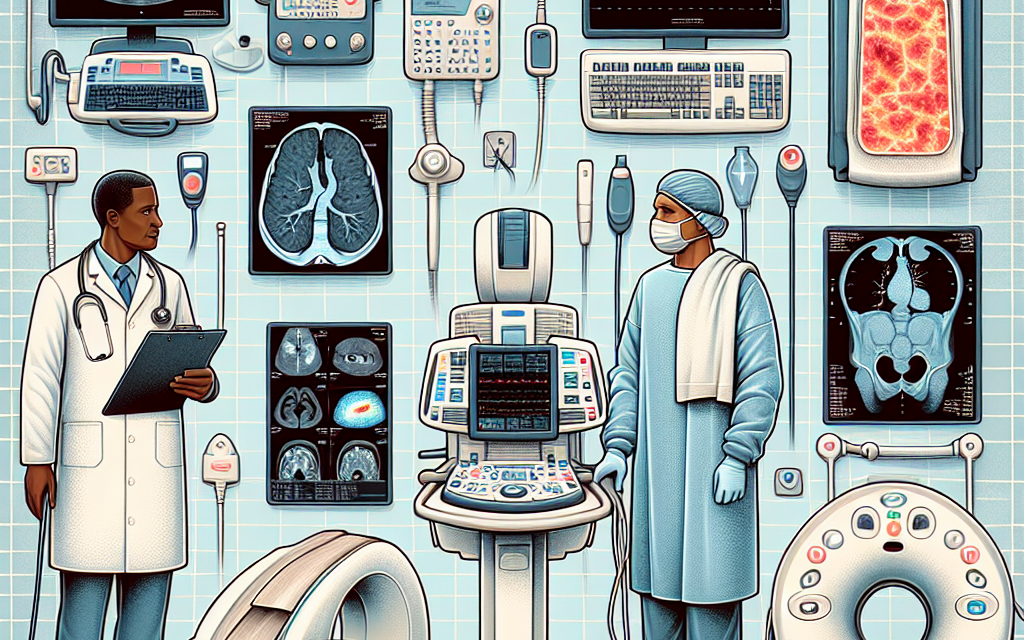
1. Imaging Techniques in Chronic Pain Diagnosis
Imaging techniques play a crucial role in diagnosing chronic pain, offering visual insights into the underlying causes of pain. These techniques help identify structural abnormalities, inflammation, and other factors contributing to chronic pain conditions.
1.1 Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) is a non-invasive imaging technique that uses powerful magnets and radio waves to create detailed images of the body’s internal structures. It is particularly useful in diagnosing chronic pain conditions related to soft tissues, such as muscles, ligaments, and nerves.
MRI is often employed to detect herniated discs, spinal stenosis, and other spinal abnormalities that may cause chronic back pain. It is also used to assess joint conditions like arthritis and soft tissue injuries. The high-resolution images provided by MRI allow for precise identification of abnormalities, aiding in the development of targeted treatment plans.
However, MRI has limitations, including high costs and limited availability in some regions. Additionally, it may not always correlate with the patient’s pain experience, as some abnormalities detected may not be the source of pain.
1.2 Computed Tomography (CT) Scans
Computed Tomography (CT) scans use X-rays to create cross-sectional images of the body. They are particularly effective in diagnosing bone-related issues, such as fractures or degenerative changes, that may contribute to chronic pain.
CT scans are often used in conjunction with other diagnostic tools to provide a comprehensive view of the affected area. For instance, in cases of chronic headaches, CT scans can help rule out structural causes like tumors or aneurysms.
While CT scans are valuable for their speed and ability to image bone structures, they expose patients to higher levels of radiation compared to other imaging techniques. Therefore, their use is typically reserved for cases where detailed bone imaging is necessary.
1.3 Ultrasound Imaging
Ultrasound imaging uses sound waves to produce images of soft tissues and organs. It is a versatile tool in diagnosing chronic pain, particularly in musculoskeletal conditions.
Ultrasound is often used to guide injections or aspirations in joints, tendons, and muscles, providing real-time visualization of the procedure. It is also employed in diagnosing conditions like tendonitis, bursitis, and nerve entrapments.
The advantages of ultrasound include its safety, as it does not involve radiation, and its ability to provide dynamic imaging, allowing for the assessment of structures in motion. However, its effectiveness is highly operator-dependent, requiring skilled technicians for accurate results.
2. Electrophysiological Studies
Electrophysiological studies are essential diagnostic tools for assessing the function of nerves and muscles. These studies help identify nerve damage or dysfunction, which can be a significant contributor to chronic pain.
2.1 Electromyography (EMG)
Electromyography (EMG) measures the electrical activity of muscles at rest and during contraction. It is used to diagnose conditions affecting the muscles and the nerves controlling them.
EMG is particularly useful in diagnosing conditions like carpal tunnel syndrome, peripheral neuropathy, and radiculopathy. By assessing the electrical activity of muscles, EMG can help determine whether muscle weakness or pain is due to nerve dysfunction or muscle pathology.
The procedure involves inserting a needle electrode into the muscle, which may cause discomfort. Despite this, EMG provides valuable information that can guide treatment decisions, such as the need for surgical intervention or physical therapy.
2.2 Nerve Conduction Studies (NCS)
Nerve Conduction Studies (NCS) measure the speed and strength of electrical signals traveling through nerves. They are often performed alongside EMG to provide a comprehensive assessment of nerve function.
NCS is used to diagnose conditions like neuropathies, nerve compressions, and demyelinating diseases. By evaluating the conduction velocity and amplitude of nerve signals, NCS can help pinpoint the location and severity of nerve damage.
While NCS is a valuable diagnostic tool, it may not detect all types of nerve damage, particularly small fiber neuropathies. Additionally, the procedure can be uncomfortable due to the electrical stimulation involved.
3. Laboratory Tests in Chronic Pain Diagnosis
Laboratory tests are an integral part of diagnosing chronic pain, helping to identify underlying medical conditions that may contribute to pain. These tests provide insights into inflammatory processes, autoimmune disorders, and metabolic abnormalities.
3.1 Blood Tests
Blood tests are commonly used to assess markers of inflammation, infection, and autoimmune activity. They can help diagnose conditions like rheumatoid arthritis, lupus, and fibromyalgia, which may present with chronic pain.
Common blood tests include the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), which indicate inflammation levels. Autoantibody tests, such as the antinuclear antibody (ANA) test, can help identify autoimmune disorders.
While blood tests provide valuable information, they are often used in conjunction with other diagnostic tools to confirm a diagnosis. Abnormal results may require further investigation to determine the exact cause of pain.
3.2 Urine Tests
Urine tests can provide insights into metabolic and renal conditions that may contribute to chronic pain. They are often used to assess kidney function and detect metabolic disorders like gout.
For instance, elevated levels of uric acid in urine may indicate gout, a condition characterized by painful joint inflammation. Urine tests can also help monitor the effectiveness of treatment for certain conditions, such as diabetes, which can cause neuropathic pain.
While urine tests are non-invasive and easy to perform, they may not provide definitive answers on their own. They are typically part of a broader diagnostic approach to chronic pain management.
4. Psychological Assessment in Chronic Pain Management
Chronic pain is not solely a physical experience; it often involves psychological and emotional components. Psychological assessment is crucial in understanding the impact of chronic pain on a patient’s mental health and overall well-being.
4.1 Pain Questionnaires and Inventories
Pain questionnaires and inventories are tools used to assess the intensity, quality, and impact of pain on a patient’s life. They provide valuable insights into the subjective experience of pain, helping healthcare providers tailor treatment plans.
Commonly used questionnaires include the McGill Pain Questionnaire, which assesses the sensory and affective dimensions of pain, and the Brief Pain Inventory, which evaluates pain severity and its interference with daily activities.
These tools help identify patterns and triggers of pain, as well as the effectiveness of current treatments. They also facilitate communication between patients and healthcare providers, ensuring a comprehensive understanding of the patient’s pain experience.
4.2 Psychological Evaluations
Psychological evaluations assess the mental health status of patients with chronic pain, identifying conditions like depression, anxiety, and post-traumatic stress disorder (PTSD) that may exacerbate pain.
These evaluations often involve interviews and standardized tests, such as the Beck Depression Inventory or the State-Trait Anxiety Inventory. By identifying psychological factors contributing to pain, healthcare providers can incorporate appropriate interventions, such as cognitive-behavioral therapy (CBT) or mindfulness-based stress reduction (MBSR).
Addressing psychological aspects of chronic pain is essential for holistic management, as untreated mental health issues can hinder the effectiveness of physical treatments and prolong the pain experience.
5. Functional Assessment Tools
Functional assessment tools evaluate the impact of chronic pain on a patient’s physical abilities and daily functioning. These assessments help determine the extent of disability and guide rehabilitation efforts.
5.1 Functional Capacity Evaluations (FCE)
Functional Capacity Evaluations (FCE) assess a patient’s ability to perform work-related tasks and activities of daily living. They provide objective data on physical capabilities, helping to determine appropriate work accommodations or disability status.
FCEs involve a series of standardized tests that evaluate strength, endurance, flexibility, and coordination. They are often used in occupational health settings to assess the impact of chronic pain on work performance.
While FCEs provide valuable information, they require skilled evaluators and may not fully capture the fluctuating nature of chronic pain. They are best used as part of a comprehensive assessment strategy.
5.2 Gait and Movement Analysis
Gait and movement analysis assess the impact of chronic pain on a patient’s mobility and movement patterns. These assessments help identify compensatory movements and biomechanical abnormalities that may contribute to pain.
Gait analysis involves observing and measuring parameters like stride length, speed, and joint angles during walking. It is often used in patients with chronic lower limb pain or back pain to identify movement dysfunctions.
Movement analysis can also be applied to specific activities, such as lifting or reaching, to assess functional limitations. By identifying movement abnormalities, healthcare providers can develop targeted rehabilitation programs to improve mobility and reduce pain.
Conclusion
Effective management of chronic pain requires a comprehensive diagnostic approach that incorporates various tools and assessments. Imaging techniques, electrophysiological studies, laboratory tests, psychological assessments, and functional evaluations each play a vital role in understanding the complex nature of chronic pain.
By utilizing these diagnostic tools, healthcare providers can develop personalized treatment plans that address the physical, psychological, and functional aspects of chronic pain. This holistic approach not only improves patient outcomes but also enhances their quality of life.
As research and technology continue to advance, new diagnostic tools and techniques will emerge, further enhancing our ability to manage chronic pain effectively. Staying informed about these developments is essential for healthcare professionals dedicated to improving the lives of individuals living with chronic pain.